What prevents us from being the doctors we always imagined? We enter medicine as inspired, intelligent, compassionate humanitarians. Soon we’re cynical and exhausted. How did all these totally amazing and high-functioning people get screwed up so fast? Attention: med students and doctors: It’s not your fault. Here’s why you are suffering and what you can do about it.
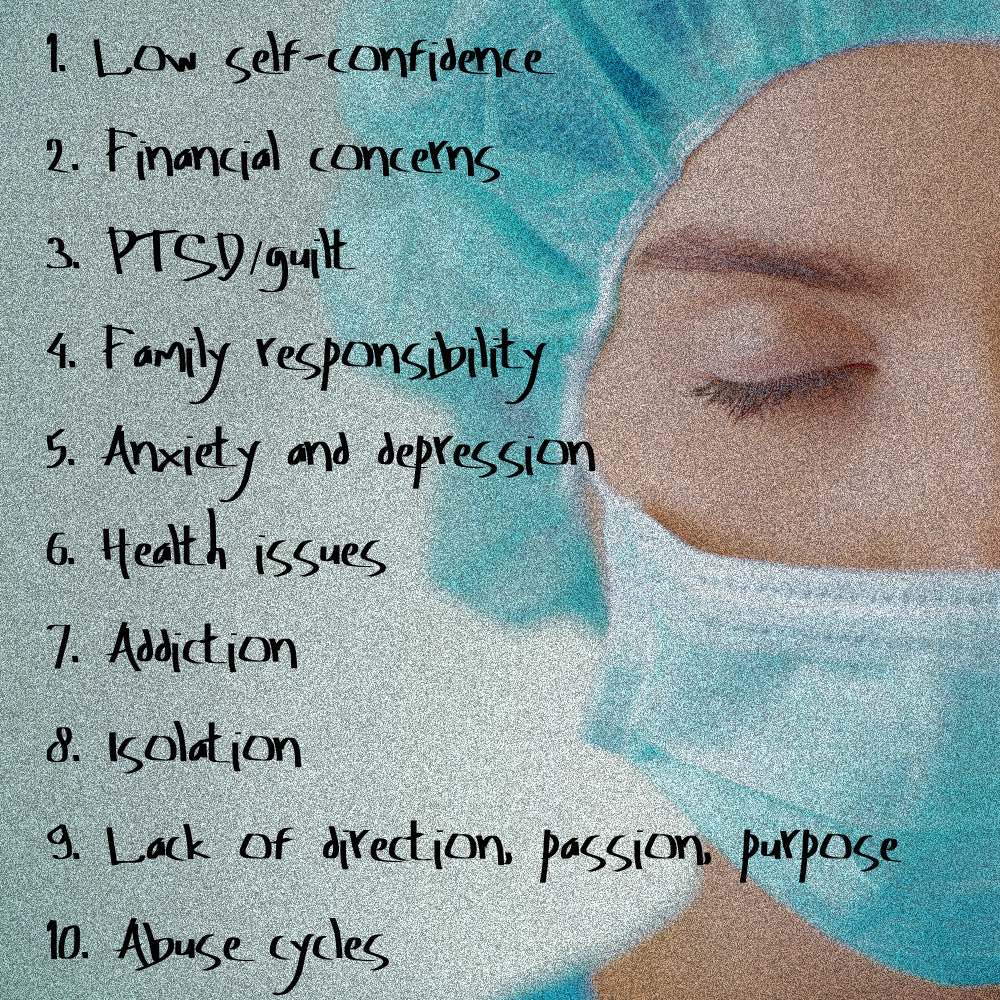
Top 10 fears that hold doctors back: 1. Low self-confidence 2. Financial concerns 3. PTSD/guilt 4. Family responsibility 5. Anxiety and depression 6. Health issues 7. Addiction 8. Isolation 9. Lack of direction, passion, purpose 10. Abuse cycles. (Listen to podcast for complete analysis)
Top 5 warning signs you lack self-confidence (and how to get it back)
1) Confusion—fear of not knowing. What if I don’t know what’s wrong with the patient? What if I’m not smart enough to figure it out? Fear of not knowing is often rooted in traumatic med school or residency training. If you’ve managed to get through training without self-doubt, it can develop in toxic/dysfunctional work environments. ANTIDOTE: CLARITY.
2) Perfectionism—Fear of mistakes. Perfectionism is a major issue for many physicians and health care professionals. We take our jobs very seriously and know that getting it wrong can have far-reaching devastating results. Wanting to get it right at our own expense leads to obsessing, overworking, lack of balance. These behaviors deplete our self-confidence. ANTIDOTE: ACCEPT YOUR HUMANITY.
3) Trauma/PTSD. Working in the field of medicine often triggers old trauma and PTSD. Acknowledging and healing our trauma has to happen in order to build self-confidence. ANTIDOTE: CHOOSE OPPORTUNITIES TO HEAL YOURSELF.
4) Destructive beliefs. Choosing stress as a belief and lifestyle has devastating consequences. “I have chosen a stress-filled profession and therefore I will live a stress-filled life,” is distorted, destructive thinking. Fueling the stress in our lives only erodes our self-confidence. What we focus on grows. ANTIDOTE: IDENTIFY YOUR POSITIVE BELIEF SYSTEM.
5) Losing your sense of purpose. There was a time when you entered medicine inspired by a vision or passion. You had a dream. You had a sense of purpose. Now, these many months and years later, you are lost. Jaded by all you have been through, you no longer easily connect with what you are here to do and have begun to doubt yourself. ANTIDOTE: CONNECT WITH YOUR PURPOSE, YOUR DREAM, YOUR REASON FOR BEING HERE.
YOUR PATIENTS NEED 1) To Be Seen, 2) To Be Heard, 3) To Feel Safe, 4) To Feel Connected.











As a retired RN I can say that these fears are not just felt by MDs.
Absolutely. They apply to all health professionals to various degrees.
– Apprehensions do appear in my mind daily – – not because I lack confidence – and not because I am not well-enough informed to deliver and provide excellent patient care – – but because I don’t fit into the environment of the group practice – – what does one do ?
Find a new group. Find your tribe. Go solo. There are many many options for you that may not be apparent at first glance. It is tough to see all our possibilities when we are mired in what’s not working. Do you have a good mentor?
AMazing episode Pamela! I really resonate with being a healer, getting back to my initial reasons of being a doctor, etc. I am an anesthesiologist and I don’t want to quit the place where I work – I actually would like to change things around here towards “ideal medical care”, but my colleagues don’t seem to care/don’t have time/not interested and some of them seem miserable and I do feel I could help (them and myself). I do wonder if this is the best path – thoughts?
Be the change. Never doubt the power of one person. You can do it. Set the example.
Excellent!! I have nurses and doctors reach out to me all the time because they fear taking the steps necessary to leave a toxic environment. Sometimes, the steps are clear and legal advice is not necessary, yet they need to hear that they are not weak or unreasonable and will be okay. More times than not, they are and have nothing but good things to say about their new job. I can identify one or more of these fears in each one of my clients. The most common theme is that they’ve accepted their environment as the status quo. Every place will be the same. IT WILL NOT!!! They often fear saying ‘no’ to an unreasonable schedules or unsafe amount of patients, even when they would not be in breach of their contract. It is ironic that what makes them a good doctor also makes them so vulnerable to abuse. Lack of confidence or the drive to be perfect makes them think they have less power or say than they really do. I have always applauded Dr. Wible’s dedication to raising awareness and bringing about change in the healthcare industry. It is an uphill battle as doctors who cannot empathize with the struggle often tell me it’s the doctor’s fault, they were not cutout for the profession, those doctors had issues beforehand that were just exacerbated by their inability to handle stress, or that the abuse and exploitative training is necessary for patient safety. It’s like they were brainwashed to believe this to be true, which often leads to the cycle of abuse. I was in healthcare management for 4 years and I know this not to be true. There are plenty of places that do not succumb to these tactics and are just, if not more, efficient and effective than those who do. Great podcast!!
A doctor can’t be a victim and a healer at the same time. Time to stop the self-neglect and self-abuse. Brainwashing is exactly what this is. Mind control. Pure and simple.
I estimate that 99% of all physicians are brainwashed. Way I’ll be a little more gentler 97%. Most all physicians believe that removing skeleton, body parts, tissues is the correct balance inhumane way to treat physical pain. It’s not.
Physical pain will fully benefit from physical therapy.
Think muscles, think football, the massage, think rehab the restoration.
If you think or act with a knife or drugs you just betray the laws of nature and the human body.
Our mission is exactly the same, yet I find it difficult to break 98% of physicians out of the brain training to do harm to their patients.
Without uprooting the seeds of our own destruction, nothing good to happen for loooooooooooong time.
99% of all physicians are brainwashed. We are indoctrinated into a one-size-fits-all assembly-line mentality that funnels us into big-box clinics. (as one example)
Fear of loss is a powerful force for good or evil. Physicians are social servants who should be in the front of the battle witnessing with good, not so good, what needs to improve and evil in real-time to make the navigation corrections.
There is no single person, organization, group our society who is protecting the integrity of science and humanity. Our healthcare system has gone renegade.
The unholy Trinity, AMA, Wall Street and lobbyist have infected federal policies and procedures. This unholy Trinity has also placed in carrots and sticks. The carrots are sweet which will allow an Honorable soul to dishonor a wounded soul. The stick is huge and powerful everyone fears it because they see their colleagues get smashed by it being disrespected by their other colleagues.
This iteration of healthcare set in motion by sinister seeds requires chaos flesh, blood bones to keep it alive. It has become autonomous just like in the Matrix using injured and wounded souls as batteries.
Probably higher than 99%. They can’t even think for themselves. I hear my peers repeat (word-for-word) things that lecturers have said all the time as if it as a niche opinion they synthesised themselves. We need more critical thinking, but the teaching trains as to be subordinate to big organisations and pharmaceutical companies, or risk having our licenses removed.
Part of being in survival mode (and sleep deprived) = brain doesn’t work right. These people were thinkers before they were starved for food, sleep, emotional comfort and now scared shitless. You need time to think clearly. Plus sleep, food . . . stuff like that . . .
oops balanced correct and humane way to treat physical pain. NO!
This lie, fallacy, definition deception, and misinformation will go down in history as the worst human on human betrayal by physicians who should know better.
The frightening part no one seems to be able to break free from thought that the earth is truly wrong even though from our perspective it seems flat.
Hi what type of physician is your friend?
A counselor who specializes in medical students and physicians.
Wow, I just have a complete case of Imposter Syndrome and had never heard of it before reading this article! Like you, I don’t feel I deserve to be a physician and it actually makes me feel uncomfortable when others put me on the “medical student” pedestal which assumes I have supreme knowledge of the human body and organisational skills. In reality, I feel I know little and my life is a bit of a mess. In my first year, I maintained a good social life but my grades suffered and I only just passed. This year, I’m doing a lot better (and by that, I mean average in the class rank), but it’s at the expense of maintaining any sort of hobby or outside interest. In fact, I don’t even have enough time to exercise because I’m in classes, clinics, labs or the library all day and choose to relax in the small few minute breaks I get each day. My health is suffering. If it wasn’t for the holidays, I wouldn’t be able to do it. I am quite a reflective and philosophical type, so I am not suited to all of the bitchiness, social-climbing and backstabbing which takes place amongst med students. As a result, I have few friends in medicine and to be honest, enjoy it that way. Patients are going to suffer too. It’s very hard to be compassionate when you’re in such a punishing environment. I remember when we were learning venipuncture, the nurse was explaining how to make it more comfortable for patients as many can find it a painful experience. My thoughts were: “Gee- pain from a needle is NOTHING compared to having to endure medical school! I wish that was my only concern!” This is a dangerous pattern of thought, but I consciously correct myself when I make these assumptions. I just wish I could reconnect with my heart, but it is hard to find the time with the insanity of our workloads.
Best of luck! I’m thinking of you.
Also Pamela, you made me laugh when you mentioned friendships centring around shared traumas because it’s so true! Those whom I’m closest to have the same gripes as me, and our relationships are built on this shaky foundation.
Dear Dr. Pamela your dream about ideal clinic and the fact that you are encouraging and helping others in this direction are amazing. Thank you.
While undergoing training in US hospitals I found one heart braking statistic number : every summer season when intern residents are starting their residency there are increase in mortality of the hospital (4-8-10 %) from 100 patients admitted and treated in this period 4-6-10 people will die… It is tragic reality for residents and patients…I saw intern residents stigmatized for all their life
in this way… it is one of the most difficult periods transition from medical student to intern doctor… in this first couple of months something has to be done to help new doctors to prevent the possible mistakes… to improve this number…most common mistakes are drug to drug or drug to disease or drug to patient interaction… a lot of patient in admissions are on long list of medications adding new ones on this list only makes risk interactions and possible side effects for patients higher and sometimes unpredictible…if in every admission or treatment plan created by intern resident in the system automatically could be created drug to drug , drug to disease and drug to patient (age, race, chronic conditions…) control checklist created by computer it could help…
it could save time and life…and I am sure that if someone will have the courage to open this taboo topic more ideas can be created for improving of this number…may creating the position of advisor senior doctor with only one responsibility to help interns and protect them from possible mistakes in the first couple of months in beginning could help? I think that first months of residency training are creating most trauma and PTSD among new doctors…
Great ideas and so much can be done to make the transition from medical student to doctor safer for all. Instead the ACGME just extended work hour shifts from 16 to 28 hours. Certain to worsen care all around. Just got off the phone with the mom of an intern who is so distressed because her son called her nearly incoherent because he had not slept and he feels worried that he may harm someone.
Dr Rodriguez, this is a very thought provoking historical perspective. I would guess you are not an ORTHO guy, but would find it refreshing if you are!
Anyway I’d like to look deeper into this historical information and am particularly interested in the basis of muscle-derived pain and the logical and more appropriate (non-surgical) treatment of it. Please refer me to a summarized references to this approach, as I am now leaning more and more towards the non-invasive, more natural-based approaches to wellness and healing and am always seeking solid supportive evidence.
“Wounded people with stress as a belief system”. Little wonder why medicine is so ridiculously toxic. I don’t understand why we in medicine are all not on the rooftop shouting about the injustice of it all??? How can we make the LCME, ACGME make this information a mandatory part of medical education so that we can save medicine??? Thank you Pam for the work that you are doing. In retrospect, I don’t know how I survived 30 years in academic medicine as a liver transplant surgeon, but I think that I can be a valuable asset in the process of healing medicine!!!! This podcast has helped produce clarity for me. Thank you.
This was so so so so helpful to hear.
“You are a human being. You are NOT a robot.” I honestly should tattoo this on my wrist to remind myself constantly of this fact.
I feel the constant push to be better, to be smarter, to keep up with the best of the best in my class who have a much more extensive science background than I do, to get the right answer when the boys in my small group sessions pimp me with questions about things I’ve never even heard of, to “only need 4 weeks before step 1” because “why would anyone need to use the 2 extra weeks to study, shouldn’t you already know all this stuff?”
I feel so stupid sometimes. Listening to this podcast makes me realize that my imposter syndrome is legitimate and that I am not the only one who feels this way.
Signed,
a baby M2
What do u mean by clarity?