
Dear Pamela,
I just worked 36 hours in 3 days. Stick a fork in me. Must have seen close to 200 patients [in the emergency department] and picked up a nasty head cold from one of them. My throat feels like sandpaper and my mouth feels like the bottom of a birdcage. Last case was a 21-year-old asthmatic. All hands on deck—balls to the wall, IV, meds, monitors—the works in 10 minutes while trying to comfort her terrified mother at the foot of the gurney. Halfway into the epi and magnesium the gal sits bolt upright, screams with a high-pitched squeak, claps her hands 4 times over her head, goes out, bradys down to 30 and pukes all over her own face. Fuck me sideways. Direct laryngoscopy is a wash, as is Glidescope—too much shit, peas and potatoes pouring out of her mouth. Fuck, fuck, fuck. Cram an LMA in—nothing. Wait—let me wiggle it just a little—holy shit—the ETCO2 just turned a beautiful shade of egg yolk yellow. Sats improving, heart rate 38…42…50…66. I think it’s gonna be Ok. I’m not letting go of this fucking tube—anesthesia has to pry my fingers off it in order to work their bullshit with whatever magical fucking tools they use to swap out the LMA for an ET tube. I’m shaking and sweating and I think I might have peed myself a little. I’m weak and my ears are ringing and I’m not hearing anything anyone is saying. I see the mom sitting alone in a chair squeezing her bible and mouthing a prayer. I sit down next to her, hold her hand and thank her for her prayers. I tell her the honest truth—it was touch and go for a few minutes, but things are ok now and I honestly, truly believe it was her prayers that enabled us to do what we did. I thank her again. She thanks me. We hug for just a second and I leave before I start to cry. Came this-god-damn-close to a goddam dead 21 year old. Now she is going to live and hopefully have many, many more opportunities to eat dinner and laugh and love and pray with her mother. Don’t talk to me about fucking resilience.
I’m so tired.
Jerry
* * *
Poor Jerry.
He’s so angry.
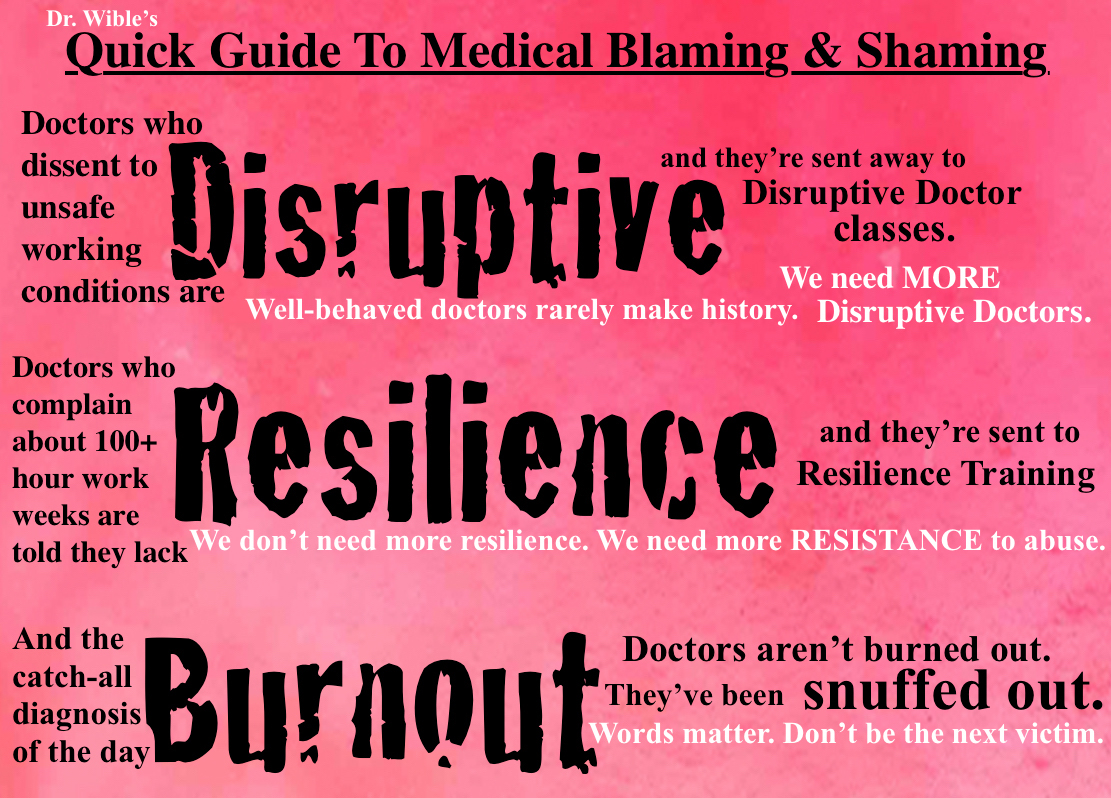
How inappropriate. I hope he doesn’t get in trouble for being a “disruptive” physician.
Maybe he’s just “burned out.”
Maybe Jerry needs to read a book on “work-life balance.”
Or take deep breaths.
Or sign up for a yoga class.
Or . . .
Maybe Jerry isn’t the problem.
Maybe we should stop labeling, blaming, and shaming doctors like Jerry.
Jerry seems like a pretty fucking amazing doctor to me.
What do you think?
Pamela Wible, M.D., is a family physician who helps physicians recover from being overworked, shamed, and blamed. She offers biannual physician retreats and is the author of the best seller Physician Suicide Letters—Answered. Dr. Wible has been named the 2015 Woman Leader in Medicine for her pioneering contributions to medical student/physician suicide prevention.














I completely understand, Jerry. Resilience is not the training we need. Empathy from the administration , a break from the dictatorial pattern of business owners and a weekend off too. I boycotted the world of slavery for two years and now I am happy. So grateful that I continue to live in a simple way so I don’t have huge monthly expenses requiring me to go back to work. You are not alone. It is important that our voice is heard.
Jerry is a “pretty fucking amazing doctor”. 100%
How can I move to allow doctors eight hour shifts instead of the rudimentary twelve? Will this be shot down as in times past?
I’m a medical records technician and would love to sit and converse with any physician any where. Listening is what I enjoy most.
Speak up Ryan. It is a public health issue. Patient safety. Please read what happens when we abuse those whom we need to care for us: http://www.amazon.com/Physician-Suicide-Letters-Answered-Pamela/dp/0985710322/ref=asap_bc?ie=UTF8
Also Ryan – just reach out and be nice to docs. We’re just normal people in a high-stress job.
Jerry, of course isn’t the problem. The problem is that doctors like him aren’t rewarded or supported adequately. Even if he survives his training spiritually, he is unprepared to deal with the modern challenges of medical practice. He will be pushed into some large medical practice or hospital system to act hike a small cog on a large wheel. Residents need to believe that they can be independent, happy, fulfilled agents of change.Medicine is a privilege, a passion and a calling. We can never forget this. We must revere , support and embrace those that devote their lives to heal others. Just look in the mirror before you disparage your fellow doctor, young or old. I’m assuming he is in residency. If not, my thoughts I feel still resonate for those enslaved spiritually in institutional prisons( hospitals).
I don’t believe he is in residency.
I love Jerry’s bad words. I was like “HELL YEAH”! TAKE THAT!
I knew you’d approve. 5 out of 5 doctors would approve of Jerry’s words.
Dear Jerry,
If you check in here to read these comments-just know we all think you did an incredible job saving that girls life. Of course, you know-it doesn’t always end in such a happy ending. Once, a long time ago, I was a nurse with a bad cold-went to the ER in a highly respected Academic ER three times-sent away each time with a “give it time” advise. The ER doctor was a surgical resident that was so tired his eyes were glazed over, and he looked like a zombie to me. The third time-I grabbed the sleeve on the nurse practitioner-who was telling me I was being released, again. When I grabbed the sleeve of her white coat-she whipped around and faced me-her eyes finally focused on me lying down on the stretcher. I realized this would be my only shot of actually saving my own life. I gave her the low-down: went through the symptoms no one bothered to ask me about, and let her know that I was dangerously ill, and needed someone else to “take another look”.
She heard me-and grabbed my arm, and said she had an idea-she called a fellow from the ID department, who saved my life. I had mycoplasma pneumonia-and the penicillin I had been taking would never work on me. He did a cold agglutin test-right there-while I was on the stretcher. Once he saw my blood clotting-he made the proper diagnosis. I was admitted, and sent to ICU, and after 10 days-I pulled through.
It was that experience that lead me to leave nursing and study medicine. Essentially-the crappy care I received from this “highly
valued academic hospital” allowed me to realize that I could do a better job then most of the doctors who treated me-both in the unit and on the medical floor. By the way-it was the first week of July-and every doctor I encountered was scared and numb. They “looked great” but they were mean and uncaring-and clearly just “winging it”, And the I.D. fellow who made the diagnosis-was actually from Canada.
You did a great job-but you probably already know-you are a rare breed. Don’t EVER leave medicine. We really need you.
with my love and admiration,
another physician
After 25 years of ER I totally hear you Jerry and even though I don’t know you, I love you for what you do. Love you too Pamela. I know what it’s like to be one of those disruptive doctors (up here in Canada where we live with rationed care) watching my patient suffer for no good reason except the next level of care won’t take her.
I was fighting this battle 25 years ago when I sent a junior resident who suffered a corneal abrasion during a night of call home in the morning. We are are not immune to injury and illness. Keep the fight going Pamela.
Jerry did an incredible job. I understand that kind of tired. You just keep going because the patient is the main thing. I have no doubt that Mother appreciated everything Jerry did. Its scary.
In the last year Ive gone from an outpatient practice with a 3000 patient panel and no time to do the work. they asked you to do more and more. My salary was decreased for a year by $30,000. My work ethic never changed. I started working more to make up. I was spending off days doing office work. When my family was visiting for vacation, I was calling patients.
I worked as a nocturnist at a hospital. They would schedule you for 10 shifts in a row at night. The 3-4 doctors during the day and one at night. No sign out on the patients , so if it wasn’t for the nurses and respiratory, I would have no clue as to what was going on with the patients. The medical director and the administration thought this was okay for patient safety. They didn’t care about my safety. Sometime I had so much work to do I didnt leave the hospital until after the next shift .
I decided to try urgent care. Which is where I am right now. I find it to be a different kind of abuse . Scolded for not seeing people within a certain time frame and talked to by administration. about every negative YELP review. the review usually comes after 8 hours or no food or bathroom breaks. You stay until the work gets done. I took the job because I was told I would only work three days a week and after I explained the hospitalist craziness, was told , ” Oh we would never treat our doctors like that.”
Whenever I have gone to admin and voiced my concerns, I was labeled as a complainer. been told that I just dont fit in. People cant understand how I went from a chief resident with so much potential to someone searching for the right place.
Ive turned in my resignation, end of March Im out . Not sure whats going to happen , but luckily Im in a place where I feel Im more important. My mind and my heart wont continue to let me give what I consider substandard care because of the constraints a job put me in . all of my patients have told me they appreciate me. Thats enough for me. Im praying I know how to get to the good place
Jerry is a hero! If we are even going to have a thing called resiliency training, then Jerry could teach it.
Thank you Jerry for your service to humankind. The description of the time you took with the mother, of recognizing her humanity, that warmed my heart. I hope it was a tiny bit of healing for your tender heart as well. May you find what you need to be whole and to continue your great work in the world.
I totally agree with you! Jerry was beyond fatigued, sick and had adrenaline coursing through his system when it appeared that the patient wasn’t going to make it. He did the best thing for himself when we went to the Patient’s Mother, held her hand and was able to tell her that her daughter would live, and acknowledged the Mother’s religious belief. All of these things let us know that Jerry is operating very well, but what his words tells us, is that he feels beyond psychologically fatigued. When someone like Jerry works so hard and so well, yet feels no success, it’s because of the prevailing attitude of the Corporation. The corporation pays what the market bears and has taken the “Doctoring” out of it. Jerry’s sense of being the one who “saved” the patient wasn’t enough, because of overwork, fatigued and being sick.
What do you think corporations should do? How should they treat physicians? What should we require of our employers in regard to safe working conditions for patients—and physicians?
How should corporations treat physicians?
Fairly…and create supportive work environment.
Like:
Work day should not be longer than 8-10 hours- and working past 10 hours was found to increase risk of MI and heart disease. My heart is no exception because I am a physician. Working during the day and then being on phone call at home and again working next day is insane- no human can do this and not get sick. This is just reality.
I can provide proper detailed human care to 12- maybe 15 patient a day, so asking me to see 35 same day is insanity. Asking me to see 35 patients a day 5 times a week and then spend my “weekend off” getting close to 40 calls on my phone from patients to answer and… working another week again is even more nuts! But unfortunately it is a reality for many physicians, and it is even worse sometimes for nurses, especially those working in hospital- they are asked to care for way too many patients.
Pamela, did you ever read this article: “How To Discourage a Doctor” by Richard Gunderman- try to google it I do not know how to insert link into email, sorry…
Katarzyna
Yes. I know that one. Here is another way to discourage doctors: https://www.idealmedicalcare.org/blog/doctors-not-allowed-to-ask-patients-how-are-you/ (tell them they can’t ask patients, “How are you?”) !!!!!?????
We need more doctors like Jerry. <3
Hello, Jerry: I appreciate you being straightforward- few have the guts to describe situation as it really is. Doing your job is like being in the line of fire every day- your body likely reacts in the same way like the one of a soldier in active combat zone. It takes days to recover from that degree of stress- all because you are human and not Robocop!
You do not have days to recover- but do 12 hour shifts one after another instead. It is like abusive marriage situation- breaks down everyone eventually, the only difference is how long it takes. It is a job with expiration day on it- and when doctors finally say “I had enough” they are told they are not resilient enough… or not dedicated enough… or blamed for considering part time positions.
I am simply glad there are still folks like you out there- makes me want to stay in my own job (not ER, just outpatient- quite different type of front-line :))
Katarzyna
Thanks Jerry all who have worked high intensity ER long enoughknow the feeling you were Great
I’m a physician who went through training with two children as a single mother &was grumpy the whole time
I am not a doctor. I deeply believe in the power of prayer. I want to thank Jerry for reaching out to that mother, for recognizing and appreciating the power of her prayers, and hugging her. A couple of years ago I visited a highly recommended oral surgeon to do root canal surgery for my autistic stepson. The regular dentist felt the tooth could be saved, but the oral surgeon was gruff, rude and angry, said he would try, but thought the tooth was unsavable. I was allowed to sit in the doorway where I could watch the doctor work on my stepson. I prayed fervently (silently)the whole time, at first feeling very discouraged, but eventually feeling somewhat better. It was more than an hour, and the doctor said nothing during that time, other than directions to his assistant. After more than an hour of intense prayer, I suddenly felt relieved and inspired, so grateful to God. I knew clearly that everything was okay! I then looked at the doctor, and he seemed more relaxed. His vocal tone had changed also. In a few minutes he looked up at me, and said cheerfully, “Everything looks good!” I answered, “I know. I’ve been praying.” He looked at me in disbelief like I was from another planet. he obviously thought I was crazy.
Carrying capacity?