
Today the ACGME (Accreditation Council for Graduate Medical Education) made the reckless decision to increase work hours to 28-hour shifts for new doctors. Here are the catastrophic consequences of their decision. Here are actual quotes from physicians (de-identified with some patient details changed to protect confidentiality):
“I did my internship in internal medicine and residency in neurology before laws existed to regulate resident hours. My first 2 years were extremely brutal, working 110 – 120 hours/week, and up to 40 hours straight. I got to witness colleagues collapse unconscious in the hallway during rounds, and I recall once falling asleep in the bed of an elderly comatose woman while trying to start an IV on her in the wee hours of the morning.”
“I ran a red light driving home in residency after a 36 hour shift. Got pulled over. It was sobering: I was not fit to use my driver’s license, but I had just been using my MEDICAL license for over a day non-stop!”
“I have made numerous medication errors from being over tired. I also more recently misread an EKG because I was so tired I literally couldn’t see straight. She actually had a subarachnoid hemorrhage and by misreading the EKG I spent too much time on her heart and didn’t whisk her back to CT when she came in code blue. She died.”
“After a 36-hour shift, I fell asleep and began dreaming while walking home—repeatedly. It was a four-block walk.”
“I fell asleep multiple times at the light at the intersection right at my neighborhood after call. I would see home was close and relax just enough. I had a baby and I was so afraid of forgetting him in the back seat if I ever had him with me I would put his bag in the front with me and my stuff in the back with him. Luckily, nothing bad happened in either situation but I just got lucky.”
“As a resident in a surgical specialty, my program routinely violated work hours, yet our attending physicians kept talking about how lucky we are because we have “work hour restrictions.” To fool my brain into not stopping, I’d lie to myself. I’d tell myself that if I just got out of bed at 3:30 one more time I could go to bed early that night, or if I just got through a few more notes I could go home and finish the rest tomorrow. I thought I could just keep going at that pace and nothing terrible would happened until I woke up in the ICU and a doctor told me I had tried to kill myself.”
“In general surgery residency I had one week in which I worked 125 hour….I did a weekend of 72 hours in which I only got 4 hours of sleep. I would secretly hope to get in a car accident and maybe break a leg so that I would be forced to take off from work…just so I could get some rest.”
“During intern year at a program with a nominal 80-hour work week, I worked 100 hours per week for most of a month. I was interviewing a patient when I suddenly realized that I could not remember what I had just asked. I excused myself abruptly and rushed down the hall where I collapsed on the bathroom floor. I leaned against the wall and felt relaxed for the first time in weeks. My face was wet and I realized I was sobbing. I was so unaware of how exhausted and impaired I had become. I cried because I was tired, and also because the patient I was seeing deserved better attention and care than I was capable of providing. I couldn’t remember any details of his chest pain or risk factors for heart attack. I couldn’t even remember his name or his face. Only that he was friendly and he trusted me. I felt intensely guilty for not being able to stay awake, let alone think like a doctor. I nodded off while crying, propped up against the wall. I woke up and forgave myself. I think I was away from him for less than 10 minutes. I walked back into his exam room and said, “Where were we? Let’s start at the beginning to make sure I get this right. Because what you are saying is really important.” That month during my evaluation, my program director told me that my total number of work hours was a sign of inefficiency. I later learned that others were also working 80-100 hours per week but they falsified their hours to avoid criticism.”
“I have fallen asleep at the wheel thousands of times since medical school. I literally would wake up the next day in my work clothes and not even remember leaving the hospital. I drive from 45 min to 4 hrs to rural hospitals now and in training, currently working up to 7 straight 24’s in a row.”
“I was post call after a 30-hour shift and rear ended a car while driving uphill. No one was hurt but I remember the guy saying ” you hit me driving up hill.”
“I was so sleep deprived that I’d fall asleep while writing patient notes and write my dreams into the notes. I’ve fallen asleep on a pile of charts only to have the nurses cover me with blankets. I woke panicked because I was hours behind in my work. I’ve fallen asleep standing up in surgery and witnessed my attending doctors fall asleep while doing surgery. I actually passed out at the end of a 36-hour shift and woke up on a stretcher in the recovery room.”
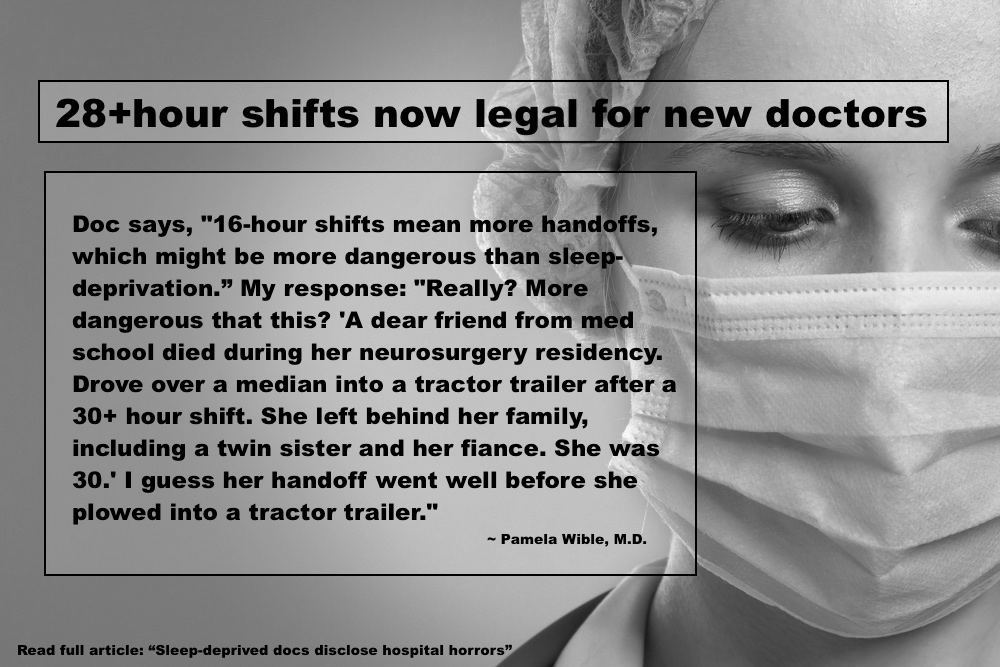
“A dear friend from med school died during her neurosurgery residency. Drove over a median into a tractor trailer after a 30+ hour shift. She left behind her family, including a twin sister and her fiance. She was 30.”
“I had married the year before residency, and for that first 2 years, I was either at work or asleep, so didn’t see my wife, and it was the start of the erosion of the relationship that led years later to divorce. I also suffered permanent health problems from extreme sleep deprivation. Prior to residency, I slept fine (8 hours/night) and had regular bowel habits. Since my internship, I developed lifelong severe insomnia, and went for decades on 4-5 hours of sleep/night, as well as severe constipation, using the toilet about every 5 days.”
“I was at one of the most humane programs in the country, yet as an intern and I would frequently gag on water while trying to drink. I knew by then that stroke patients and others with neurologic impairment had swallowing problems. Mine always went away while working less than 50 hours per week.”
“During internship I was driving home after a 30-hour call. It was dark and rainy out. The usual road I took home was closed, so after some roundabout driving I got on to the garden state parkway in NJ going in the wrong direction. Thankfully a police car saw me and pulled me over as I realized I was going into oncoming traffic. He escorted me all the way home.”
“I was working in the NICU and commuting 45 miles each way to and from the hospital when I was involved in a serious car accident in which my car was completely totaled. My program directors were upset that I did not make it back to work the next day (as I had to deal with insurance, get a rental car, etc.) Before this, I had a perfect driving record.”
“I was struck down with a very severe depression in the context of emotional conflicts and severe sleep deprivation, after doing a surgical rotation with every other night call and lots of degrading comments from the surgeons recommending that I go into nursing or teaching instead since those were “good professions for women.” This was 1983. I was supported in the sense that I missed 6 weeks of medical school without censure while I was too debilitated to move physically. I spent those weeks mainly sitting in a corner of my apartment, crying, and seeing my psychiatrist once/week for therapy and meds.”
“I have gained easily a hundred pounds over the years in part from eating to stay awake. The state police have woken me up on the side of the road many times when I pulled off the highway to sleep because I couldn’t stay awake until the next exit.”
Are these the doctors you want to see in the hospital? Protect yourself and your loved ones. Always ask, “How long have you been on your shift, Doc?”
Let the ACGME and Dr. Thomas Nasca know how you feel about their decision to allow doctors to work 28+ hours without sleep: Accreditation Council for Graduate Medical Education 401 North Michigan Avenue, Suite 2000, Chicago, IL 60611 or call 312.755.5000. Email Dr. Nasca: tnasca@acgme.org
__
Pamela Wible, M.D., reports of human rights violations in medicine. Have a story? Contact Dr. Wible.














It doesn’t stop with residency or fellowship; I’ve been out for 17 years. We’re a couple of docs short right now, so I’m in the middle of a 73-hour shift. My relief should arrive tomorrow evening.
168-hour shifts for hospitalists in some US hospitals: https://www.idealmedicalcare.org/blog/physician-whistleblower-exposes-human-rights-abuse-in-u-s-hospitals/
We don’t allow truckers or pilots to work over 60/hr week. See their limitations here: https://www.idealmedicalcare.org/blog/pilots-doctors-truckers-work-28-hour-shifts/
Human rights violations in US hospitals. Terrible.
28-hour shifts. Hmmm. A band-aid only works over wounds appropriate for their proper use. Otherwise, unintended consequences can occur. If hand-off and communication are two known problems with patient care, why not find solutions to improve hand-off and communication other than legalizing 28-hour shift work where known negative consequences have been documented for both staff and patient?
Maybe, just maybe, what is needed is to approach improving patient care from a systems perspective without potentially jeapordizing the physical and emotional health and welfare of staff and increase health risks for patients. Health systems may be putting their brand, community reputation, staff retention rates, and patient experience scores under fire. Let us not forget we live in a litigious society. Bring that thought into the equation. The answers to this problem lies beyond the horizon where decision-makers must look to see the bigger picture other than 28-hour work shifts.
You nailed it.
I’m glad I’ve been enlightened about this. I may not be a doctor, but I will definitely spread word of this. Btw, what countries is this happening in. I definitely know it’s going on in USA.
To: Dr. Thomas Nasca
Hello,
It is ludicrous and unsafe to allow twenty-eight hour shifts for doctors. I know. I am a producer/director and have worked shifts like this on a sustained basis for years. It causes sleep problems for life. It is dangerous and abusive and it doesn’t help the bottom line if companies manage staff effective.
Stop this immediately.
Thank you,
Paula Virany
We can’t wait for the fox guarding the henhouse to be nice to the hens.
“Dear Dr. Wible, I have a horror story caused by a pediatric resident at the end of a 36 hour shift. He was ordered to give a dose of chemotherapy intravenously to a three year old child with leukemia. In his sleep deprived stupor he gave the drug intrathecally into the spinal fluid. The child died a painful death. The shadow of that devastating mistake followed that doctor as long as I knew him.” (just got this email – published with permission)
Thank you to all the physicians who contributed to this important documentation. Thank you Dr. Wible for compiling it!
Labor of love. Trying to save my beloved profession from unethical leadership. Health care human rights violations impact physicians, patients—and even innocent families who may be driving down the highway next to a sleep-deprived doctor. Just sat down next a guy today who told me his friend just died in a car accident two days ago after a 48-hour shift at a Maryland hospital. Now he is talking about how to help support her children who have been left without a mother!!!
(Sharing anonymously as hospital employees are afraid to speak out):
The doctors at my hospital have been told they are are 24/7 call…meaning they will, for their salary, work whenever they are called, for as long as they are called, no restrictions.
I said, “I thought indentured servitude was outlawed a hundred years ago??”
What other profession allows this?
Incredibly criminal,incredulous, ungodly a violation of human rights to both healers providing healthcare and the patients and clients they serve.
I challenge the physicians/administrators who are making these decisions to only schedule their personal and family appointments with doctors who are sleep deprived.
And the stories above are just the tip of the iceberg. No apparent legal protection for the human rights violations of our new (and old) doctors. Other industries would be shut down with this kind of abuse.
Excellent point!
Perhaps state medical licensing boards should stop labeling and punishing “impaired physicians” and start actually protecting their patients (the public) from unsafe/unhealthy work environments. NOBODY should be working more than 12-14 hours in a day without a 10-12 hour period for rest, sleep, and nutrition. NOBODY should be working 7 days per week for weeks on end without time for rest, recreation, family, friends, exercise, fresh air, daylight, healthy meals, personal medical appointments, and other self-care activities. I routinely worked 100-120 hour weeks in medical school and residency, sometimes allowed to sleep only every other night for weeks on end. I got in trouble once for excusing myself from patient care after I hadn’t slept in 80 hours and was starting to have hallucinations (vague shadows in the corners of my vision). My Chief Resident reported me to our Residency Director for not finishing the last 2 hours of my shift. I didn’t abandon my patients; my daily notes and duties were done, and I simply missed our second daily bedside rounds. All healthcare professionals have an ethical duty to not practice while “impaired” — even by sleep deprivation. Maybe we should start more closely examining (and perhaps regulating) the ethical responsibilities of the ACGME, public and private hospital administrators, medical staffing companies, state and federal government officials, state medical licensing board staff, and the FSMB. Perhaps a month-long workshop/retreat should be offered for all of these “stakeholders” (and their attorneys) — where they can be subjected to the same working conditions (and duty hours) that they impose upon physicians. Just to make the experience more realistic, participants should face the risk being labeled as “impaired” and permanently losing their job, license, career, and future employability if they are suspected of showing signs of fatigue, discouragement, irritability, “burnout”, depression, or other personal weakness or illness. Finally, this experience should definitely include the same risk that physicians have for public humiliation, loss of personal healthcare privacy, and devastating financial exploitation when they are suspected of possible “impairment” (see last sentence for qualifying conditions) — through the same expensive closed network of self-referring “Physician Health Program” profiteers who extort billions of dollars per year (for “evaluation”, labeling, “monitoring”, “treatment”, and mandatory unnecessary drug/alcohol testing) from physicians who are alleged to be “impaired”.
Truth IS stranger than fiction. Just talking about what physicians go through in their toxic working environments is enough to give someone PTSD. I just shared some of this in an elevator at a hotel. Yes, all were shocked to learn doctors could be FORCED to now work 28 hour shifts. All were surprised that docs die by suicide in such high numbers. All were probably relieved when I got off the elevator on the 17th floor. There is only so much of these horror stories that the average person can fathom. Yet we live this every day as doctors. With NO support. Only punishment by regulating agencies, PHPs, and our medical leadership that actually upholds these human rights violations.
These stories seem unreal though they’re 100% true. Those at the helm of the death machine called health care have blood on their hands. I don’t know how they can sleep at night knowing that their decisions increase suicides among doctors and kill innocent patients and families just driving down the highway who have head-on collisions with sleep-deprived docs. It is hard to even put this into words. Not enough exclamation points to drive home the emotion here . . .
I’ve been on the phone with a mom who lost her ONLY child to suicide in med school. I wonder if our leaders who sign these 28+ hour shifts into law ever get to spend time talking the those who have lost their loved ones to this antiquated, barbaric medical education system rampant with human rights violations. So sad.
It doesn’t have to be this way. I’m an eternal optimist. I know we can do better.
Actually, regarding PTSD,a study was conducted here in Canada just a few years ago, and it was found that 2% of residents filled the criteria for a PTSD diagnosis. I’m pretty sure (although a psychiatrist could inform us on this matter) that this % is higher than inthe general population.
And they should have the stress of possibly killing someone while trying to help them while they are feeling barely human.
This was horrible. When I read the justification this morning, they basically said that “since data doesn’t show more errors are made or that the physicians feel worse about their life or career, we will lengthen hours because we want to for our own purposes.”
I told my husband about this decision (he is the physician in our family), and he was furious. When they conclude that they can extend the hours because it doesn’t seem to kill more patients or make the interns more miserable, they are asking the wrong questions.
My husband said, “Why don’t they ask how many residents die from accidents because they are sleep-deprived? Or how many commit suicide later from all of their abuse? Or how many die young from stress-related diseases when they are older? They are committing ABUSE!”
He views it in pretty black and white terms. It is abusive and evil to exploit someone more deeply and risk their lives simply because there isn’t enough evidence that more people are killed or miserable by extending the already too long shifts. Maybe the reason that the data didn’t show that those with the longer shifts were more miserable than those with shorter shifts is because lying about your hours is endemic in the system? If you don’t lie, you could lose your career? This means that many who have shorter hours on paper really work longer hours, and they are equally as miserable.
Look, we have solid stats that ER docs die younger than other docs because more of them die in car wrecks after their night shifts. That alone should tell us that residents at any level should not be made to work these insane shifts.
One week during his surgery intern, my husband was home for 18 hours total, six hours a night on three nights out of seven. I spent the night one night in the sleep quarters. He was paged so many times that before the end of the night, I cried from constantly being awakened, and I rarely cried back then. (I still rarely cry for myself. I cry easily for others. When I cried back then from the pager going off, it was instinctive exhaustion from my own condition; I was not crying at that moment for my husband.)
We were too young and naive to recognize the abuse as abuse. Hopefully today’s young students and residents are wiser.
Oppressors won’t apologize spontaneously. Change depends on the victims. Here’s the problem: victims who don’t realize they’re victims are at high risk of becoming victimizers—thus perpetuating the cycle of abuse.
Actually, regarding PTSD,a study was conducted here in Canada just a few years ago, and it was found that 2% of residents filled the criteria for a PTSD diagnosis. I’m pretty sure (although a psychiatrist could inform us on this matter) that this % is higher than inthe general population.
I was given a botched appendectomy in my senior year of medical school. The exhausted intern who had me sign the release for surgery gave me the form for a cholecystectomy. I wouldn’t sign it and he apologized; it was the second day of his surgery rotation, and he had been in the surgical suite since 8 AM the day before; unfortunately he had also had last overnight call in the pediatric rotation previous to that, so really he had been up for two days and two nights. He pale, was nearly inarticulate and blank faced as he brought in the correct form. Then they had him tie off a blood vessel during the surgery and he went one branch too far down and tied off the vessels to the entire right colon. So I had an unnecessary ascending colonectomy done too.
No, I didn’t sue; I just felt so sorry for the guy.
I’m so sorry Joanne. Terrible. According to ACGME care is actually improved on longer shifts. Maybe you should submit a letter?
Let the ACGME and Dr. Thomas Nasca know how you feel about their decision to allow doctors to work 28+ hours without sleep: Accreditation Council for Graduate Medical Education 401 North Michigan Avenue, Suite 2000, Chicago, IL 60611 or call 312.755.5000. Email Dr. Nasca: tnasca@acgme.org
Dear Dr. Nasca,
I am very concerned that the ACGME has made the decision to allow 28+ work hour shifts. This extremely shortsighted decision impairs the health and safety of both residents and patients. I am an adult psychiatrist in Brookline, Massachusetts who routinely provides psychiatric care for medical house officers and physicians. Last week, the Vice Chair of the Department of Psychiatry of a large tertiary care hospital system called our office to discuss the need for more outpatient psychiatry services for house staff. He mentioned that they have never witnessed such need as residents from all specialties are requesting care. This is obviously a complex issue but the reality is medical training has become excruciatingly difficult as our patients are sicker, hospital stays are shorter and documentation requires using cumbersome inelegant software. On top of all this, being a physician demands interpersonal skills that are spot on- negotiating and working with patients, families, nurses and ancillary staff. How can we expect severely sleep deprived house staff to complete all these tasks without experiencing adverse health effects. Shame on the ACGME for not protecting the health and welfare of physicians in training!
Lisa Giudice, MD
Brookline, Massachusetts
781-771-8011
Thanks for speaking up Lisa. Silence will not save us. All change depends on the victims standing up to prevent the cycle of abuse passing on to the next generation. I wonder what Libby Zion’s dad would say about this decision? We need more Sidney Zions.
Call me old school but I did 36 hour shifts
Every third night on call for nine years plus
A memorable 88 day shift once….(in the us)
28 hours sounds decent in the sense “the
Briuses will heal quickly kind of way”
BTW an anesthesia resident in mexico city
Died from “Karoshi” or overwork in japan last
December…..Its causing rightfull indignation
The program head hated him and refused
To upload his grades for the last semester
So he would not graduate, 15 attendings signed
A letter saying he should be allowed to graduate
But the boss said no….went into utter despair
And stress and died from a heart attack at
28 with no diagnosable heart conditons at autopsy
. ……we are about in the 1980’s compared to
The us
Reminds me of the many cases I hear about regrading third-year residents who are screwed over, fired, not given credit for one rotation so they are never allowed to graduate. Sadistic residency directors and attendings (who desperately need mental health care themselves) are taking their personal torment out on colleagues, Terrible. Physicians are the most emotionally distressed group of people I’ve ever met.
This is a tragedy. It is ironic knowing all that sleep deprivation can do to the body that they will be allowing people who have to mentally sharp to make complex life or death decisions to work under such conditions is beyond frightening.
My husband has very complex medical conditions and spends a lot of time in the hospital. It chills me to the core that at some point he may be under the care (he actually probably has been…) of someone who is sleep deprived. We are at the Emergency Department as I type this. I always feel like I have to be hyper vigilant because I have no clue if the clinician who sees him will be rested or at the tail end of an ungodly amount of hours. While I don’t practice medicine, I work in healthcare and know enough to ask questions and advocate for my husband. Amazing that pilots and flight attendants have a limit on how many hours they are allowed to work, but those who are responsible for making medical decisions for the most vulnerable are not. Shame on them.(sorry for the grammar and spelling. It’s been long night).
Subject: Horrific Idea
Dr. Thomas Nasca,
Who in the world came up with the idea of 28-hour shifts for new physicians i.e. interns?
This is a dangerous mistake. Think of the patients. They are the ones who are going to suffer; rescind this order now and get back to reality.
I’m a nurse practitioner have seen it all. You need to get out of your ivory tower and actually go take care of patients. Patients are getting increasingly complex and you will see physicians killing themselves en masse.
Judith Vance, MN, MPH
Tucson, AZ
Thanks Judith for speaking out. You are spot on.
I went to medical school in the early seventies. During our clinical rotations in third year we did 36 hour shifts and worked up all the
patients the Intern or resident did. At that time there was a quota on women in medical school of 10% which was legal at that time. On Medicine
rotation there were no on-call rooms for women so the nurses would allow me to use an unoccupied patient room until a patient needed it so I would then wander around the hospital or check on patients or got called to see a patient, until Rounds at 7 A. M. I remember one day when the Intern, after we were up all night with no sleep,
fell asleep leaning against the hospital corridor wall during Morning Rounds right in front of the Chief of Medicine who did not even notice. One of the other women students was brought to tears during pediatric Grand Rounds due to the public pimping. She subsequently
became head of Geriatric Medicine at a prestigious ivy-league Medical School. On my fourth year Medicine rotation I came down with Hepatitis
and was ill and working for 2 weeks before my urobilinogen was positive and the Transaminases were off the charts. I told the Chief of GI I was icteric but he did not see it. Meantime on Hematology elective I was giving IV meds to leukemia patients on reverse isolation. I could not make it very well from the Hospital parking
lot to clinic where the nurses said, “Oh, Doctor! You look awful, come
over here and lie down”. Which I did , for a few minutes then back to work. My blood sugar was 60 due to not being able to eat and probably
impaired gluconeogenesis. Then one day the Chief of GI came in
to the nurse’ station where I was and put his hand comfortingly on my
shoulder and said, You have Hepatitis. I said, Oh thank God! Can I go home now? So I went home for 2 weeks and the Chief of GI called me almost every day to see how I was. Then it was time for another rotation to begin and my bili was about 3 so it was back to work.An
Internal Medicine resident said I had it easy because his hepatitis was worse and he worked more than I did. I remember one time as an Intern, on Medicine rotation where in the 750 bed hospital House Off-
icers were responsible for evaluating all medical problems on non-ICU
medical patients, there was a rare 36 hour shift where I did get to go to sleep but when the nurses tried to get me up to see a patient
I could not get up, I kept falling asleep again. I don’t think I ever
saw the patient. Hurting people hurt people.
In the eighties, when I was in private Internal Medicine practice, there was an article and editorial published in a respected medical
journal (don’t remember which) where the new syndrome Medical Student
Abuse was discussed. It was likened to child abuse in that the abused were helpless to prevent it and had no recourse. The perpetrators had been similarly abused and were passing on what was done to them and
do not recognize the problem. So medical culture has known about the problem for thirty years at least, and nothing has been done except to blame the victims and sweep it under the rug. “Resiliency training”? Makes me want to vomit! Would “they” the “authorities,” say that to a child abuse victim or a rape victim or a slave? I have been retired for
nine years and I still have nightmares and flashbacks from PTSD and similar experiences too numerous to recount. And things have only gotten worse
from the research I have seen. It is time for the perpetrators to admit the problem and take the responsibility to stop it. And we must continue to speak out.
“Hurting people hurt people.” Tragic that the medical system sacrifices its own people in such high numbers. I believe most of us have had experienced PTSD from our chronic mistreatment and unrelenting exposure to human suffering & death (without any support, only punishment for our tears or cries for help). Some of us don’t make it. Suicides are covered up by the medical organizations that profited from our sleep deprivation & ungodly work hours. Criminal.
“Hi Pamela, I am mailing in my residency contract today. I thought it was very strange to sign a document that had no cap on ‘duty hours’ as defined by the acgme.” (letter from an intern I just received). Why do our doctors-in-training have no legal protection? I get calls from young doctors being forced to work 120+ hour shifts. Criminal. No other industry could get away with this in the USA.
Hi Pam,
To my understanding, there’s a lot of research clearly showing that sleep restriction impairs decision-making far more than we appreciate. It’s also correlated with lots of unhealthy outcomes, risk of accidents, etc. There is also a lot of research on circadian rhythms and the impact of disrupting them. If there is an educational advantage to working such shifts (which I don’t necessarily believe) then it is surely offset by all the negatives.
I don’t believe that the deciders were “honest brokers” who considered all the evidence. They must have had an axe to grind. It’s hard for me to understand what’s really driving this decision. Greed? Machismo? I’m thinking about making an evidence-based reaction to this. Any thoughts?
— Jim
James F. Cox, Ph.D.
Thanks Jim! We need more public awareness and less professional denial around extreme sleep deprivation and human rights violations of our resident physicians (and docs in general).You’ve got my approval. Keep going! Pressure from all sides.
Dear Sir or Madam,
I’m worried about the planned reversal of duty hour restrictions for physicians in training and I believe lifting these will result in increased death by suicide. While the number of dead doctors has been unavailable in the past because of systematic ignorance and denial, the invisibility of physician death by suicide is rapidly becoming a thing of the past, due in part to the dedicated efforts of Dr Pamela Wible who is shedding light and making public this disgraceful phenomenon. I call on you as gatekeeper of the lives of future physicians to do no harm. Work hour restrictions for physicians in training are crucial. These protections save lives, both of patients and of physicians. As a former neurology intern who lived through the grueling destruction of the pre-ACGME work hour restrictions in the 2009-2010 epoch, I barely survived what in retrospect I believe was something like a nervous breakdown which I attribute mainly to sleep deprivation at that time, as well as emotional sadism on the part of some of my faculty upper level residents. I have observed several of my classmates loose their lives through suicide, due to multiple factors, particularly sleep deprivation during residency at the time when duty hour restrictions were not in place as they are now. Reversal of work hour restrictions will result in driving up rates of completed suicide by physicians in training. In the past when these numbers were not tracked and documented, it was possible for ACGME to sweep these “bad outcomes” under the rug. As I wrap up my final year of psychiatry residency and join the workforce, I call out directly the cause and effect of increased death by suicide of residents that are predictable and should be expected as a direct result of sleep deprivation, which will result from lifting current work hour restrictions. Now that these deaths are being tracked and observed by Pam Wible MD and her group, you can expect in the future to have ACGME’s decision of this week become prominent in social media as well as medical journals of the future as the landmark event triggering accelerated suicide rates among physicians in training. Understand that the cause and effect relationship between overwork and death is no longer a medical mystery and that the decisions you make today won’t go unnoticed when that death rate rises. You will be in the newspaper and on Facebook and there won’t be anywhere to escape the fact that your decisions directly affected lives of physicians and the families and patients who have lost them forever.
Respectfully,
Lisa E Goldman MD MSW,
4th year psychiatry resident
As you mention these decisions must be called out publicly and your letter should not just disappear in some folder on an ACGME computer or in the trash. Thanks for making your statement publicly. Silence will not save us. Those who are complicit with human rights violations of our doctors in training perpetuate the cycle of abuse.
Doc says, “16-hour shifts mean more handoffs, which might be more dangerous than sleep-deprivation” My response: “Really? More dangerous that this? ‘A dear friend from med school died during her neurosurgery residency. Drove over a median into a tractor trailer after a 30+ hour shift. She left behind her family, including a twin sister and her fiance. She was 30.’ I guess her handoff went well before she plowed into a tractor trailer.”
Additional letters collected by Public Citizen.
Dear Dr. Nasca
I implore you to reconsider the decision to allow new physicians to be scheduled for 28 hour shifts. This is the most inhumane administrative move I have witnessed in my lifetime career in healthcare. While I am not a physician, I do understand the myriad pressures that caregivers face today. Asking someone to work 28 straight hours almost guarantees the chances for serious errors while eroding the humanity of the individual physician. I am confident that the medical community can create some other alternative means of matching patient care needs with available staff besides the 28 hour shift.
Respectfully yours,
Charlotte Pearce
Horrible for both doctors and patients. How can we as patients avoid these intern/doctors who are putting our lives at risk?
1) Protect yourself and your loved ones. Always ask, “How long have you been on your shift, Doc?”
2) Boycott hospitals that routinely violate the human rights of their staff.
3) Speak out. Share this article. Most folks have NO idea this is happening.
Silence will not save us.
Doctors in leadership positions who work 9-5 and get home for dinner with weekends off somehow don’t believe younger docs need sleep.
The same seems to be true in training programs in some other countries. I live in, and trained in the Philippines. Even before graduating from medical school or taking the licensure exam, students are expected to have 28+ hour duty shifts, every two to three days.
One really early morning just before handing off our patients to the incoming group of doctors and interns at the ER, I suddenly collapsed and began seizing. In fact it was one of my patients who noticed me first, and called for help. I woke up in the interns’ quarters, where my friends were about to start an IV line. So instead of my endorsing my patients….I was the one who got endorsed.
Sadly common. Seizures. Hallucinations. Suicidal thoughts. Falling asleep on patients. And then getting in fatal car wrecks on the way home. Modern medicine.
I think the most effective way to fix this problem is to encourage residents to inform patients who were victims of poor care due to their sleep deprivation to file lawsuits against Dr. Thomas Nasca and the ACGME.
5 lawsuits top and the policy gets changed.
Splendid idea.
Thomas Nasca,
The catastrophic consequences of your decision to increase resident work hours to 28 hour shifts will be your responsibility. The blood of residents and patients who lose their lives as a result of this reckless change in policy will be on your hands.
William G. Stueve, MD
Lawrence, Kansas
Dr. Thomas Nasca,
As a pgy4 resident physician in Texas I would like you to know how disappointed I am by the ACGMEs decision to return to 28 hour shifts for interns. This decision is damaging to both patients and residents. We all know that sleep deprivation leads to more errors, less focus and less empathy toward patients. Whether or not the studies reflect the data, long hours are detrimental to resident well being and patient safety.
I know that I personally make more errors towards the end of long and busy radiology shifts, and I’m sure that I am not alone. Sometimes my errors go unnoticed and often they don’t affect greatly patient care, but they are there. With each long night shift in the EC, I always fear that I will make a fatigued induced decision that will negatively affect a patient. I know it’s only a matter of time.
I am saddened for the patient and doctors that will negatively be affected by this rule. For the surgery intern who will crash their car driving home after a long shift. For the patient who has a bad outcome from a decision made by a sleep deprived physician.
Other industries do not tolerate these kind of unsafe working hours. Why is medicine so far behind? Why are truck drivers, pilots, and oil field workers more regulated than surgeons. We must move forward and improve medical culture.
I believe that the ACGME is taking a big step in the wrong direction with this decision. We need physicians to be happy and healthy, not sleep deprived and callous. Please reconsider your stance on this issue.
Sincerely,
WB, MD
It was my PGY3 year and I was the chief resident of transplant surgery. Unfortunately at my small program, there were no other residents on the service to share a call with me, therefore I took call 24 hours a day every day for the entire month. One particular week, we dissected two different donor kidneys back to back one night and found neither of them to be sufficient for transplant and sent them back, therefore waking up our patient without ever having the transplant. That was some nine hours of: waiting for the left kidney to arrive, prepping it on the back bench, finding that it wasn’t good enough, sending it back, waiting hours for the second organ to arrive, and repeating the process. This was day four of a four day streak where I had been awake with only one or two hours of sleep total. At the conclusion of this day, it was after dark, I left the hospital parking garage as I always did to drive home, 20min, to my apartment. I have done this so many times that I could do it without even really thinking about it. However, sleep deprived, I was confused and hallucinating and ended up driving 30 minutes out of my way and getting lost in a small town I had never been to. When I finally noticed my surroundings, I realized I had no idea where I was. Sleep deprived and completely frustrated because I just wanted to be home in my bed to get a few hours of sleep before I would have to be back at work. I pulled over into a gas station and started crying, completely forgetting I have Google maps on my phone to help me find my way home. I sat there for a moment still pretty confused and very very tired and finally figured out where I was and got back on the road. I had been crying mostly because I knew I was losing the few hours of precious sleep that I could get on that month of transplant surgery.
You cannot tell me sleep deprivation is not dangerous, hazardous to one’s health, or damaging in many ways. I lived it and it has taken a permanent negative toll on my life.
Medical students, residents, nor even attending physicians should be held to a standard where you have to be awake for so long doing something that is so high stakes. If CMS would increase the general surgery class-size and turn out more surgeons, this could be alleviated.
Dr. Nasca,
I am extremely disappointed by the ACGME’s decision to extend resident shifts to 28 hours. You are speaking to a nurse here, not a physician, but I am still the operator of a human body, which experiences physiologic effects from sleep deprivation. 4 years ago, after only an 18 hour shift in the ED, I ran a red light on my way home. I remember vividly as the thought “wait… was that a red light?” slowly sunk into my mind miliseconds before a car entering the intersection smashed into the passengers side of my vehicle. I may not have made any mistakes with my patients that night, but my actions did result in a poor outcome for that man in the oncoming vehicle who, though he fortunately walked away from the accident, most certainly suffered significant musculoskeletal pain and trauma in the coming weeks vs years vs lifetime. These aren’t metrics that are even recorded, so how can you be prepared to make this decision to increase the work hours of brand-new, unexperienced doctors. I’ll be convinced that the welfare of the patient or the education of the physician is being kept in mind only when these type of excessive work conditions are combined with a sign hung around the physician’s neck that informs those around them that they are “impaired and unable to answer questions or make decisions”. I’ll buy it that’s it’s helpful for a physician to see out the entirety of their patient’s care (even though there’s plenty of evidence to suggest that a human brain cannot learn effectively when sleep deprived, so chances are that this “learning experience” is just going to become some hazy memory figment in this exhausted human’s brain anyways – and if this human were a patient of mine and they described to me their work hours in the context of their health, I would likely recommend that they find alternative employment….). However, I will never endorse that it is safe practice for this human trainee to make decisions about patient care when that have not had adequate sleep, breaks, and nourishment.
This decision reeks of carelessness. Why does the stereotype persists that physicians are uncaring? Because physician leadership, like you and the ACGME, make uncaring decisions.
Sincerely,
Concerned caregiver, patient, daughter, and friend
Dr. Nasca,
You and your organization’s choice to make 24-hour+ shifts “legal”is immoral, unethical, and inhumane. Why do you think this is even remotely acceptable?? I demand that you provide us with an answer. And an answer of “medical mistakes happen because of handoffs” is complete and utter nonsense. Residents are there for training and learning. No form of quality education happens in an atmosphere of sleep-deprivation and extended hours. You put lives at risk from doctor to nurse, all the way down to the patient. We all preach evidence-based medicine; there are plenty of articles refuting this decision and you make it based on one or two trials. Truck drivers, police officers, firefighters, airline pilots, and many other professions HAVE LIMITS. Why are we different??
Shame on you and the ACGME. Do the right thing and fix this. Help change the culture of medicine and stop making the problem worse.
Mike Sass, DO
Internal Medicine Resident
Thanks Mike for speaking the truth. Silence will not save us. When outrage overcomes apathy we WILL have change. Public has no idea.
Dear Dr. Nasca,
It is with significant frustration that I write to you regarding my awareness of the new change to physician work hour restrictions. To say that this is a horrible decision is an understatement. Not only are you threatening the well being of the young resident doctors, but you are placing the patients under their care at risk of serious medical error.
Currently, our profession is in serious jeopardy, with many physicians leaving the profession entirely, due to the sheer lack of sustainability and deep dissatisfaction with the system that they are being asked to perform within. Simply stated, we have a shortage of physicians currently and it is in my opinion that you have placed yet another burden on a broken system of medical eduction. I envision that, as a result of this ridiculous and unethical work requirement, there will be legal ramifications for the physicians that are overworked and the hospitals/graduate programs that employ and train them. In other words, families will sue not just the physician but the program that is driving these young doctors to breaking point, where they are too sleep deprived to act appropriately in the best interest of the patient.
I cannot deny the hypocrisy in the “do no harm” oath we are asked to uphold. With all due respect, you are harming our doctors, our patients and our modern medical system. Shame on you.
Dr. Rebecca Gallagher
In specialties without enough people we are left with the choice of no one cover or work more. That has gone on for years, it then becomes codified in the administrations mind. We are honorable and won’t let patients go uncovered. I am starting my normal 80-90 hr week and that is status quo (21 yrs now) and do not even really realize how sick that is, I allow the abuse.
We have allowed ourselves to be abused for so long that we have become our own abusers. And we self-abuse with pride.
This is an issue very close to my heart. I worked many 30 to 36 hour shifts during my internship as a doctor in South Africa. Thankfully the working hours for junior doctors have now been regulated and reduced in some provinces to 24 hour shifts (which I think is still far too long), but we are making progress at least. Most of us know colleagues who have died in motor vehicle accidents while driving home from these shifts, most of us have almost fallen asleep or fallen asleep ourselves while behind the wheel. This is not to mention medical errors made and the physical and emotional strain on doctors and their families of these incessant hours. As others have said, it is unlikely that this sort of abuse would be tolerated in any other industry.
If they want doctors to give there best .The administration of hospitals should realize that as a human not every person has a stamina to work for then 8hours straight to maintain there concentration on the patients.Doing so many hours makes you unsuitable to do your job.And if you think this is possible then give the same duty hours to every professionals and we will see who is right and wrong.Althiugh I have done the same duty hours in my housejob.
Dear Dr. Nasca,
I abhor your and the ACGME’s unexcusably irresponsible decision to allow resident physicians to work 28 hour shifts. There is no conclusive evidence demonstrating that prolonged work hours increase the knowledge base of a physician in training.
Prolonged work shifts and over-working do, in fact, have conclusive causal evidence demonstrating poor medical outcomes and adverse health risks to the person working prolonged shifts and excessive work hours.
I recognize that there are financial pressures on hospitals and residency programs, as well as educational requirements that need to be met – lower the pay and increase the duration of the training if need be. These are the only ethical ways to continue to train the physicians in our country. When I was a resident, I felt like I was zombie, for 3 years straight, and I never exceeded the 80 hour per week work rule. I did not feel human. By definition, this amount of work is inhumane. I would have gladly traded a lower salary and giving an extra year of training in exchange for a humane work-week.
The only safe and humane decision for the ACGME, OSHA, AAMC, and AMA (This letter will be submitted to OSHA, AAMC, and AMA as well as a workplace safety investigation complaint) is to cap a work shift at 12 hours every 24 hours, and at 40 hours per week for resident physicians and medical students.
Sincerely,
Shahram Hosseinion, M.D.
Hosseinion Family Medicine LLC
3942 SE Hawthorne Blvd
Portland, OR 97214
Dear Dr. Nasca,
I honestly don’t know how anyone on this committee can sleep at night, knowing that this decision will undoubtedly contribute to the deaths of multitudes of physicians, patients, and citizens who might be driving next to a sleep deprived physician. If you don’t already know about the impact of such work shifts, read this article, including the comments.
https://www.idealmedicalcare.org/blog/sleep-deprived-docs-disclose-hospital-horrors/?inf_contact_key=61d0614182bf5e2be4440dcdf490eb5758cc6693f0b1d4665052148ec69f5f45
Please reconsider your decision and reverse this legislation.
Sincerely,
Dara C. Lifschutz, M.D.
In the European Union the working hours are strictly limited. It may not exceed 12 hours a day. This is equally in force for residents, physicians during the day and during the night.
There was a case before the Strasbourg Court of Human rights.
I’d like to add the following:
duty hours are equal with normal working time hours.
Weekly working hours are limited to 48 hours, in some countries like Hungary you may be in duty service longer, if this is the case, the weekly maximum is 72,
The employer does not have the right to use the extra weekly hours between 48 and 72it without the employee’s consent.
The total of the yearly extra hours (above 8 hours / workdays of which we have appr. 251/year) may not exceed 416.
regards
weltner
I was asked to post this anonymously:
I agree about the dangers of sleep deprivation. But I don’t think longer residencies are the answer. Academic surgery is already 7 years. As is neurosurgery. And with the cost of school and loans accruing interest during residency, it’s impossible.
I fell asleep once post call during my second year. I woke up driving straight on a straight part of highway surrounded by cars. My heart was pounding in my chest when I realized what happened. It will never happen again, I would rather sleep in my car in the parking lot than drive that tired. But I couldn’t do a longer residency. We do spend a lot of time doing BS that doesn’t need to be done by doctors, and that time could be spent operating. Longer training isn’t the answer though, I think more efficient training is.
Dear Dr. Nasca
I implore you to reconsider the decision to allow new physicians to be scheduled for 28 hour shifts. This is the most inhumane administrative move I have witnessed in my lifetime career in healthcare. While I am not a physician, I do understand the myriad pressures that caregivers face today. Asking someone to work 28 straight hours almost guarantees the chances for serious errors while eroding the humanity of the individual physician. I am confident that the medical community can create some other alternative means of matching patient care needs with available staff besides the 28 hour shift.
Respectfully yours,
Charlotte Pearce
I was a single mother with two kids doing my residency at 1:30 at the stoplight I fell asleep my car just rolled into the other car luckily no one was hurt but it certainly relationship with my kids and it was very difficult I do not recommend anybody work that long we been fighting this since I was in residency back in the 80s time to put a stop to it Mylene and Middleton and Rucker Rucker MD mph
Those long shifts are slave labor not learning…..no one learns when their basic needs for sleep, food, down time, connection with those who matter are unmet. It is a shameful usery of people that must stop! I ranted about that in 1979 when it was my spouse and our friends being used up, wrung out, all traces of altruism for humanity turning to sour cynicism. THanks for all you’re doing to empower physicians and students/residents. Debra Waldport, OR
Not to mention FEAR. Terror-driven teaching.
Dear Dr. Thomas Nasca,
As a practicing family doctor and assistant professor in family medicine, it is my distinct observation, that physicians that are forced to work overtime are subject themselves to mental fatigue, burnout syndrome and depression.
In a recent study, 23% of the resident physicians and practicing physicians were found to be suffering from depression. Because of the mental fatigue that resulted from the required excessive required working conditions, the body suffers mental and physical.
By excessive work schedules, I mean, 8 to 12 hours of constant mental and physical work daily.
In 1969, as a intern at the Washington Hospital Center in DC, I experienced first hand mental and physical fatigue in obstetrics, internal medicine, emergency room care, ICU and CCU care as well as pediatrics.
Many days I would come home too tired physically and mentally to enjoy my family and a normal lifestyle! I often thought that this is just the way the doctors have to and expected to perform in a medical setting! It
I was often too tired to appreciate the medical insight and medical education that’s surrounded me. I felt that I had to do what I was told. I accepted the excessive work without complaining. It was the expected the norm for physicians to be overworked as I was told and observed.
I remember very many days I would not leave the hospital but slept over because of my extreme physical and mental fatigue!
My attending physicians in chief of medicine never concerned themselves about how I felt.
There was no discussion about the enjoyment and pleasure of being a doctor. You were just treated as the low man on the totem pole!
As I entered private practice in 1970, I felt obliged to continue working in the same vein as I had in the past. It’s a type a personality, I enjoyed my work. Everything was reasonable in the practice of medicine at that time. It was an honor for me too be a Family physician because of respect and trust of my patients.
After 43 years of practice, I recognized that medicine changed. There were more regulations and less time to treat patients have a high level of care.
This is what I expected of myself when I first started practicing medicine. In 2009, there were new requirements requirements for patient care. Less time four face-to-face medical exams with patients and more time with medical records and less time face-to-face with patients.
This was a direct dichotomy to my teaching in medical school. I resented the fact that could not spend adequate time with my patients. As a result of the new regulations in the ACA – Affordable Care Act, I felt overwhelmed as a solo family doctor. I spent an increasing amount of computer dictating in order to provide the patient with a complete report at the time of every visit.
Instead I gave the patient a instruction sheet concerning my treatment plan. Therefore, I was left with only one option — dictating the patient notes after I finished hospital rounds in the evening.
As you can well imagine as a busy Family Physician, well trained in office and hospital medical care, I had 10 to 20 or more patient charts to complete using my electronic medical record’s program! I’m sure you can understand and predict that I was working on patient records until 12 midnight or later! Tired and mentally exhausting for six days every week!
I wondered how long I would be able to continue this medical record process without feeling burnt out mentally and physically!
After three years of increasing stress as a result of excessive hours , I felt totally abused trying to keep up with requirements of the ACA.
I felt there my time to enjoy life was severely limited and restricted. I wondered how this would affect me mentally and physically continued
Obviously, I knew the consequences and decided that the excessive -greater than 12 hours a day would make me depressed mentally! I felt too fatigued to enjoy life. There for one day, I decided that that time to retire and enjoy the normal activities of life!
I felt that my life expectancy was too important and precious me. I felt that I could not longer continue on the same path. As I always told myself enjoy life to the fullest.
In conclusion, so I made the right decision.
I’m alive and well and enjoying myself without the frustration, anxiety and stress in my daily life.
Thank God I came to my senses!
John J Shigo M.D.
March 16, 2017
As a nurse, I was always concerned about the absurdity of making interns and residents work shifts that are way too long. I don’t understand why this still goes on. It is inhumane and dangerous, to say the least. I recently read a book written by a professor emeritus who was a physician at a major teaching university hospital. He was all for these hours and thought it made for better doctors. He was of the opinion that the young doctors are being coddled and it is not good for the entire process. I don’t understand that way of thinking because, whenever I was forced to do a double shift, I would be a danger to myself and others while driving home after having had no sleep for 24 hours.
Pure insanity.
Call me old school but I did 36 hour shifts
Every third night on call for nine years plus
A memorable 88 day shift once….(in the us)
28 hours sounds decent in the sense “the
Briuses will heal quickly kind of way”
BTW an anesthesia resident in mexico city
Died from “Karoshi” or overwork in japanese last
December…..Its causing rightfull indignation
The program head hated him and refused
To upload his grades for the last semester
So he would not graduate, 15 attendings signed
A letter saying he should be allowed to graduate
But the boss said no….went into utter despair
And stress and died from a heart attack at
28 with no diagnosable heart conditons at autopsy
. ……we are about in the 1980’s compared to
The us
If they want doctors to give there best .The administration of hospitals should realize that as a human not every person has a stamina to work for then 8hours straight to maintain there concentration on the patients.Doing so many hours makes you unsuitable to do your job.And if you think this is possible then give the same duty hours to every professionals and we will see who is right and wrong.Althiugh I have done the same duty hours in my housejob.
As an RN for 39 years, I’ve always thought this craziness was some sort of hazing to get into the profession, that if it were a college fraternity or sorority membership process, it and the frat would be banned for endangering the health and life of the applicant. Certainly airline pilots have very clear and stringent rules for flying a plane and sleeping. Why can’t medicine? I never understood the “rationale” given by practicing physicians, also quoted here, basically that “If I did it, you have to do it, too.” Yes, sometimes it might be necessary to work 36-hours straight through, like being stuck in a hospital during a hurricane or after an earthquake, but that would be a rare occurrence. (Perhaps this stubborn adherence to tradition that we’re hearing from MD survivors is a residue of PTSD, and *they* need some resolution for their trauma, first, and trauma this is, before they can support the next generation of physicians. Allowing the next generation of physicians to have it better than they did in no way minimizes their painful memories, but that they think it does.) The other “rationale” given is the number of handoffs would be too great and cause problems with continuity of care. Listen, if nurses can figure out how to provide quality continuity of care with 2 or 3 handoffs every 24 hours, and we’re with the patients constantly, 24/7, why can’t doctors? I’ve cared for patients in PICU who were so intense that nurses worked in 4-hour shifts – yes!! 6 handoffs/24 hours!! It was hard to cover staffing but we figured it out because that was in the best interest of the patient! What kind of stupidity says working until you are non compos mentis is a good thing? Oh, right, it’s arrogance from the Good Old Boys Club. I know the reason why the data doesn’t show more errors are made: it’s because nurses are taught from Day 1 of nursing school to watch and monitor and challenge every action and order as patient (& physician) advocate. We nurses are the safety net scrutinizing every order, watching procedures, and yes, tucking blankets around exhausted residents who are comatose wherever we find them: at the nursing station, on an empty bed, or in the bathroom. If that data about “lack of, or averted, errors” is needed, start talking to nurses. We see everything and we think this policy is abusive and a human rights, not to mention decency, violation. What is needed is hard science data, perhaps an fMRI as the doctor comes off the third or seventh 28-hour shift in a row, or even a SPECT scan at the beginning and end of residency. Now that would be a study that would rival the NFL concussion studies.
Thank you for caring and noticing the hazing Kate. Would be illegal in any other profession.
Two stories shared by Benjamin Van Raalte M.D.
“One of our surgical interns was asked what he was going to do for his vacation (We were at Cook County Hospital part of University of Illinois general surgery residency in the 1980s). He said he wanted to be paralyzed, intubated, and put in the ICU, he was too tired to even breathe on his own.”
“The other was when I was interviewing for surgical residency. There had been Pope Paul for 15 years passing in 1978. One of the residents said when he was an intern he was so busy that one day he realized he was two Popes behind.”
I read below a comment by Dr. Wible regarding the cycle of abuse, namely the positions of victim and abuser (that can be held by the same person).
Here’s a model that might help you in recognizing negative/prejudicial thought patterns: it’s called The Karpmann triad. In addition to the 2 positions I just named, in this model states that there is also the Savior position, which of course most md students/interns/md in practice are all too familiar with. Hence, the Savior position is conducive to the victim (and vice-versa), the abuser position is conducive to the victim position (and vice-versa). I’ve helped many students with this approach, as well as some colleagues in practice.
I even think it should be mandatory teaching in med schools.
I’ll finish this by thanking you Dr.Wible for this excellent initiative, (which has resonance even her in Canada).
Oh thank you for the insight. There is so much to learn here. Human psychology is the last frontier, for sure. Fascinating. WE can do so much better with insight and understanding. Upholding the human rights of all would be a great first step.
The point here is that once a caregiver recognizes he/she is experiencing this triad, this person is at high risk of burning out. Of course many here could rightfully that “they knew that anyway since they are working terrible hours under tremendous pressure”.
However, being aware of the Karpmann model can help you say no ( which we all know is notoriously difficult for mds…Savior position, victim position through helplessness feelings), as well as seek for help (which on average here in Quebec, Canada, takes md 8 years to do).
Human rights violations is not the same as “burnout.” One is a crime.
A fairly recent study found that after 18 consecutive hours awake the subjects’ performance was the same as that of subjects who were legally drunk (i.e. can’t drive). So how drunk will doctors be after 28 hours? This decision is spiteful, especially coming from someone working convenient “office hours”.
Email I just received worth noting:
Pamela,
Although, I completely agree with all of the points made regarding the inhumanity of the system, I believe that there is an underlying variable that is THE central point at the crux of this discussion. Lack of sleep and circadian rhythmn disruption. There is ample scientific evidence now available regarding the havoc that circadian disruption has on human physiology, including mental and cognitive processes. This includes inadequate regulation of light/dark cycles and insufficient sleep in general as well as individuals being pulled out of one of the various phases of sleep while on call during residency and into practice. The science is startling and yet for the most part completely ignored by the Medical System.
It begins in undergraduate work with highly motivated individuals burning the midnight oil with the intent of getting the coveted high GPA. It continues in the cut throat competitive environment of medical school and residency, and unfortunately for many, into their Professional practice. It is a brutal competitive environment, highly stressful and part of life for YEARS, all on inadequate rest and sleep.
I had an older brother who served as a Marine in Viet Nam. He mentioned to me once that after being up for extended periods of time, sleep being interupted every 2 hours while on patrol in the bush, that his exhaustion was so complete that he literally did not care if he lived or died. He slept on the ground during a mortar barrage throughout the night because he simply did not want to have to move to get to safety….he just wanted to sleep. Sleep deprivation is a “enhanced” interrogation technique utilized by our own intelligence services and known to induce psychosis.
I have experienced similar desires although not as a Marine or an MD. I functioned as a Perfusionist taking call, being up all night with ECMO patients, Transplants, etc, and there were many times I simply stopped caring about the patient because I had no mental or physical energy to give….I was spent and exhausted. I just wanted to sleep.
I can easily see how a Physician could easily become suicidal given repetitive incidents spread over years of this toxic type of work environment. The system is not blind, it is simply too mercenary to care.
I encourage you to explore it further.
MG
I’ve had some thoughts about the duty restrictions and started writing a response to your Friday post re the duty hour petition… and lol yikes my response got long, and included my personal experience tangents that I do have a point in stating and tying back to my opinions on changing duty hours back… but anyways so below I cut and pasted the response I was typing up. Thought you should read it first
I can only speak from my personal experience in training, which crossed over the years when duty hours changes were being made. My rotation years as a medical student were from 2010-2012 and we had no restrictions; an example, my very first rotation as a Med student was OB where I did 32 hour shifts.
New Duty hour restrictions for residents began in 2012, my PGY1 year. I was a surgery resident, and the program I was at had done a really good job at creating appropriate shifts for residents, and I never had to do a single note or chart at home (that’s when dictating was allowed and they were strict on timeliness of dictation prior to shift ending. This was great; it taught us how to learn to become efficient and also to never be behind in charts).
I transferred into a Family Medicine program my PGY2 (2013-2014) year, same restrictions in place… and the experience in regards to shifts and abuse of the junior residents was shocking. And this was family medicine, not surgery. Not many cared if a resident lingered around for hours to complete notes. Attendings/ seniors that ‘maybe cared’ would say ‘if you have to complete charts after your shift you can’t be visible to other faculty and staff because of duty hour restriction’.
Every night during my time in that program I had charting to do in the evenings up until I finally made it to bed.
As for residents reporting number of hours spent working, lol yeah the residency tells you how to answer that to. They basically state the message that if residents have frustrations with hours or anything with the program, to not take your emotions out on these national surveys because that only hurts the program in the long run, such as a program ending up on probation. And who wants to graduate from a program in probation? Or piss off the program director and attendings whom hold all the power to the fate of your future career in their hands?
And this I know for a fact is true, because during my time in the FM program, I eventually sought out legal advice and representation because of the extreme abuse going on at my program.
Did you know that residents do not have any legal rights such as an employee does? In Law, a resident is seen or classified such as a student would be, not that that means anything, just how my lawyer explained it to me.
Did you also know that there are no regulations, or strictly enforced ones atleast, requiring documentation of a residents entire in-training experience?
Your faculty can make up ANYTHING about a residents training, good or bad. This absolutely happened at my program. It was horrible.
Also, yes residency programs across the nation are bringing in new mental health resources for residents in a program, BUT no one at a university, such as the GME, regulates if a
Program Director is actually utilizing and referring their residents to these new mental health resources. And I can also speak from my personal experience that that was an absolute fact going on at my program. Absolutely horrifying.
But on a more reassuring note, once the University GME Director found out about this happening within the FM program, an emergent meeting with all staff and faculty was made to take place 24 hours after the fact, canceling clinics etc because attendance was strictly required, and I remember all the faculty and staff gone, in a four hour lecture given by the GME Director, reviewing all the policy and procedure regarding mental health concerns for any resident, medical, and faculty and staff of a program.
Also at this time, the PD was asked/required to resign at the end of that year and the GME Director made it mandatory for the program to appoint a new program director within 30 days during the time this all happened.
Over the years I’ve been wanting to write out the things that happened to me during my experience in residency.
And I have thoughts on what really needs to happen in this country (and world) to effectively intervene and begin to hault this epidemic of losing our doctors.
“Regarding insane hours which doctors are required to work during their residency: If an airline pilot worked those hours they would lost their certification. If a truck driver worked those hours, they would lose their license (if they survived). [In the past, some may have, but according to a well informed source, federal mandated electronic monitoring of long haul trucks will render that difficult if not impossible.] During emergencies, utility line workers sometimes spend as much as sixteen or twenty hours (according to recent issue of Ruralite magazine) to restore service. The widow who once lived down the street told me that her late husband and his partner would work until they couldn’t anymore, then sleep in the truck for a few hours, and work some more. But (to my knowledge) none of these professions require trainees to work 24 to 36 hours continuously, and regularly, as part of their training. How can people with such a sleep deficit be expected to make reliable decisions, especially life and death decisions?
`That’s how we have always done it’ can never justify continuing a bad practice.
As patients should take responsibility for our health. Any of us could probably do more to avoid damaging our bodies. Far too many expect health care professionals to provide some magic pill to cure any and all ailments, often after decades of neglect. Several decades ago, public television broadcast a series (five part I recall – still have the videotape, but haven’t viewed it in years) in which someone commented that we spend five, six, or seven decades abusing our bodies, then another decade attempting to undo the damage. On the other hand, companies spend billions annually urging us to do things which will be detrimental to our long term happiness and well being. Physicians should not be discouraged when they can’t overcome the adverse consequences of this situation.
Have you seen recent reports that life expectancy in the USA has declined for several years? These did not surprise me, as I’ve heard it before, and in my practice doing trusts, wills, and settling estates saw a surprising number of cases in which elderly people had outlived some or all of their children, children who died of natural causes, even as younger senior citizens. A couple of decades ago, I had a delightful neighbor who, when she moved to Arizona to live with her son, had outlived four of her five children, all of whom died as adults of natural causes. Her early life was not easy, by modern standards – it was `BE’ – before everything, including electricity. She said that her mother lived to 85, father died as week short of 100 years. Both of them had endured an even less easy life.”
I am a newly retired high school English teacher (almost 30 years in Houston,Texas). My psychiatrist killed himself???? My heart is broken for him. He gave so much to his patients. I haven’t a clue why, but reading this article, I can only imagine his inner demons. My friends who were patients of his are numb too.
I once was forced to work 68h without sleep.
Started at 7am on day 1 and was on call through the night with non-stop work and no sleep. Continued on day 2 and was on call through that night too with non-stop work and no sleep. On day 3 I drove back home at 5pm at the end of my day shift. Very dangerous drive back home. I skipped dinner and as I was crashing in bed, my chief resident called me at home asking me why I was not at work, as I was apparantly on call that night too. I told him I had been awake for 58 hours straight and was barely lucid. He told me to get back to the hospital STAT to do my call shift. I drove back to work, another very dangerous drive, barely awake. Worked non-stop until 3am, when I just collapsed from exhaustion. Total time forced to be awake: 68 hours. When I woke up around 8am, I immediately looked at my pager expecting 30 missed calls. Fortunately there were none.
I went to survival school (the AF makes anyone that flies in things go to this 3-week survival school in Spokane. During that time, one of the forms of torture they do is sleep deprivation.
Fast forward to a stretch of 7 days I just did. I knew it would probably be less-than-ideal, but had no idea how bad/unsafe things would be. It was awful. I was on call the first & last days, as well as 1 more day than my colleague (it was 7 days, so one of us had to do it). I got called all night, 5 out of 7 nights (once you’re there, you’re on call 24/7 for your own patients). Literally none of the nighttime calls were about medical issues that couldn’t wait until the next day. I talked to the house super – didn’t help at all, probably just made staff angry. My counterpart almost never got called.
The last night I made 2 fatigue-related mistakes, and thankfully no one got hurt. So I then had to meet with the CMO and risk management where they basically berated me for my behavior. Not that I’d ever go back there but I wondered if they would pull my credentials and I’d now have to report this for the rest of my life. Only later (after I’d had sleep!) did I realize that the AF recognizes sleep deprivation as torture, yet this hospital knew about this, knew it had been an issue with many physicians before me, but took no steps to correct anything. After sign-out at my last day, right before my meeting with the CMO, I was told about two things (an orientation packet another doc made but we were never told about, and the fact that I shouldn’t have admitted half of the patients I had, over the week – they belong to other specialties or should have been an ER-to-ER transfer for services unavailable at that hospital) that would have cut my workload by at least a third, maybe half.
This is a big part of what makes me want to run my own clinic. I never want to be in that position ever again.
I totally support. If 16 hours is not good, it should be reduced to 8 hours like all the other professions. They should not take this as it is a normal practice. If they don’t get enough sleep, it is not safe for the patient as well.