Ripple effect of ONE doctor suicide. How many people are left behind . . .
Two weeks before her son was born, my physician friend’s obstetrician killed himself. Left behind his wife, three kids, and my friend.
Eighteen years later, she still grapples with why.
Today a widow writes me:
“How do I stop carrying the guilt of this loss? Of not noticing the signs? It is killing me. I am slowing deteriorating. My husband, a beloved pediatrician of 45 years, killed himself by firearm in our home. I don’t know how I failed to see the signs that he was struggling mentally. I have not been able to find any peace or purpose.”
Three years after his suicide, she still grapples with why.
Since 2012, I’ve received hundreds of letters asking me to explain why a specific doctor chose suicide. I’ve categorized my responses in Physician Suicide Letters—Answered (free audiobook).
In the book, a patient shares the loss of her small-town Washington obstetrician/gynecologist:
“I am still in a state of shock hearing that my brilliant, loving, compassionate, successful, well-respected, honest, hard-working physician committed suicide this past week. Pressure from the changing medical community and insurance [system] had forced him to close his thirty-year practice and he went home and shot himself in the head. The letters keep coming in of how many people loved him, were healed by him, and admired him. What a tragic end to a successful career. He was the best of the best, surgeon and specialist, nice home, nice family and now he is gone. Everyone is asking why. ”
A year later, she writes me again:
“Recently I made an appointment with one of his associates for my yearly exam and am hoping that perhaps she will be able to shed some light and help me understand why . . .”
Today, eleven years after his suicide, she still grapples with why.
Why would a doctor who took an oath to save lives, kill a life? Why didn’t I see the signs? Why can’t I stop asking why?
Perpetual whys lead to prolonged grief, anxiety, depression, even suicide (often by the same method) in hopes of reuniting with the deceased to finally understand why.
To prevent future suicides we must support loss survivors. One way is to answer the perpetual why. Suicidologist Edwin Shneidman coined postvention as prevention of the next generation of potential suicides.
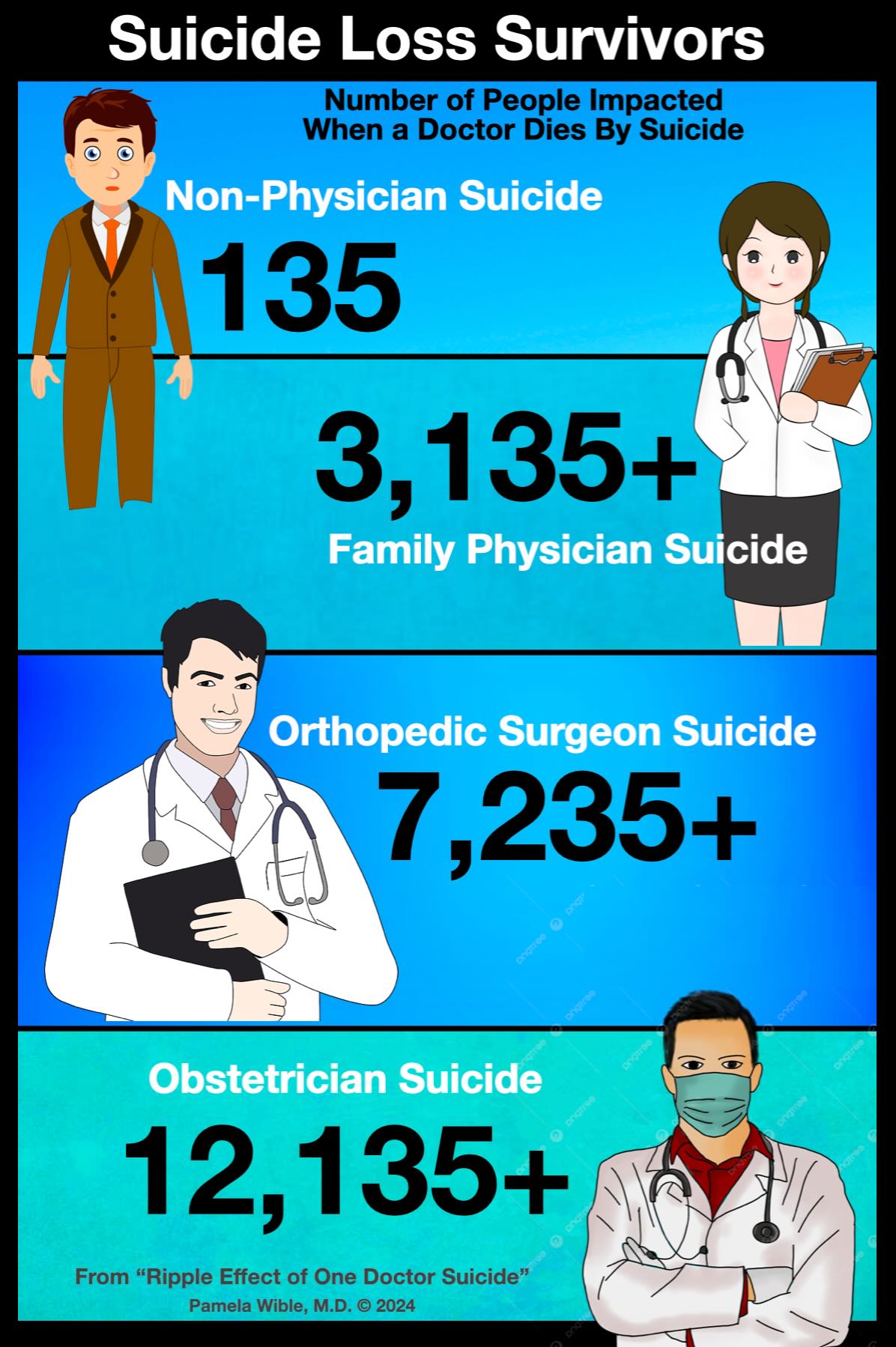
In 1973, Shneidman stated one suicide greatly impacts six people. His focus was on family members; however, 2019 data reveals one suicide impacts 135 people.
Loss survivors after a doctor suicide are exponentially higher.
Suicide loss survivors are all who knew the person or were exposed to the suicide.
One doctor suicide leaves not only 135 friends and family, but many thousands of grief-stricken patients.
Exact numbers depend on specialty and patient panel.
A patient panel is an economic term for the number of unique patients seeing a doctor in past 18 months; however, that’s an underestimate of loss survivors since patients who’ve not been seen for years may still feel great loyalty to their doctor.
In 2012, average US family physician patient panel was estimated at 2,300 and increasing.
Ten years earlier as a family physician employee, I cared for a patient panel of 3,000. Had I died by suicide, I’d leave 3,000+ patients and 135 family/friends. My loss survivors: 3,135+
In 2021, I led a postvention at a Memphis orthopedic clinic after their founding physician’s suicide. He had a patient panel of 7,100+. Including family/friends, his loss survivors: 7,235+
Loss survivors for obstetricians are even higher. Some deliver 10,000+ babies in their career. One doc delivered 40 babies monthly, 14 in one day. The small-town Washington obstetrician/gynecologist in my book delivered 6,000+ babies. Add the mothers and that’s 12,000+ loss survivors (not including his non-obstetric gynecology patients). Add 135 family/friends and the low-ball loss-survivor estimate: 12,135+
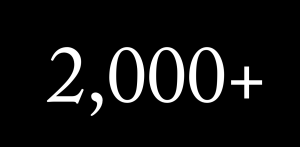
In 2014 curious about the total number physician suicide loss survivors, I multiplied 400 US physicians who suicide annually by 2,500 (family doc panel guesstimate).
The result: 1 million Americans lose their doctors to suicide every year.
Shocking that 1 million is still an underestimate. Adding specialist loss survivors to the mix may exceed 2 million.
Last week I led a small physician retreat on the Oregon Coast to discuss how we might stop doctor suicides. Walking along a desolate stretch of beach, we asked a couple to take our photo. When questioned why we were visiting, we shared our intention to end doctor suicides. Married 58 years, he and his wife were vacationing from a small town in Washington.
“I know a doctor who died by suicide in your town,” I shared. “ An obstetrician.”
Tears welled up in her eyes as she replied, “He was my doctor.”
💔
Special request: If you’re a doc, please share the number in your patient panel in comments. All these people would surely miss you! Need help? Join our confidential peer support.
Video from our retreat to end doctor suicide
Pamela Wible, M.D., is a suicidologist who runs a free doctor suicide helpline. She investigates doctor suicides and eulogizes victims to ensure their lives are celebrated. Dr. Wible performs psychological autopsies and provides postvention crisis support at hospitals and clinics to prevent future suicides.











2500
What’s your specialty? Internal medicine I believe (from a quick search).
Per this article: Primary care faces a dilemma. On the one hand, the average primary care physician’s panel size is too large for delivering consistently high quality care under the traditional practice model. Estimates suggest that a primary care physician would spend 21.7 hours per day to provide all recommended acute, chronic, and preventive care for a panel of 2,500 patients. The average US panel size is about 2,300. On the other hand, the decreasing number of physicians entering adult primary care—in part due to the excessive work of primary care physicians, which dissuades US medical students and residents from choosing primary care careers—means that panel size will increase, particularly as more people have insurance coverage and seek access to a primary care medical home.