We go to the doctor when we are sick. But what happens when doctors get sick? Who cares for them? All too often, physicians are threatened, harassed, even terminated for being ill. After reporting on a psychiatrist fired for having cancer and a pediatrician bullied for her brain tumor, I’ve heard from many more physicians who are now courageously stepping forward to tell the truth. In their own words . . .

Andrea Seiffertt, D.O.
I got a migraine with aura on NICU [Newborn ICU] call. I literally couldn’t read the orders and had to call over my resident, and tell her I had to lie down in the next 10 minutes before the pain hit or I’d be unable to work later. They left me alone for a few hours, grumbling. After I’d slept a half hour or so, they said, “examine this new one” and pulled me half asleep to a cold, turned-off open warmer with an unwrapped baby inside. He had gastroschisis [birth defect of abdominal wall in which baby’s intestines are outside of the body] , and I didn’t in the first moment realize he had already died, and wasn’t given any history or story, just handed the form. My impression was only of his perfect and sweet smaller-than-term face, his ruined middle, and how he was blue and cold and too stiff, with amniotic banding on one arm and leg. After that first second I realized what had been done to me, and was horrified and tried hard not to cry. That was the only moment of serious hazing I ever experienced.
Dario Lizarraga, M.D.
I’m a family medicine doc and during one of my OB/gyn rotations I came down with pneumonia. The OB attending refused to let me leave. I was running a fever of 104 so they just gave me Tylenol and put an IV in my left hand to keep me hydrated between deliveries. I would just double glove to protect myself. As the night wore on I became worse and my own family medicine attending saw me and proceeded to give me Phenergan IV and told the OB attending that I couldn’t work anymore. She called my wife to pick me up and take me home. If not for that one act of kindness I would have had to stay and deliver babies while sick and the go to gynecology clinic the next morning working a 30-hour shift. The next day, I saw my doc who prescribed antibiotics. My OB attending was so furious that I had extra work to do the rest of my rotation.

Anna Hollenbeck
After my emergency C-section, when my son had gone into fetal distress after getting caught, and they ripped apart my abdominals, they had to carry me, bleeding, up and down 4 flights of stairs to attend school because I’d be failed if I didn’t show up. I shouldn’t complain, though. There was another student a few years back with an aortic dissection and half of his internal organs lost blood supply and had to be removed. The school was kind enough to allow him to continue his opiate pain medication while attending classes. Eventually, he ended up dying. All of these events seem almost surreal. Medical education is cruel…

Susan Haney, M.D.
I had a meningitis (proved by spinal tap and hospitalized for 3 days during my second year of residency). Subsequently developed some depression, worsened by the fact that I initially complained about my residency program requiring me to “pay back” the 3 days of work I missed while hospitalized (to work 3 extra shifts on my days off). I complained because I was contractually entitled to sick leave. These were the only 3 days of work I missed over a total of 5 years of residency. In return for complaining, I was told a couple of months later that someone had noticed my attitude had changed (it had) and my knowledge base was deficient (it was not). I was asked to submit to a random urine drug test (which of course I passed). I told my residency director that yes, my attitude had changed—I was depressed about how the program was treating me—and that I agreed I would benefit from some counseling (which I arranged for privately, without further interference from my program). The following month, I tested in the 98th percentile nationwide on my residency in-service exam (higher, in fact, than any other resident in my program). It turns out that my perceived “knowledge gap” was real: I knew more about Emergency Medicine than some of my upperclassmen. When test results returned, their criticism stopped.

Lane Baker, D.O.
In med school I had viral meningitis during a 4-week rotation at the place I wanted to do my residency. Week two I had a pounding headache, fever, intense neck pain. Tried to work through it with Tylenol. I may have mentioned it to some of the residents, but if I did I downplayed it. The start of the third week I was barely holding it together. I was a first assist on a C-section and had about a 102 fever and dripped sweat into the patients open belly. At this point they were concerned and also pissed. I was sent home until medically cleared. The disease got worse from there, BP 79/30 tachycardia. Well a spinal tap later some fluids and tampering with the bp machine I avoided their recommendation of ICU admission and went home. I took the remaining week and the next off but started the next rotation on time. Had to make up the two weeks at the first place over summer break. I felt the main “lack of support” is the whole environment of “do not seek help.” If you do you will be looked down on as weak and unworthy. My attending told me he worked until his appendix burst and he collapsed. This was given as an example of a “good work ethic.” In residency I had Guillain-Barré. Not horrible I never had to be on a ventilator. I could not use my hands as they were nearly paralyzed. Walking I would have to lean to get momentum and even then it was difficult. Chief resident joked and “called” that he gets to intubate. They were trying to figure out how I could take call if I was any worse. I took no time off during that illness, again viewed as weak if you did. Damn I was just thinking I also had a mental health issue—depression mainly and anxiety. Here is the help I got for that: after morning rounds and lecture I was told to go into a room and make zero stops. I was met in the room by my superiors who said, “You have been acting different and have been reported by a nurse for acting not like yourself. We are going to follow the impaired physician protocol. You are to leave the premises now. Go from here to this address and do a urine drug screen. From there you will submit to a psych evaluation. If you refuse you will be suspended and sent home and possibly terminated.” I didn’t feel much support. By the way, no drugs. My diagnosis: depression and anxiety.

Michelle Catena, M.D.
One of my classmates was dragged by a bus. A second was struck, flipped, left on the road in a hit and run when crossing the street. Our med school had people taking attendance by the number on the back of your chair. The first person had to be in her seat, scraped, bruised, bloodied, in pain. The second had to get special permission to be absent while admitted to the facility hospital. They wanted him in his seat to take tests and then return to the hospital. He was finally allowed to take his tests in the hospital. Even my residency program director did not allow anyone to be absent for illness. It’s a disgrace. A severely ill student missed a few weeks. She was forced to repeat and ended up leaving. My tale of having severe food poisoning the night before a final and not being able to take the final at another time is trivial in comparison. I was pretty much passed out and delirious taking this final. But if you don’t show up, you are automatically failed.
Is this how our doctors should be treated?
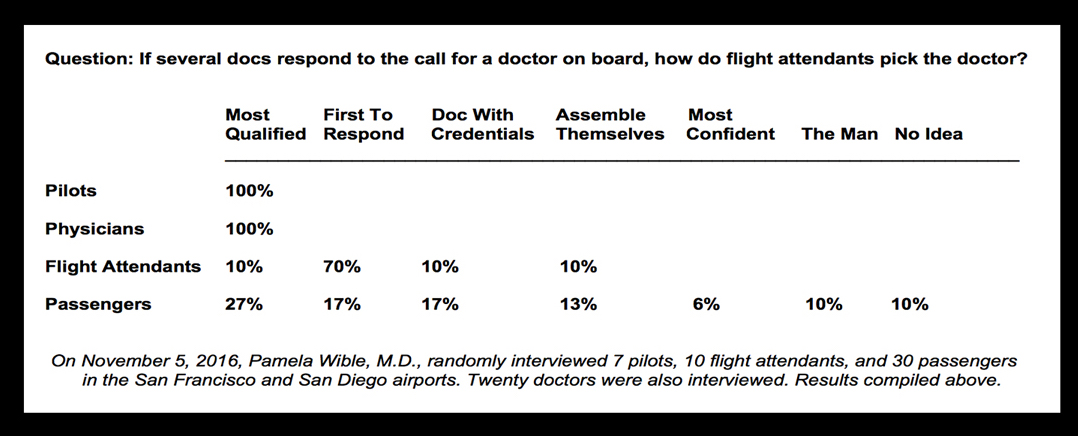
Pamela Wible, M.D., reports on human rights violations in medicine. She is a practicing physician in Oregon where she hosts physician retreats to help doctors heal.