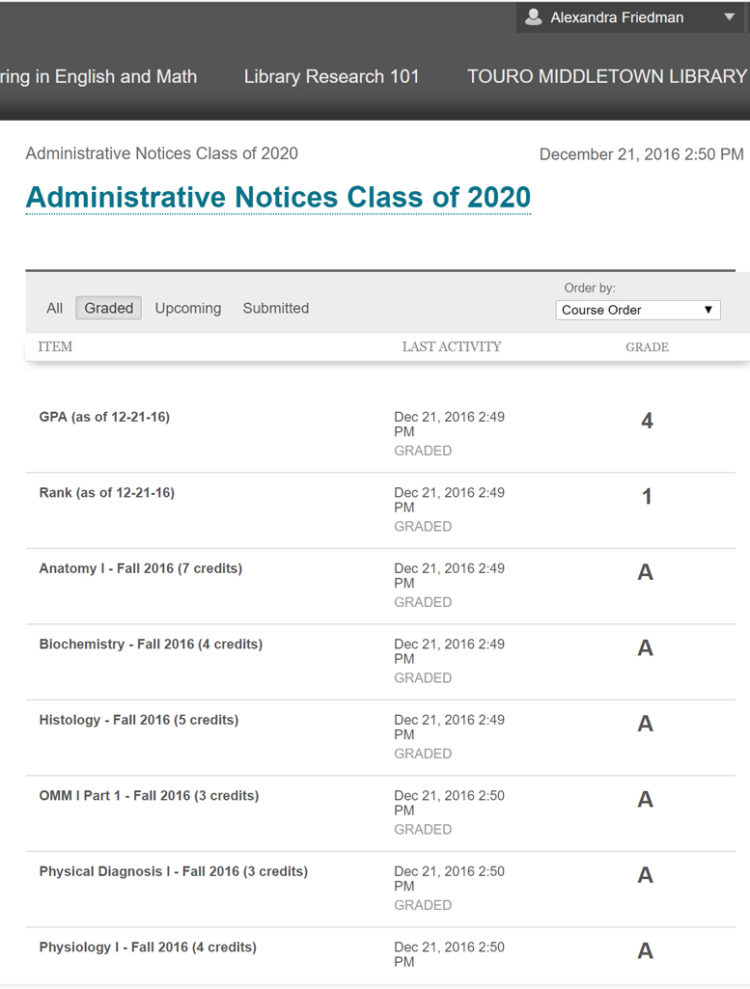
Alexandra Friedman has been awarded $10,000 as the recipient of the 2017 Judith Wible, M.D., Scholarship for Visionary Women in Medicine. She is a first-year medical student at Touro Osteopathic Medical School in New York.
In her own words . . .
Why do you want to become a physician? I have felt since I was a young child that being a physician was one of my life’s missions. Although it is not the easiest or most lucrative path, I have never been able to separate myself from the identity of being a physician, so I feel I am meant to practice medicine.
Describe your ideal practice: I’d like to have an integrative family medicine clinic, working alongside therapists, life coaches, acupuncturists, and other health professionals, all in the same building. We would refer to one another and have team meetings to optimize care for our patients. I’d help women feel empowered to experience natural childbirth (at home or in the hospital). I will offer culturally-sensitive programs for victims of sexual abuse and promote the benefits of integrative medicine (including osteopathic techniques) for trauma healing.
List the top three reasons why you need this scholarship: (1) I’m interested in being the best physician I can be and I’d like to hear Dr. Wible’s thoughts on how to do that. (2) Med school is never easy, and for a non-traditional student with children it can be even more difficult, so I’d like inspiration from like-minded people which I would get by participating. (3) I have a family of nine and we are living on student loans meant for a single person plus my husband’s minimum-wage 36-hour/week night job, so I cannot afford to pay for med school on my own.
Wow. I’m blown away that anyone can feed nine people on student loans, follow an ultra-orthodox lifestyle, and excel in med school—so effortlessly!
When I notified Alexandra that she was a finalist, she wasted no time organizing her schedule, family responsibilities, and limited finances to fly out to Oregon and attend our medical student retreat on full scholarship. She even brought her own kosher food. I’ve never been good at meal planning so I was especially impressed. (I could barely remember to put fresh water in my dog’s bowl during med school.)
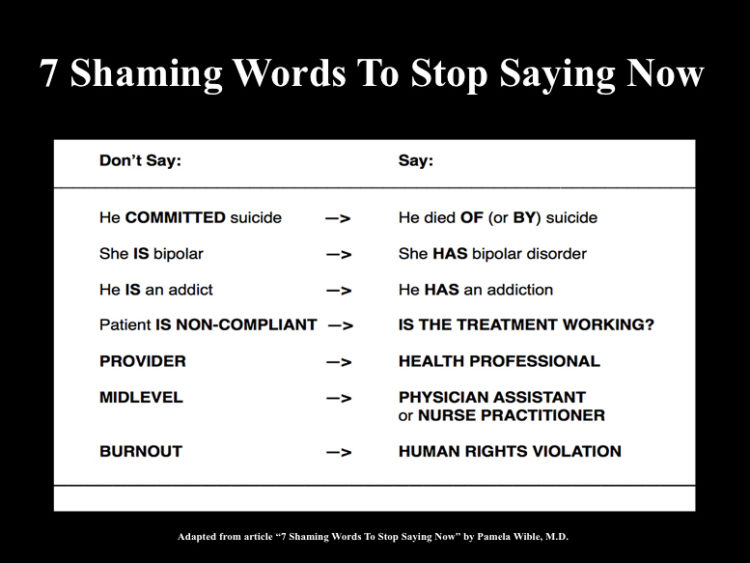
Then, in August 2016 (just a month into her first year at her second medical school) she organized a solidarity vigil for medical student and physician suicide awareness. Alexandra invited me to speak at this event and since I was already leading a vigil in DC, I took a train up to New York to talk with her classmates.

I met her husband and her youngest child when they picked me up from the train station and I got to witness firsthand how she has mastered the art of work-life balance as a devoted wife, mother, and future physician:
“I don’t study on Shabbos so that I can take 24 hours each week to focus on my spiritual well-being and connect with my family. Also I pray/meditate daily, I regularly read books, especially personal development and spiritual books, I eat vegan during the week, and always sugar-free to take care of my physical health. I eat dinner with my family every night and generally don’t study in the evenings in order to spend time with my family.”
Please join me in congratulating Alexandra Friedman—our 2017 Visionary Woman in Medicine.
Check out the cool thank you card from her kids!

Images courtesy Elnaz Mahbub, Alexandra Friedman and her children.