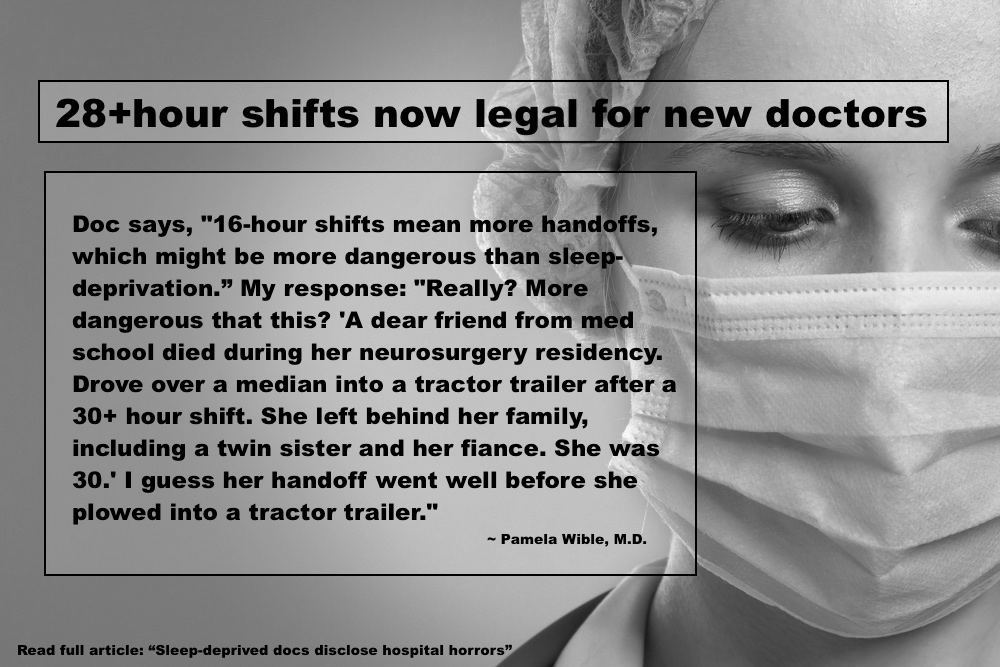
Today the ACGME (Accreditation Council for Graduate Medical Education) made the reckless decision to increase work hours to 28-hour shifts for new doctors. Here are the catastrophic consequences of their decision. Here are actual quotes from physicians (de-identified with some patient details changed to protect confidentiality):
“I did my internship in internal medicine and residency in neurology before laws existed to regulate resident hours. My first 2 years were extremely brutal, working 110 – 120 hours/week, and up to 40 hours straight. I got to witness colleagues collapse unconscious in the hallway during rounds, and I recall once falling asleep in the bed of an elderly comatose woman while trying to start an IV on her in the wee hours of the morning.”
“I ran a red light driving home in residency after a 36 hour shift. Got pulled over. It was sobering: I was not fit to use my driver’s license, but I had just been using my MEDICAL license for over a day non-stop!”
“I have made numerous medication errors from being over tired. I also more recently misread an EKG because I was so tired I literally couldn’t see straight. She actually had a subarachnoid hemorrhage and by misreading the EKG I spent too much time on her heart and didn’t whisk her back to CT when she came in code blue. She died.”
“After a 36-hour shift, I fell asleep and began dreaming while walking home—repeatedly. It was a four-block walk.”
“I fell asleep multiple times at the light at the intersection right at my neighborhood after call. I would see home was close and relax just enough. I had a baby and I was so afraid of forgetting him in the back seat if I ever had him with me I would put his bag in the front with me and my stuff in the back with him. Luckily, nothing bad happened in either situation but I just got lucky.”
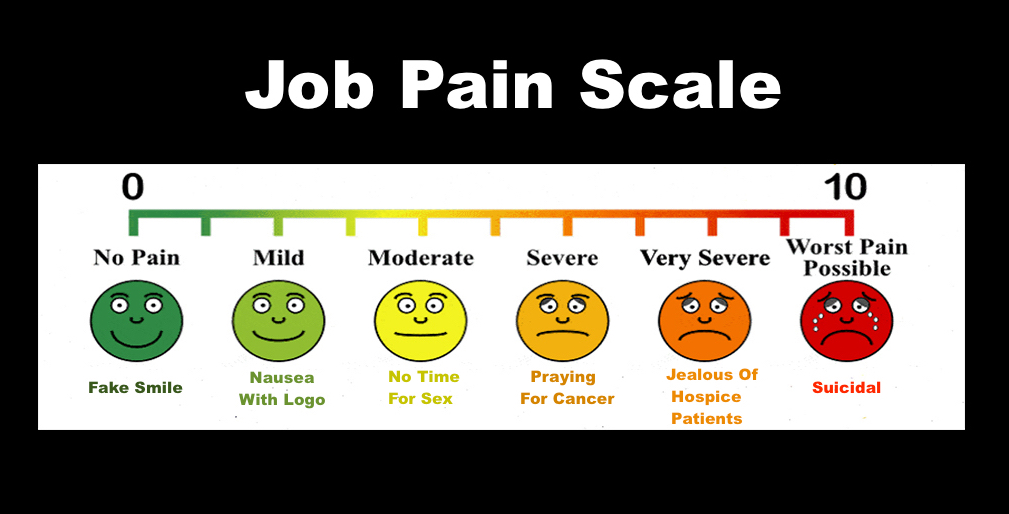
“As a resident in a surgical specialty, my program routinely violated work hours, yet our attending physicians kept talking about how lucky we are because we have “work hour restrictions.” To fool my brain into not stopping, I’d lie to myself. I’d tell myself that if I just got out of bed at 3:30 one more time I could go to bed early that night, or if I just got through a few more notes I could go home and finish the rest tomorrow. I thought I could just keep going at that pace and nothing terrible would happened until I woke up in the ICU and a doctor told me I had tried to kill myself.”
“In general surgery residency I had one week in which I worked 125 hour….I did a weekend of 72 hours in which I only got 4 hours of sleep. I would secretly hope to get in a car accident and maybe break a leg so that I would be forced to take off from work…just so I could get some rest.”
“During intern year at a program with a nominal 80-hour work week, I worked 100 hours per week for most of a month. I was interviewing a patient when I suddenly realized that I could not remember what I had just asked. I excused myself abruptly and rushed down the hall where I collapsed on the bathroom floor. I leaned against the wall and felt relaxed for the first time in weeks. My face was wet and I realized I was sobbing. I was so unaware of how exhausted and impaired I had become. I cried because I was tired, and also because the patient I was seeing deserved better attention and care than I was capable of providing. I couldn’t remember any details of his chest pain or risk factors for heart attack. I couldn’t even remember his name or his face. Only that he was friendly and he trusted me. I felt intensely guilty for not being able to stay awake, let alone think like a doctor. I nodded off while crying, propped up against the wall. I woke up and forgave myself. I think I was away from him for less than 10 minutes. I walked back into his exam room and said, “Where were we? Let’s start at the beginning to make sure I get this right. Because what you are saying is really important.” That month during my evaluation, my program director told me that my total number of work hours was a sign of inefficiency. I later learned that others were also working 80-100 hours per week but they falsified their hours to avoid criticism.”
“I have fallen asleep at the wheel thousands of times since medical school. I literally would wake up the next day in my work clothes and not even remember leaving the hospital. I drive from 45 min to 4 hrs to rural hospitals now and in training, currently working up to 7 straight 24’s in a row.”
“I was post call after a 30-hour shift and rear ended a car while driving uphill. No one was hurt but I remember the guy saying ” you hit me driving up hill.”
“I was so sleep deprived that I’d fall asleep while writing patient notes and write my dreams into the notes. I’ve fallen asleep on a pile of charts only to have the nurses cover me with blankets. I woke panicked because I was hours behind in my work. I’ve fallen asleep standing up in surgery and witnessed my attending doctors fall asleep while doing surgery. I actually passed out at the end of a 36-hour shift and woke up on a stretcher in the recovery room.”
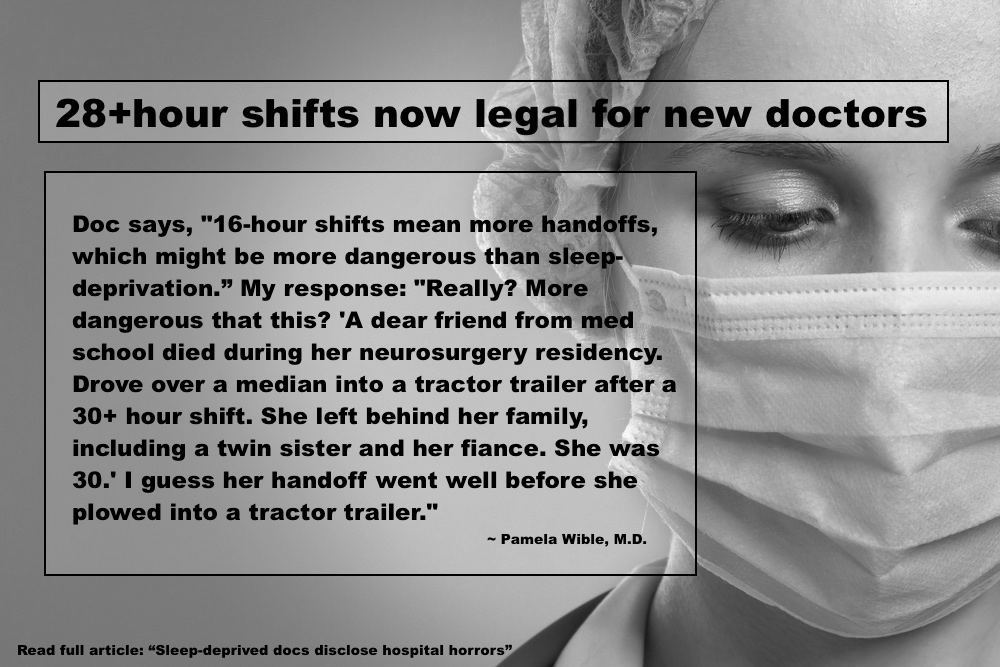
“A dear friend from med school died during her neurosurgery residency. Drove over a median into a tractor trailer after a 30+ hour shift. She left behind her family, including a twin sister and her fiance. She was 30.”
“I had married the year before residency, and for that first 2 years, I was either at work or asleep, so didn’t see my wife, and it was the start of the erosion of the relationship that led years later to divorce. I also suffered permanent health problems from extreme sleep deprivation. Prior to residency, I slept fine (8 hours/night) and had regular bowel habits. Since my internship, I developed lifelong severe insomnia, and went for decades on 4-5 hours of sleep/night, as well as severe constipation, using the toilet about every 5 days.”
“I was at one of the most humane programs in the country, yet as an intern and I would frequently gag on water while trying to drink. I knew by then that stroke patients and others with neurologic impairment had swallowing problems. Mine always went away while working less than 50 hours per week.”
“During internship I was driving home after a 30-hour call. It was dark and rainy out. The usual road I took home was closed, so after some roundabout driving I got on to the garden state parkway in NJ going in the wrong direction. Thankfully a police car saw me and pulled me over as I realized I was going into oncoming traffic. He escorted me all the way home.”
“I was working in the NICU and commuting 45 miles each way to and from the hospital when I was involved in a serious car accident in which my car was completely totaled. My program directors were upset that I did not make it back to work the next day (as I had to deal with insurance, get a rental car, etc.) Before this, I had a perfect driving record.”
“I was struck down with a very severe depression in the context of emotional conflicts and severe sleep deprivation, after doing a surgical rotation with every other night call and lots of degrading comments from the surgeons recommending that I go into nursing or teaching instead since those were “good professions for women.” This was 1983. I was supported in the sense that I missed 6 weeks of medical school without censure while I was too debilitated to move physically. I spent those weeks mainly sitting in a corner of my apartment, crying, and seeing my psychiatrist once/week for therapy and meds.”
“I have gained easily a hundred pounds over the years in part from eating to stay awake. The state police have woken me up on the side of the road many times when I pulled off the highway to sleep because I couldn’t stay awake until the next exit.”
Are these the doctors you want to see in the hospital? Protect yourself and your loved ones. Always ask, “How long have you been on your shift, Doc?”
Let the ACGME and Dr. Thomas Nasca know how you feel about their decision to allow doctors to work 28+ hours without sleep: Accreditation Council for Graduate Medical Education 401 North Michigan Avenue, Suite 2000, Chicago, IL 60611 or call 312.755.5000. Email Dr. Nasca: tnasca@acgme.org
__
Pamela Wible, M.D., reports of human rights violations in medicine. Have a story? Contact Dr. Wible.