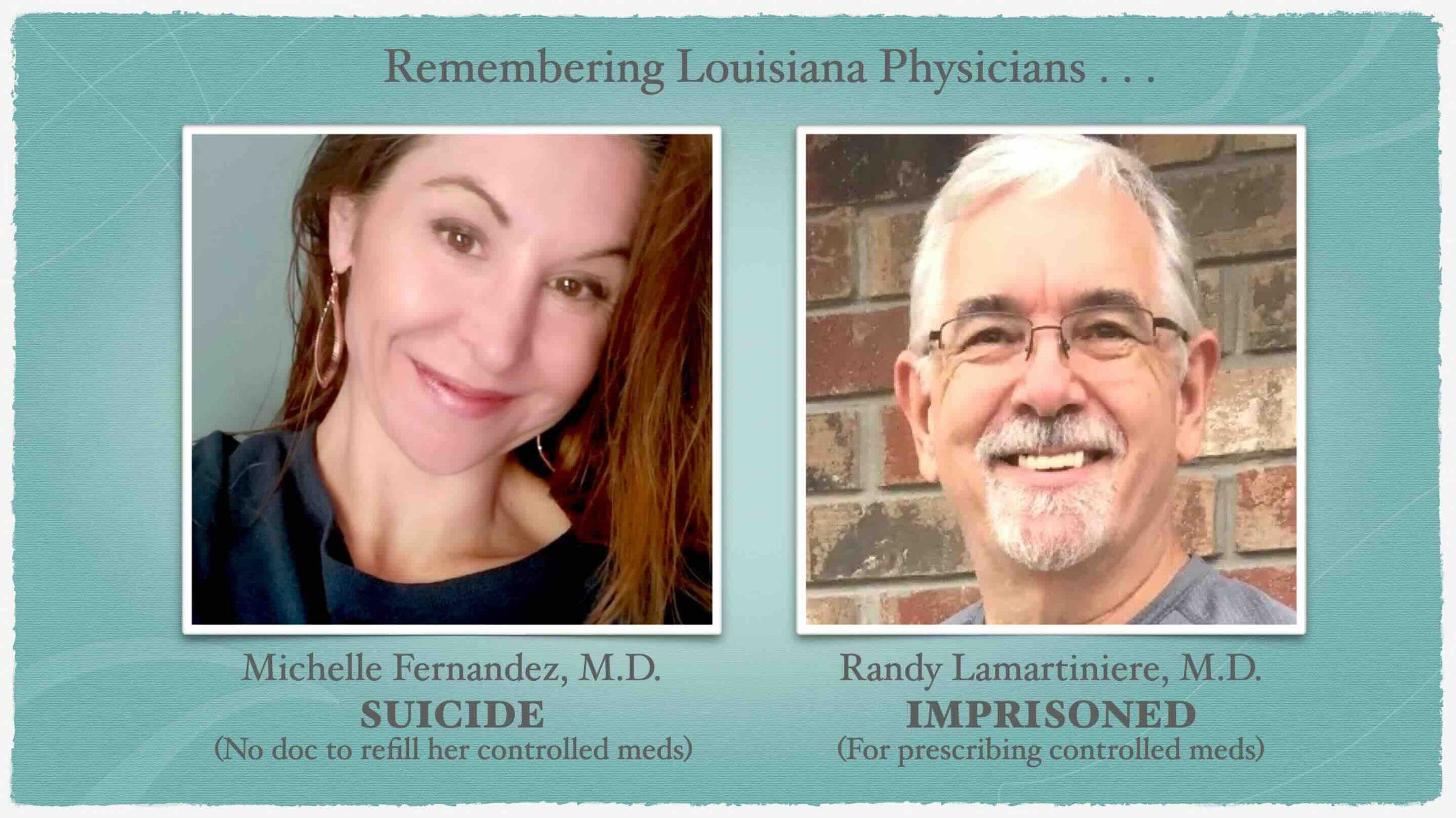
In 2023, I lost two dear physician friends. To overzealous DEA agents.
Michelle, a stellar emergency physician with well-treated depression/ADHD for 20 years couldn’t find anyone to continue her meds when her doc retired. Depressed, she shot herself Christmas Day.
Randy could have saved Michelle. But he was in prison for prescribing the meds Michelle needed to undercover DEA agents.
Physician entrapment is the act of tricking a doc into committing a crime to secure prosecution.
Thirty years ago, we were trained to treat all pain.
“In the mid 1990s, certain pharmaceutical companies funded non-profit organizations focused on pain management, which led to the belief that the medical community was undertreating chronic pain . . . the Federation of American Medical Boards urged medical societies to punish prescribers who undertreated pain.”
In 1999, my own Oregon Medical Board was first to discipline a doctor for not prescribing pain meds. Now docs are in prisdon for treating pain.
In 2015 Randy attended my launch your ideal clinic seminar. An internist who left big-box medicine to care for elders, Randy celebrated his new clinic at our May retreat.
Weeks prior, undercover DEA agents began visiting his clinic. Matthew Dixon and Craig Crawford saw Dr. Randy Lamartiniere for nine separate visits April to September 2015. See USA vs. Lamartiniere.
7 tips your patients may be undercover DEA agents
DEA agents often:
1) Use slang.
“I’ve gotten a ‘couple of roxies’ from my friend that made me feel good.” ~ DEA Agent Crawford
Doc Randy replied: “Do you have any history of drug abuse? Your symptoms are really not something that any doctor should prescribe a major narcotic for.”
2) Take friends’ meds.
“I took some of my coworker’s ‘addies’ to help me stay awake.” ~ DEA Agent Dixon
Doc Randy: “Taking Adderall for that purpose is illegal and using Adderall to stay awake is non-indication for adult ADD.”
3) Claim a doc prescribed med in past.
“But another doc gave me ADD meds when I had trouble focusing.” ~ DEA Agent Dixon
Randy sought other solutions before reluctantly prescribing Adderall 20 mg.
4) Fill meds out of state.
“I filled my prescription in Texas.” ~ DEA Agent Dixon
“I filled my prescription in Mississippi.” ~ DEA Agent Crawford
Randy: “Louisiana’s PMP shows no record of you filling my last prescription. I can only give you one more prescription unless you return with records confirming you filled your prescription . . . they’re using people like you to catch doctors like this, so that’s why I have to be careful. I also need you to get an MRI of your back.”
5) Say prescription was stolen.
“I need another prescription because a guy stole mine.” ~ DEA Agent Crawford
Randy: “The only way to get another prescription would be to have a police report, but it is hard to get police to write reports on stolen drugs because they know that some people will use that to get more medication.”
6) Run out of meds early.
“I haven’t taken the meds you prescribed in several weeks because I ran out.” ~ DEA Agent Dixon
Randy: “I’m going to drug test you in order to ensure prescriptions are not being diverted. Unfortunately they treat doctors like they’re supposed to be detectives these days. They can take licenses away.”
7) Beg for higher doses.
“Do you have anything stronger that would last longer?” ~ DEA Agent Crawford
Randy: “Problem is all these pain medicines are addictive and people develop a tolerance to them which is especially concerning for someone that’s not really in a lot of pain as you said. . . . You must sign a pain management agreement or I’m not be able to continue prescribing your meds.”
Despite his hesitation, Randy prescribed Percocet 10 mg #90.
Never prescribe controlled substances to DEA agents.
Randy hoped to see a mix of elder patients for $100/month in his clinic. [Note: his cheap flat monthly fee ensured he was not earning money per visit or per prescription]. Because boards were sanctioning docs prescribing controlled substances, Randy got an influx of discarded patients. Within a year, he had 250 patients, eighty percent abandoned by other docs.
Many docs now refuse “high-risk” patients. To avoid entrapment, a few choose not to renew DEA licensure.
One pain patient testified Randy was “one of the hardest pain doctors” from whom to obtain narcotics.
So was Randy running a pill mill? Or was he too kind to deceptive DEA agents?
Randy reminds me of my dad. Both old-school docs upholding their oath to soothe pain of all who suffer. Like Randy, Dad even “lent” patients bus money. Had DEA agents visited my dad, I’m sure he’d be in prison too.
Randy’s not a street-smart police officer. No doctor is. Yet people-pleaser docs must think like cops when caring for undercover DEA agents.
I just mailed Randy a letter. Want to check up on him? Here’s his address and inmate number:
Randy Lamartiniere, MD
Inmate Number 09020-095
FCI Seagoville
Federal Correction Institution
P.O. Box 9000
Seagoville, TX 75159