Sometimes there are no words.
Not even a eulogy.
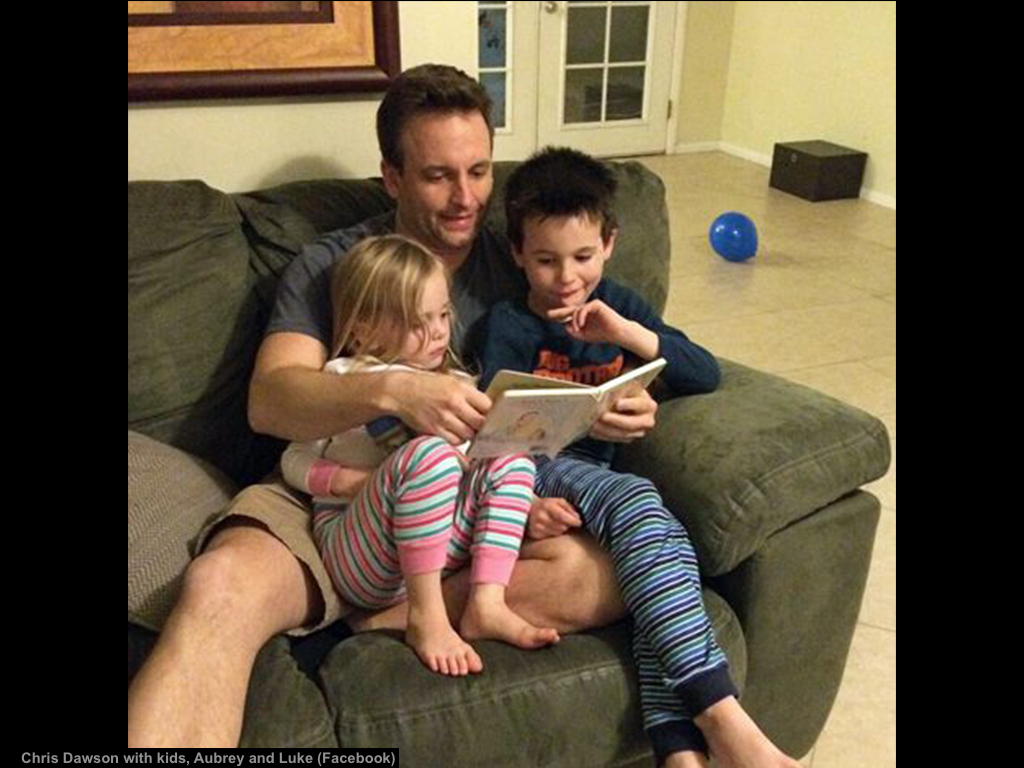
Then one courageous family writes this obituary. [This obituary was written by Rachel Dawson, his wife, with the blessing of his parents] In it they share how their son lost his battle with severe depression. How he adored his children. How he sacrificed fun, free time, and relaxation to receive his medical degree. How he took on the challenge of surgical residency. How he was so very damaged by his untreated anxiety, long work hours, and intense stress. How he attempted to self-medicate his hurt. How despite being an intelligent surgeon and a loving father, he did the unimaginable.
I first heard of Dr. Chris Dawson just hours after his suicide in a Facebook private message:
“My friend who is also a doctor’s wife is going through a nightmare at this very moment. Her husband graduated residency this summer along with my husband and he killed his two small kids and himself this morning. Her husband suffered from depression due to the difficulty of residency season and never recovered from it. I know residency is hard, I always said it’s a real b#%^*, but if you know your partner is having a rough time, suffers from mental illness or is going through a depression get him some help. At all cost! My heart is broken for my friend who no longer has her babies. This med journey can be very hard and can take you through a darkness if you don’t get the help needed. It was so close to home that I had to share. Mental illness is nothing to be ashamed of.”
I’m a doctor, a problem solver. I study human suffering so I can help people. That’s my job.
In 2012, I became alarmed by how many doctors were dying by suicide. So I started counting dead doctors. I began with a list of 10. Today I have 699.
Now I run a suicide hotline for doctors.
During the last 5 years, I’ve spoken to thousands of suicidal doctors; interviewed surviving physicians, families, and friends; and published a book of their suicide letters, I’ve spent nearly every waking moment since 2012 on a personal quest for the truth of why we lose so many doctors to suicide. Here’s what I’ve discovered.
Of the 699 doctor suicides I’ve compiled, only 2% (15) involve a homicide. Half of those (7) are male physicians who killed a female spouse/girlfriend (all in health care—4 nurses, a nursing student, pharmacy tech, and dentist). Three male physicians killed their young children. Another strangled his disabled adult daughter before killing himself. Less than 1% of all doctor suicides involve homicide of their children. Of the 3 cases involving young children, all suicide victims were having marital/relationship problems with the mother. One also killed the mother.
Why would a doctor dedicated to saving lives take his own? And the lives of his loved ones?
Many doctors write suicide notes explaining their motives. A few leave extensive documentation—even videos (often they are whistleblowers exposing fraudulent hospital systems). Still questions remain.
Motives for murders perpetrated by doctors often involve ending perceived suffering of others. Four of the 15 physicians were attempting to end distress in dependent family members prior to taking their own lives. They wanted to protect siblings from an abusive parent; to stop an aging mother’s misery; to prevent institutionalization of a severely disabled adult daughter for whom the physician was full-time caregiver; to end the suffering of a child tormented with the same anxiety disorder as the dad. None of these four physicians seem to have been acting with malicious intent when they took the lives of others before killing themselves.
So how do we respond as a society to these suicides? Often with an outpouring of love for the surviving family amid condemnation of the suicide victim mixed with lots of confusion.
And then comes silence.
Until it happens again. In the house next door. The one with the Christmas lights and candy canes. And the soccer ball in the yard.
Our collective rage resurfaces. We pray for the family to find peace. Then the story falls to the bottom of the news cycle.
Until it happens again.
And again.
‘Round and ’round and ’round we go.
I’ve read hundreds of doctor suicide obituaries. One common theme: euphemisms obscure the cause of death and prevent discovery of answers we so desperately seek.
Secrecy, shame, and silence are 100% ineffective as problem-solving strategies. They also prevent us from healing.
Full disclosure: I do not know Chris Dawson, but I feel like I do. Maybe it’s because I grew up in Dallas down the street from where he died. Maybe it’s because we both graduated from medical school in Texas and completed our residencies in Arizona. More likely it’s because we both fell into a suicidal depression at age 36. Since he can’t share his story, I’ll share mine.
From October 22 through December 7, 2004, I couldn’t get out of bed. For 6 weeks. I wanted to die. I prayed that I’d go peacefully in my sleep. Despite my pleas with God and the universe, I woke up each day horrified that I was still breathing. I could not figure out how to release myself from my unbearable pain. I was fed up with being forced to practice assembly-line medicine like a factory worker. I had just been let go from a job (contract nonrenewal “not a good fit”). I could not face one more day. My bills were piling up. My marriage was on the rocks. I felt like I was in a suicidal coma. If I had a loaded shotgun, I may have pulled the trigger too—and this story would be mine.
The fact is we all have a breaking point—a threshold over which we would consider killing ourselves. And even our loved ones (in our disordered thinking) as a mercy killing.
So what shall we do now?
Here are 5 ways we can prevent the next physician suicide
1) Increase awareness of our physician suicide crisis. Be alert to mental health risks of medical training and practice, including high-risk specialties for suicide. We can’t solve a problem nobody knows exists. Talk about it. See the forthcoming film, Do No Harm. View trailer here. To arrange a screening at your medical school, hospital, or conference, email info@donoharmfilm.com.
2) Avoid a medical career if you have pre-existing anxiety or depression. Medical training will worsen your mental health—and may be life-threatening to those who are not resourced to cope with chronic high pressure and ongoing exposure to suffering and death. In fact, 75% of med students are on psych drugs just to survive med school.
3) Allow access to nonpunitive mental health care. Physicians have unique occupationally induced mental health needs and currently risk punishment for help-seeking by state medical boards, hospitals, and insurance companies that may prevent a doctor from practicing medicine. If you are suffering, I’m available to speak with you and I can refer you to confidential care by phone or Skype 24/7. If you are in imminent danger please call 911.
4) Allow access to nonpunitive marital counseling. A physician friend had her state license delayed for 6 months because the medical board demanded to review her marriage counseling records because she was depressed during a divorce. Doesn’t everyone need help during a divorce? Why should physicians fear seeking counseling for their marriage? (Note: a lot of physician relationships fail because there’s no time to spend with your spouse when working 100+ hours per week!). One request: Please support Rachel Dawson who has lost her entire family.
5) Humanize medical training. Residency is brutal with chronic sleep deprivation and human rights violations (plus lack of legal protection). Surgeons used to brag about 100% divorce rates! (as if toughing you up and destroying your family would make you a better doctor). Let physician trainees sleep, eat, and see their loved ones. Doctors are human.
Doctors are extremely gifted, complex individuals. Most people attracted to medicine have brilliant minds and are able to tackle immense complexity. Yet the culmination of such intense personal and professional pressure contributed to this surgeon’s complexity becoming confusion and such horrific torture that he just had to end it all.
So how do we preserve our humanity? That was the one thing Chris was unable to do at that moment—preserve his humanity. He most assuredly loved his children and as a surgeon saved many lives. Though he saved lives, he may have been unable to feel fulfillment. Medicine conditions physicians to be withdrawn and professionally distant. For somebody like Chris who suffers with anxiety to be groomed for emotional distance and discouraged from seeking help is deadly.
We are all born into this world with our own eccentricities, quirkiness, and a certain predisposition to anxiety and depression. Nobody is immune.
Did Chris have pre-existing anxiety before medical school? Seems so. If he were a realtor or an auto mechanic would he have been able to access confidential nonpunitive care for his anxiety? Yes. Would he have been more resourced to assist his children with anxiety? Yes. Would he have had more time to spend with his wife and invest in his marriage had he not been a surgeon? Yes. Would he and his children be alive now? I think they would.
My hope is that this honest obituary allows us to begin an honest (and long overdue) conversation about mental health.
Because our silence nearly guarantees our suffering will continue.