“Have you ever been depressed as a physician?” I asked 220 doctors. Ninety percent stated yes. Yet few seek professional help. Here’s what depressed doctors do (when nobody’s looking). Some drink alcohol, exercise obsessively, even steal psychiatric meds. Still more shocking—I discovered that 75% of med students (and new doctors) are now on psychiatric medications.
“I was told by the psychologist at my med school’s campus assistance program, that 75% of the class of 175 people were on antidepressants,” shares psychiatrist Dr. Jaya V. Nair. “He wasn’t joking. How broken is the system, that doctors have to be pushed into illness in order to be trained to do their job?”
“During my internship, I found out that at least 75% of my fellow residents were on SSRIs or other antidepressants, just ‘to get through it’ because it was so horrible.” states Dr. Joel Cooper, “Depression, or a constantly depressed state, is more or less the norm in medical school and throughout one’s residency.”
“When I left my residency, I was alarmed to find out that about 75% of my fellow residents had started antidepressants since their intern year,” says Dr. Jill Fadal.
Seems the epidemic of depressed doctors begins in medical school. I wondered how best to verify this oft-repeated 75% statistic. Just then a student called to tell me what her professor said during orientation: “Look around the room. By the end of your first year, two-thirds of your class will be on antidepressants.”
I’m appalled. Yet she’s grateful. Why? Her school is so progressive. They normalize the need for antidepressants.
I must be out of touch. Do most med students require psych drugs for day-to-day survival? I turned my question over to Facebook: “75% of med students and residents are taking either stimulants or antidepressants or both. True or false?”
“It’s absolutely, horrifyingly, true. It is a symptom of a great sickness in MedEd.”
“Sadly I am guessing true as I prescribed some for my residents every year that I worked in a residency.”
“True, but I’m sure a lot is unprescribed.”
“I would assume definitely true, Ritalin, Adderall, energy drinks, ephedrine. Yep.”
“While working as a nurse at a major Army hospital, I was astounded by the number of medical students on Adderall or Ritalin.”
I’ve been on an antidepressant since being premed—18 years now. Little did I know it would be impossible to wean myself off and that my entire class was using Adderall.”
“True but most take them in secret as there are negative consequences and stigma that come with getting your mental health addressed.”
“Very true. From my practical point of view, I’d put medical students & residents at 100%.”
“I take both Zoloft and Adderall daily.”
“Very much so true—the percentages may actually be higher. I see it in my classes and I’m only a premed student.”
“If coffee counts as a stimulant it’s definitely 100%.”
“The only way I’d say false is to say it’s higher. I’d say a quarter of my class had to take a leave for a mental health break.”
Having received Facebook confirmation that most med students are on psych drugs, I then queried 1800 medical students via email with the same question and encouraged respondents to share personal experiences. To prevent professional retaliation, all quotes are published anonymously (with permission).
“I am one of the many who are currently on BOTH antidepressants (2 types) & a stimulant (amphetamine). I lost my very dear friend (also a classmate) to suicide in my third year of med school. I have been on psych treatment since then.”
“Hi Dr. Wible. The number sounds high, but whether it is right or wrong is anybody’s guess. I can tell you about myself and my girlfriend—we both just started our third year at a DO medical school. I use 100 mg Sertraline to treat panic/anxiety attacks that were very bad when we had practical exams. I am also very depressed, but the Sertraline does nothing for this. I was diagnosed with ADD in 2013, right before taking the MCAT. I have been on and off of amphetamines and Concerta since then. Then there’s the alcohol and marijuana for the end of the day when I just get too tired of thinking. I have been offered various benzos by my family doctor to help treat the anxiety attacks. I haven’t filled that prescription, but do use them (from a friend) occasionally to help sleep, escape life etc. This is coming from someone who never touched alcohol or other drugs/mind-altering substances until I was 25-ish right at the time of taking the MCAT. My now significant other also uses Sertraline, Adderall, and Benzos to treat anxiety/panic attacks and ADD. Coincidence? I doubt it. So my sample size is two, but 100% are taking antidepressants and stimulants.”
“True. I’m on them, and every student I know is on them too. I’m on both; never took them before med school. Same with all of my friends. Eek!”
“I do recall around board study season hearing from half of my classmates about sharing Adderall and getting Rx from doctors they knew. I was even offered it, but never tried. However, my coffee intake has definitely gone up since school to the point having trouble controlling my bladder. I also know of about half of my friends taking antidepressants throughout school. So I would guess at least 50-75% of my class took stimulants and/or antidepressants.”
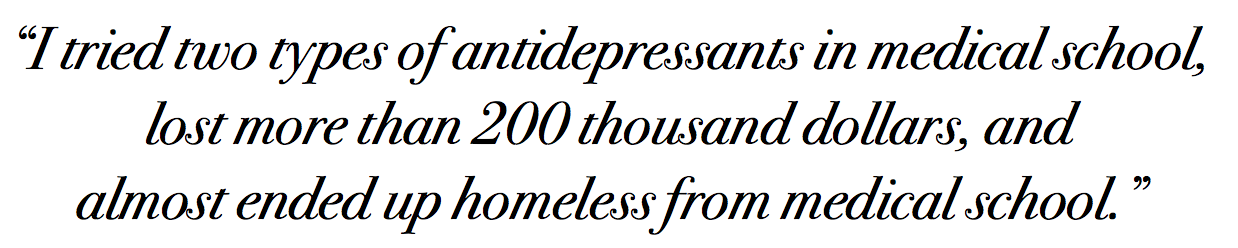
“I tried two types of antidepressants in medical school, lost more than 200 thousand dollars, and almost ended up homeless from medical school. All [my depression and debt] started in medical school. Yet my passion remains.”
“Hi Pamela, I agree! Students are afraid to speak about it and I know some who have even asked friends/family to get meds under their name so it isn’t on their record. I finally started talking about it with my classmates and found that many of my close friends were taking them and we had individually struggled alone not knowing there were others going through the same thing. Also, if everyone’s doing it and it gives you an edge, then everyone else has to do it.”
“Sounds about right. I never needed antidepressants before medical school. And it definitely made me rely on higher doses of methylphenidate than I’ve needed in the past.”
“I never thought I would take study drugs. But I was near the bottom of the class in my exam results, and then found out that several who were best in our year were taking study drugs. I cut my losses and copied them. Low and behold, my results improved drastically. I don’t like it, but for me it is better than falling behind and doing poorly. All my friends at other med schools use Modafinil and Adderall too. They also use recreational drugs like ecstasy, cocaine and acid when they’re partying. Drug use is very common amongst the med students I know.”
“In my med school class, I’ve heard of people on antidepressants, on sleeping pills, using pot to calm down, and then also on some kind of uppers for test days and days after partying which the partying was to de-stress..but I have no idea if it’s 75%…I don’t know enough of my class well enough to have that info, nor do I think anyone does…there are usually cliques of up to 25 people, but for people to say they know for sure details of 75% of their class would be hard for me to believe but maybe…there is a lot of it, I agree with that.”
“True. As a med student I was on antidepressants. No different now I am intern. Having just finished 12 days straight and >120 hrs. I can understand why people are also using stimulants.”
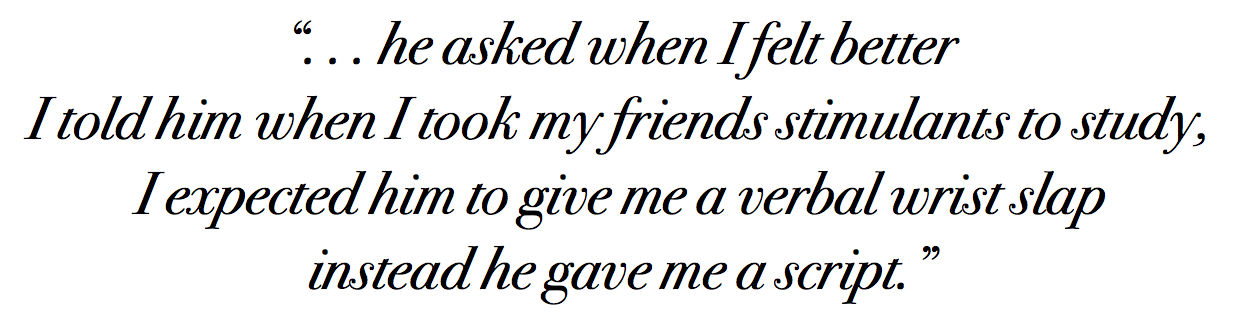
“True. I only have four friends in medical school that I know well enough to know which meds they take. All are on both. I went to the university psychiatrist in my Texas premed program for depression he asked when I felt better I told him when I took my friends stimulants to study, I expected him to give me a verbal wrist slap instead he gave me a script. I was on a steady dose for years but the first year of med school I kept upping the dose to try and keep up, ended up deciding I needed to stop after one episode of not sleeping for four days and having auditory hallucinations. Failed second year when I quit them cold turkey, didn’t feel like I was keeping up without them so switched to Modafinil which is much mellower than amphetamine but definitely not good for me. Everyone started antidepressants in school even folks without a history of depression. Being completely honest 75% seems a bit high, but I wouldn’t be that surprised if it were true, in my n=5 study it’s 100%.”
“True. But that number may be higher or lower depending on the school and year in med school. I was on an antidepressant in the last month of last semester because all my other coping skills weren’t enough. I’m on summer break and I haven’t needed any medications to be functional and happy. My depression was entirely induced by the stress and frustrations encountered during medical school.”
“I was on an inpatient internal medicine rotation working 12-14 hour days 6 days a week (as a 3rd year med student) and would ‘keep it together’ at the hospital and fall apart on the way home, cry and sleep to cope. It was the first time in my life I felt suicidal, no plans—just wanted to fade away. My husband was afraid to leave me alone. I put myself back on the Lexapro, equalized somewhat and kept pushing on. That all happened around Christmas of last year. In June I finally was able to find a psychiatrist. He put me on a trial of Adderall. I was hesitant due to the abuse potential but decided to give it a try. With the two meds I have less anxiety, way better at prioritizing, and my focus is improved. I’m studying for step 2 currently so time will tell.”
“I take Effexor 150mg QD. In addition to 10mg of amphetamine salts TID. I used to drink 2 quad shot white chocolate mochas from Starbucks a day, but with the stimulant I threw myself into SVT too frequently.”
“I cannot talk about anything beyond what I know of my immediate friend circle but I have in mind about 10 examples of people who started NEW prescriptions for 1) Stimulants for studying and staying awake 2) Antidepressants and/or mood stabilizers and one person who was started on 3) Beta blockers for new onset panic. These are people with new diagnoses since starting school. I know a few others who came in on these medications after having hard times as premeds (or earlier, I don’t know) That’s just those who actually got the prescription…. As I’m sure you know there is unfortunately also a great deal of illegal procurement of prescription medications as well as abuse of illegal drugs. An increase in alcohol abuse is also a major concern. People are self-medicating left and right.”
“Oh, I would not be surprised! I know 10 people from 5 different schools and at least 7 are on either.”
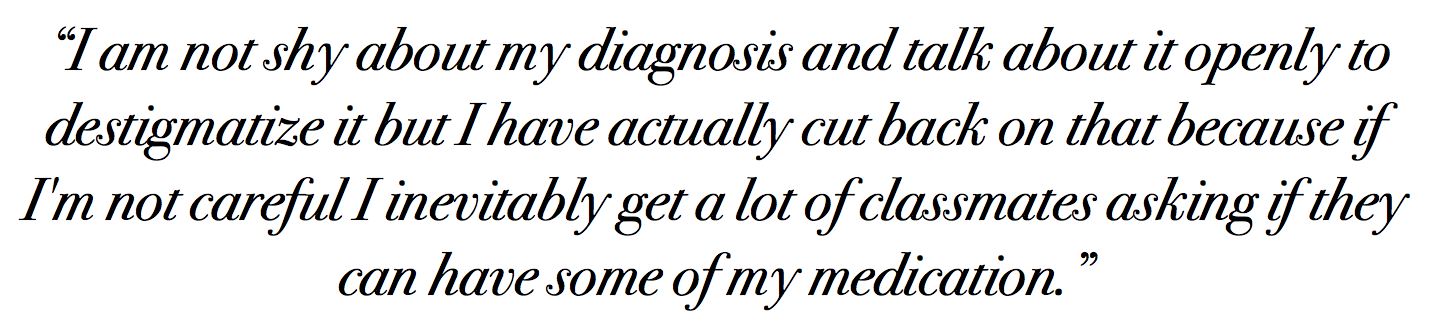
“I am lucky to have a great support structure and have coped quite well so far without needing any medication. I am actually diagnosed with ADHD and have a prescription for two medications which I don’t really use. The pressure to use them every day rather than relying on my own hard-won compensatory skills is certainly there. Interestingly, I am not shy about my diagnosis and talk about it openly to destigmatize it but I have actually cut back on that because if I’m not careful I inevitably get a lot of classmates asking if they can have some of my medication. For a future doctor to brazenly ask for illegal sharing of medicine is worrisome to me but again I do understand the pressure (to stay up just one more hour studying) that drives the behavior.”
“Popping prescription bottle caps and chafing of pills while studying in the library is a fixture of how daunting the pressures of medical school really are. Med school libraries are dungeons where souls came to die. You’re surrounded by absolute dread—the look of despair painted across the faces of your fellow classmates who feel at any second their life could be ruined with one failing grade. Most of my friends were on SSRI’s, Benzodiazepines, and various types of stimulants. I once asked a friend if he had anything to help me go to sleep and he recommended Lorazepam, which he gave me. The ‘top student’ in our class was rumored to be a serial user of cocaine. To avoid having a drug test reveal his dirty little secret prior to third year, he took a hiatus by engineering a family emergency to give himself adequate time to pass the contents of amphetamine (he passed). Elicit substances in medical school may seem like taboo to lay persons, however in our eyes, it’s a natural and regular experience. In fact, it is astounding how many medical students (myself included) smoke marijuana in order to experience a night of restful sleep. With each puff, it’s as if I escape a bit from my hectic reality. A reality dominated by judging, vengeful, and heartless administrators/faculty who can care less if we live or die, as long as we perform on USMLE Step 1. Yup, its that bad.”
In 1990, even I was severely depressed as a first-year med student. So my mom (a psychiatrist) mailed me a bottle of Trazodone. I thought I was the only one crying myself to sleep. Turns out occupationally-induced depression is rampant in medical training. Now schools dole out antidepressants like candy. Stimulants are used by med students like steroids in athletes. So where do we go from here? Should “progressive” med schools distribute samples of Zoloft and Adderall during orientation?
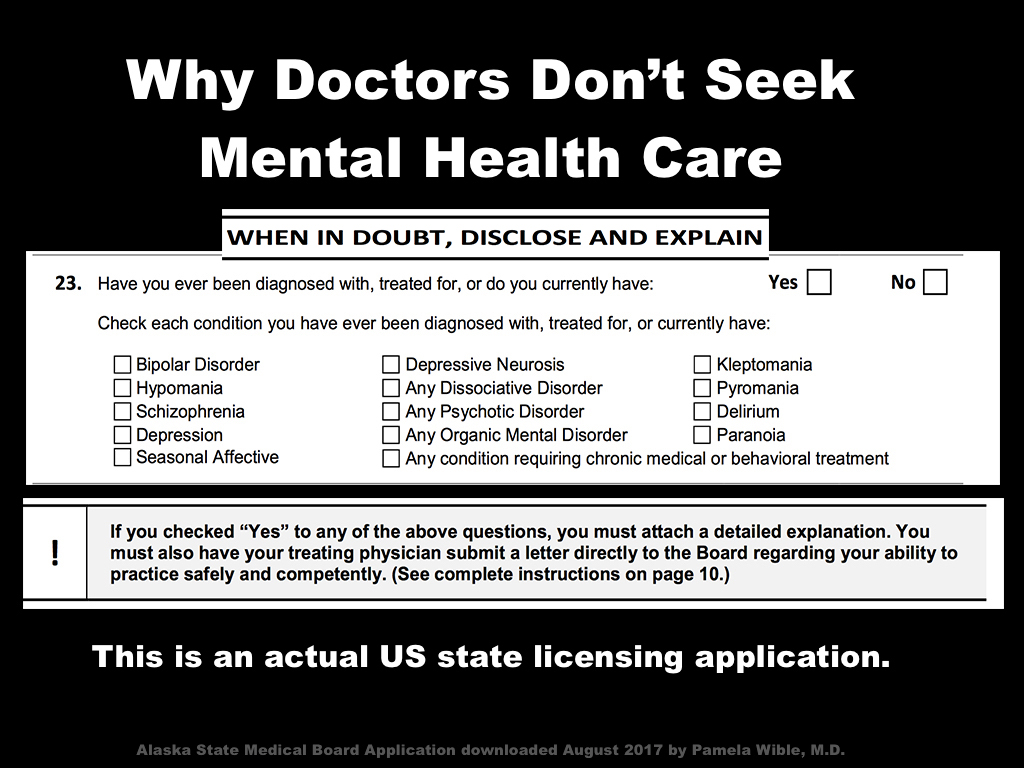
Problem is physicians must answer mental health questions (right next to questions on felonies and DUIs) to secure a medical license, hospital privileges, and participate with insurance plans. Check the YES box and be forced to disclose your “confidential” medical history and defend yourself—again and again for your entire career. Treated like a criminal for taking meds to cope with the torment of medical training (and practice).
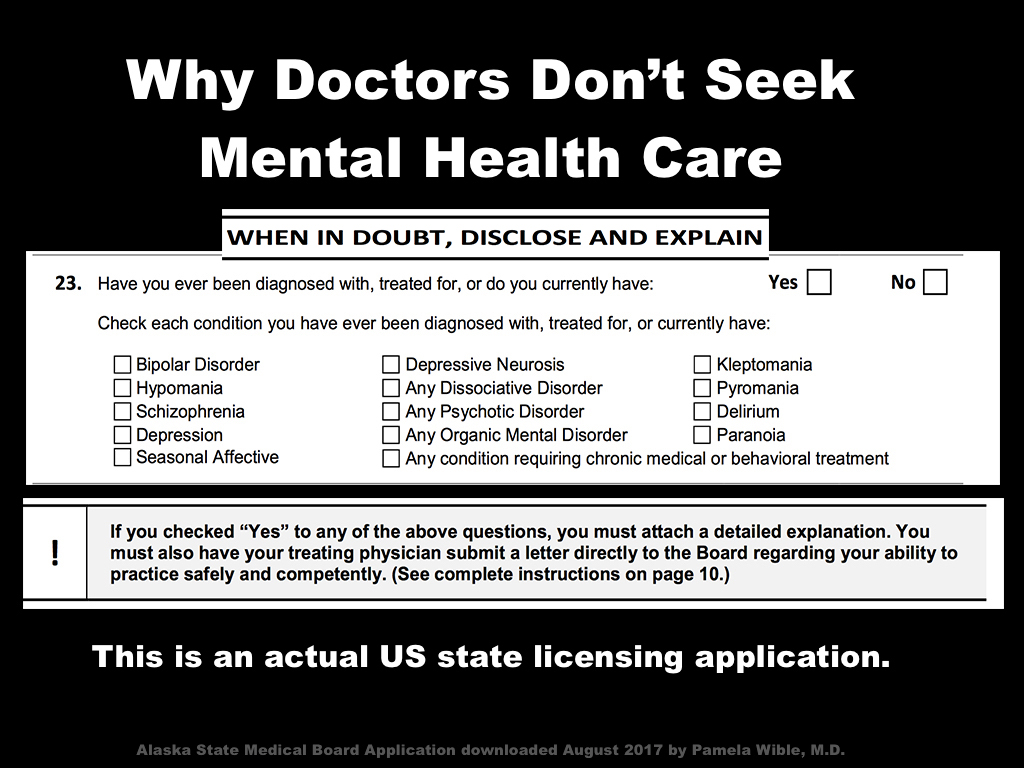
Maybe that’s why so many future (and current) physicians sneak drugs and go off-the-grid for mental health care.
“I’ve been in practice 20 years and have been on antidepressants and anxiolytics for all of that time,” says Jason. “I drive 300 miles to seek care and always pay in cash. I am forced to lie on my state relicensing every year. There is no way in hell I would ever disclose this to the medical board—they are not our friends.”
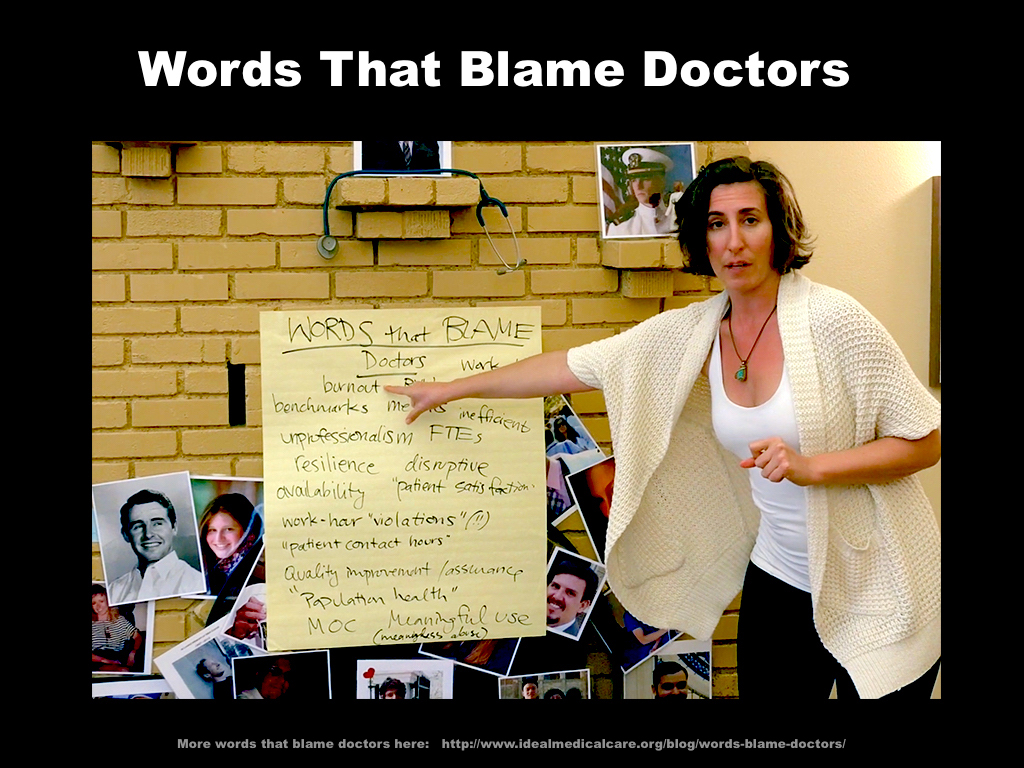
What if we stop the mental health witch hunt on our doctors? Why not replace threats and punishment with safe confidential care? What if we address the root of the problem—the great sickness in medical education—rather than shifting blame to 75% of medical students for not having enough serotonin or dopamine or norepinephrine in their brains?
As scientists, we can’t continue to approach medical education reform as a neurotransmitter deficiency in medical students. Can we?
___
Pamela Wible, M.D., is a family physician in Oregon. She is happy in her solo practice and takes no psychiatric medication. Turns out her depression was environmental—entirely related to the culture of medical education. Dr. Wible is author of Physician Suicide Letters—Answered. View her TEDMED talk Why doctors kill themselves.