Most docs are unaware they waive their HIPAA rights when acquiring a medical license.
The right to practice medicine is a privilege. Each state regulates medical practice by state statute, often called their medical practice act. Most docs have never heard of nor read their state’s medical practice act. Yet when applying for a license, we’re agreeing to comply with statutes we’ve never seen.
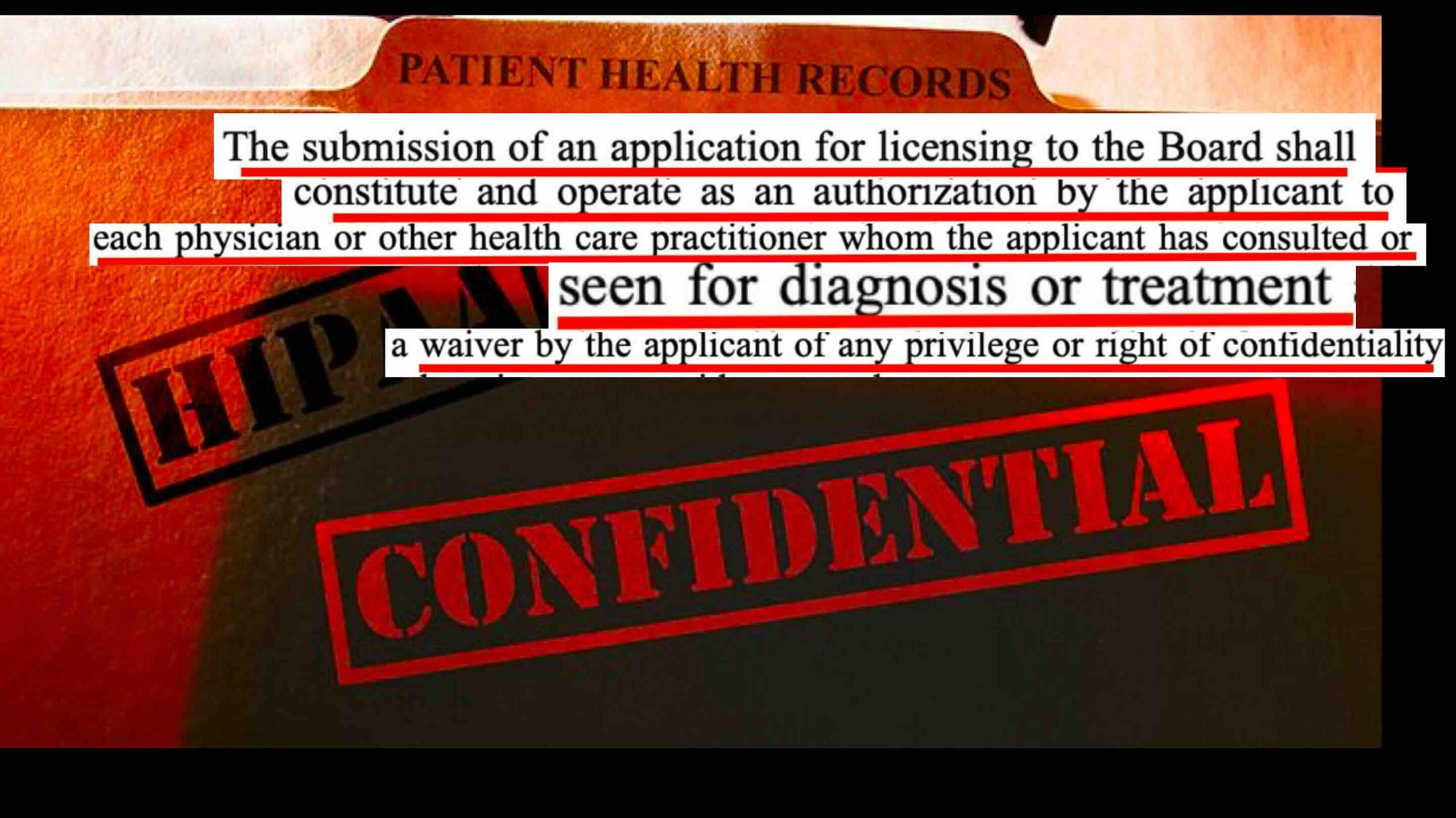
I’d recommend all docs read the contract they’ve signed for the privilege to practice medicine in their state. Here’s fine print from the Mississippi Board:
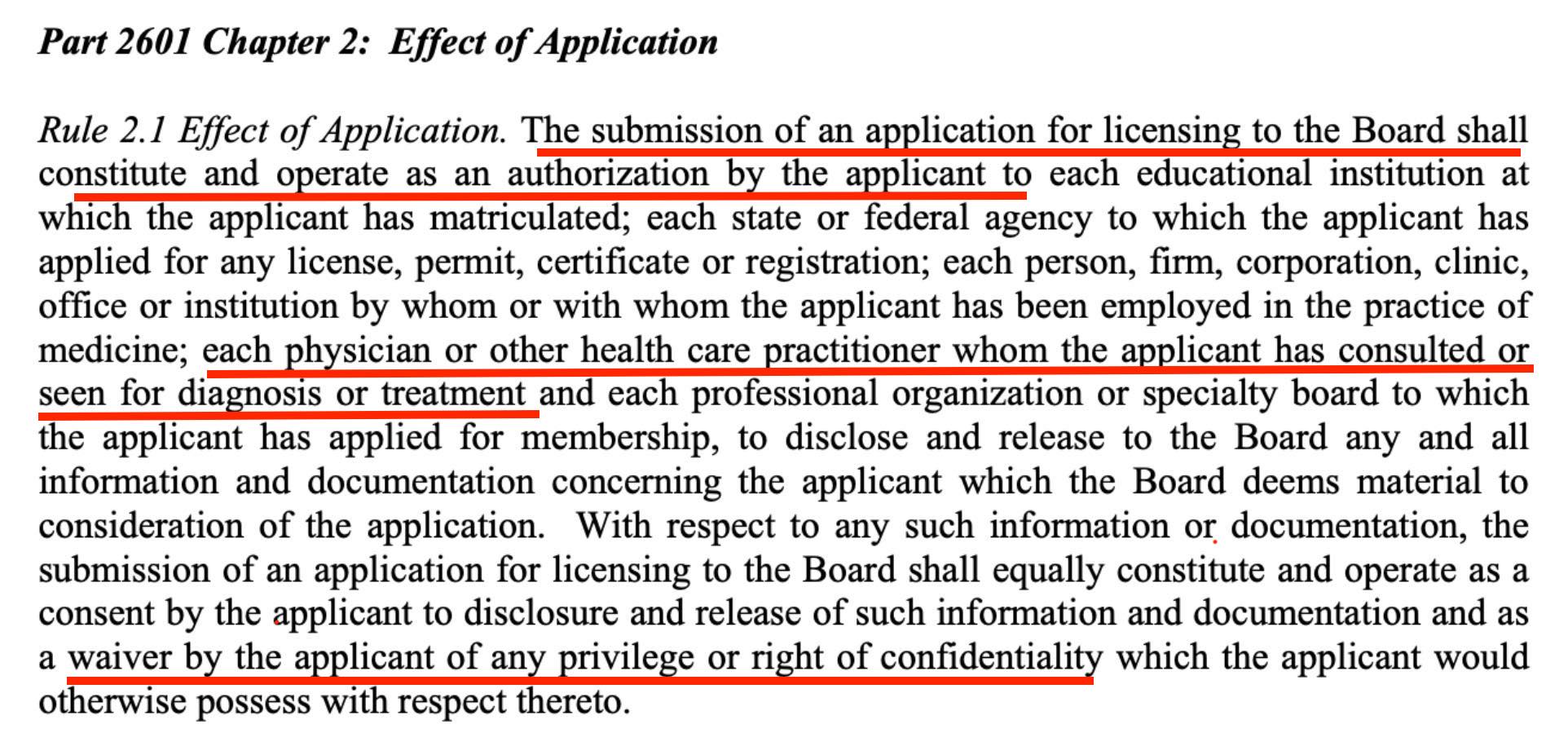
Mississippi Medical Board Application
I bet your state has similar wording hidden in documents you’ve never read.
“The submission of an application to the Board shall constitute and operate as an authorization by the applicant to each physician or health care practitioner whom the applicant has consulted or seen for diagnosis or treatment—as a waiver by the applicant of any privilege or right of confidentiality.”
We entered medicine without informed consent that we’d lack the confidentiality and privacy we uphold for our patients. So what should physicians do when they need help?
Here are 13 tips for doctors who need confidential mental health care.