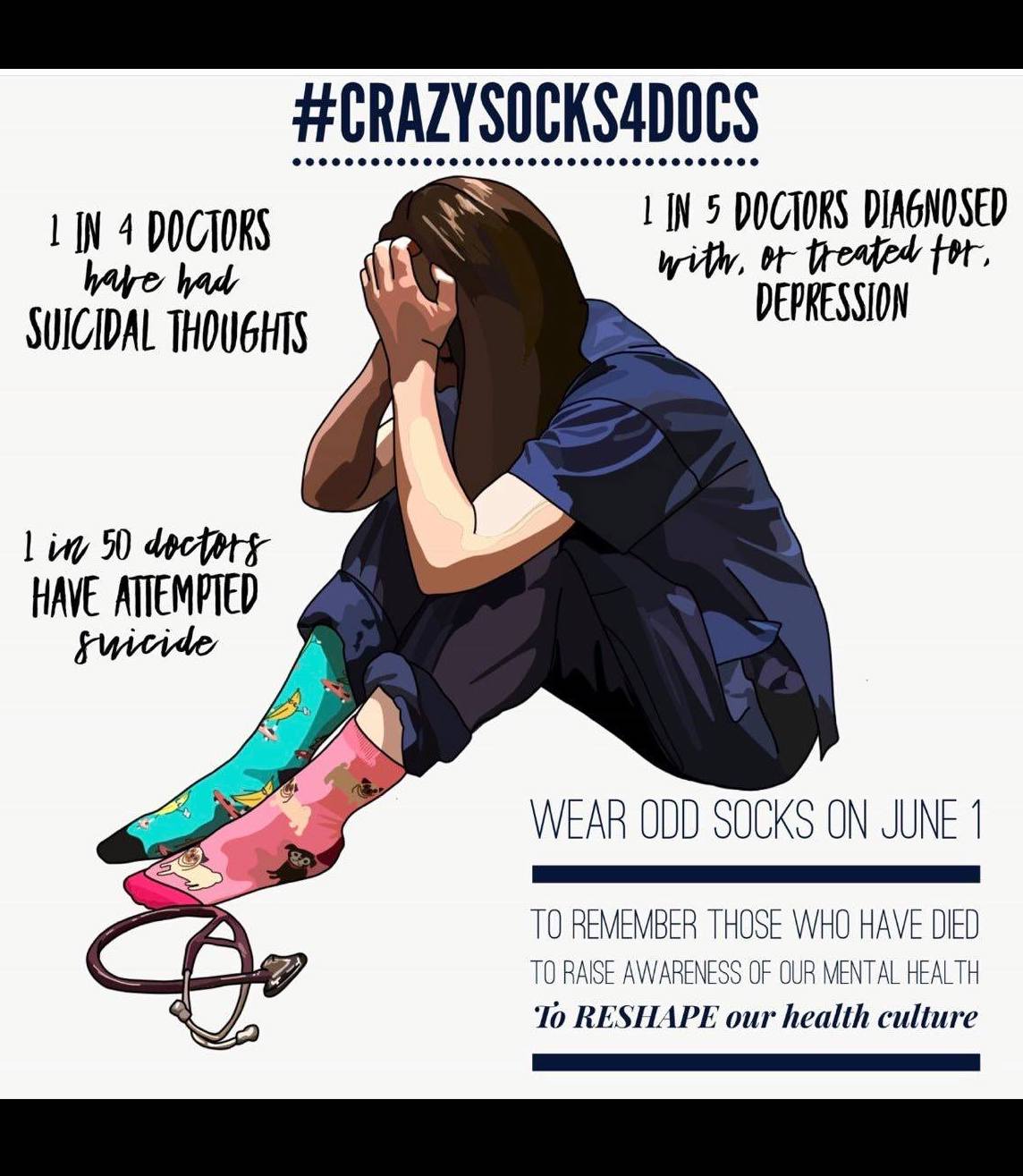
Physicians experience the highest suicide rate of any profession. I’ve been investigating doctor suicides for more than 5 years. What began as a personal quest to discover why so many of my physician friends had died by suicide has now become an international inquiry and full-time job. Here’s what I’ve learned from my first 757 cases. I’ve now amassed 952 doctor suicides on my registry and anesthesiologists remain in the lead with the highest suicide rate among all doctors.
Thankfully two courageous anesthesiologists have stepped forward to address depression and suicide within their hospital. Both were forced out of their jobs. One has filed a lawsuit.
Dr. Michael Shaughnessy—an exemplary anesthesiologist much beloved by staff and students at Duke University—was wrongfully terminated in 2017 as retaliation for his objections to disability and sex discrimination in the Department of Anesthesia.
After the suicide of a second-year female anesthesiology resident (June 2016), Dr. Shaughnessy and others complained about the “insensitive response” and “stubborn refusal” to support those with mental health disabilities and the widespread discrimination against many female anesthesiologists in the department,” according to a federal lawsuit.
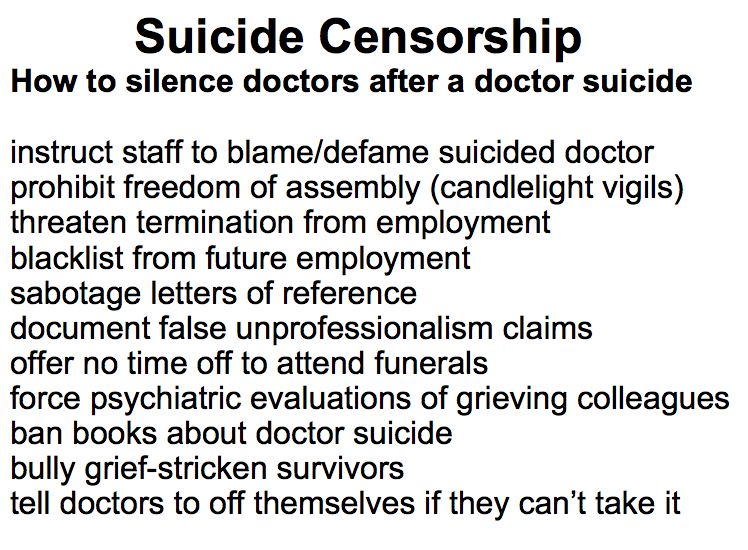
Yet the official stance of the Department Chair was that they held no liability in the Resident’s suicide. Many faculty, visibly upset, felt the focus should instead be helping staff experiencing depression and grief after the sudden death of their colleague.
Faculty member, Dr. Cheryl Jones met with surviving residents to offer her support—at which point faculty were warned they were “not permitted to gather with residents without the approval” of the Program Director. Furthermore, Dr. Jones was prohibited from organizing a candlelight vigil to mourn the Resident who had died.
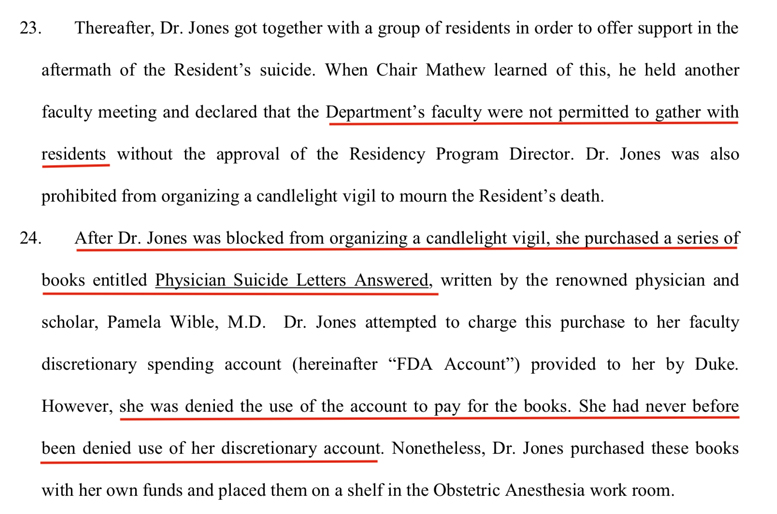
Shaughnessy v. Duke (excerpt page 8 of 24)
“After being blocked from organizing a vigil, Dr. Jones attempted to distribute a book, Physician Suicide Letters Answered, to assist her grieving residents and was physically obstructed by her superiors. The books were stolen from the hospital where she placed them and banned from the department. In August 2016, I received the following email from Dr. Cheryl Jones:
Pamela,
I had previously written you about the death of one of our residents in the anesthesia department. I had mentioned another death [confirmed suicide] of a former internal medicine resident who had just started his fellowship.
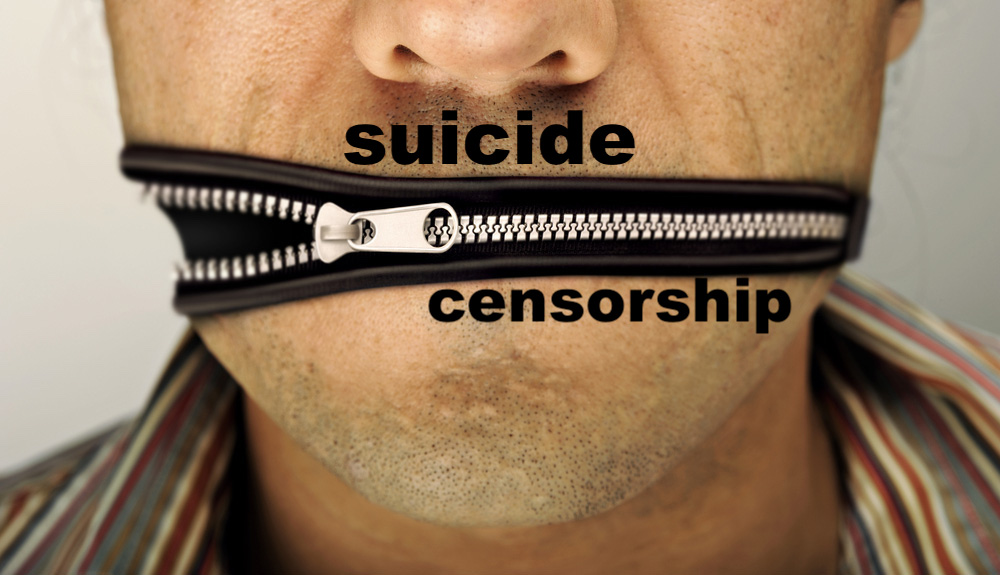
I also want to let you know that our department is doing their best to continue the culture of shaming and secrecy around physician suicide. We are not allowed to talk about what happened. We have not had any sort of service to honor our own grief. We have been given various excuses for the lack thereof.
I had also purchased 6 copies of your book for my residents. I had not distributed them but had told a few about their presence. Please see the department-wide email that I sent last week. The departmental administration should be ashamed of themselves. Please share this information as you see fit.
Sincerely,
Dr. Cheryl Jones
Download Free Audiobook Physician Suicide Letters—Answered
Subject: Book on Physician Suicide
To all,
I have purchased a few books about physician suicide by Pamela Wible, M.D. I have had them for the better part of a month and have not sent a notice that I had them available for anyone. I was refused reimbursement from the department as this was considered to be a personal expense (for 6 books). I had previously purchased books on wellness and had been able to cover them through the department.
On Monday I was summoned to the office of the division chief. I had assumed that I was to be informed as to why the books were not eligible for funds. Instead I was informed by the executive vice chair that “the department did not want me to distribute these books to the residents.” At that time I also discovered that the division chief had stolen these books from the anesthesia workroom where I had placed them on the shelf. Since I have now recovered them I am making them available for anyone that is interested.
Dr. Cheryl Jones
Physician suicide book banned, stolen from hospital (original 2016 blog)
Dr. Shaughnessy was concerned about the mistreatment of Dr. Jones who resigned from Duke Anesthesia faculty it is believed as a result of harassment and retaliation.
During a subsequent meeting held by the Department Chair to prepare for resident application season, he expressed his “disdain for Dr. Jones and her disability and attributed her actions to mental illness” and told those in attendance to inform applicants that “the Resident had committed suicide because she had a drug problem.” They were not to mention her depression.
Dr. Shaughnessy objected to the mischaracterization of the Resident and mistreatment of Dr. Jones and then shared his own “struggle with depression.” Weeks later the Vice Chair warned him not to “rile up the troops” and told him he “could count on sabotaged letters of reference” and “blacklisting” from further employment upon nonrenewal of his contract. He was then terminated for “less than optimum professionalism” and “not being team-oriented.”
In United States District Court, Michael Shaughnessy vs. Duke now alleges discrimination (and retaliation) under the ADA, hostile work environment based on disability, retaliation in violation of Title VII of the Civil Rights Act of 1964 and wrongful termination in violation of North Carolina Public Policy—all actions taken with malice or reckless indifference to Dr. Shaughnessy’s rights. Read 24-page court document.
Yet harassment at Duke is not limited to the Department of Anesthesia as confirmed in a letter (published with permission) from a physician friend:
“A pediatrics resident at Duke took his life several months before graduating from residency. It was a horrible tragedy that had a profound impact on the psyche of all of us residents. Unfortunately, as residents we were completely silenced and the whole tragedy was swept under the rug. I was speaking with 2 other resident colleagues after the incident and said “something isn’t right here.” Within 30 minutes I was called into my program director’s office. There were 4 doctor administrators sitting behind a desk with legal pads and pens. They demanded that I sit down and share anything on my mind and furiously scribbled notes as I spoke. Tears streamed down my face and their cold stares persisted as they took notes. I can barely remember what happened because I was so scared and their intimidation and bullying tactics paralyzed me. The end result: I was immediately forced to go to psychiatric services to be “cleared” so I could report back to clinic that same day and finish seeing patients. I thought I moved on but these visions still haunt me, years later. Some memories can never be erased and linger on in your soul.”
Yet harassment is not limited to Duke; it is widespread throughout medical education in our nation’s most prestigious teaching hospitals as indicated by just a few of the letters in the book that the Department of Anesthesia didn’t want their residents to read:
Hello Dr. Wible, I’m a surgery resident in New York. I began my residency in California and during that time was very depressed due to abuse within my training program. My depression impacted my performance and I was eventually fired. I was lucky enough to find another position and continue my training. However, some days I feel my depression and despair returning—primarily when I feel my career has been irreparably damaged by my departure from my first residency program. Those feelings were initially tied to hazing and bullying that are an integral part of the educational program there. . . I am reaching out to you for two reasons: I’m interested in eradicating the abuse in medical education. I’d like to have a career in academics and to influence policy regarding the treatment of trainees. More importantly, can you help me make the flashbacks stop? Can you help me not worry so much about my future? Can you help me with my depression related to my change in career trajectory? Thank you for your work! ~ Lisa
Pamela, When I share what happens in our academic medical center with my non-medical friends, they are astonished and disbelieving. The level of bullying in my institution is amazing, including a faculty member seriously suggesting that a resident’s mistake was so heinous that he should “off ” himself. ~ Vicky
Dr. Wible, I was dismissed from medical school in the beginning of my fourth year because I had a medical condition that didn’t help the school’s “technical standards.” I suffered abuse my entire third year from residents and physicians telling me that I wasn’t fit to be in medicine, that if I knew what was good for me I would just drop out. My school told me that being sick was akin to being unprofessional, and that I should give up my dreams of wanting to become a physician. They pulled me into their administrative office several times to harass me, and eventually told me that I was dismissed. I couldn’t think, I couldn’t breathe. If I hadn’t called my parents immediately and spoken to them, I don’t know what I would have done because only the worst was running through my head at that time. Medical schools need to be more attuned to their students’ needs and psyches before treating them like slaves or robots with no regard for human emotion. ~ Sarah
Pamela, In anesthesiology, it seems we have a higher percentage of death by suicide than other medical specialties. My colleague took his own life over a year ago. I was basically okay until then, but it’s how everyone reacted that really got me. The show must go on. We diverted patients the first night, probably because the ER had to see Joe when he came in. The next day all of us were back at work in the operating room. There was no time to grieve and we in the department were so stunned we did not know what we needed and what to ask for. It felt like abuse to not honor him or his colleagues with some rescheduling of operations. I will never be the same. I no longer see medicine as a force for good. It seems like it is a way for other people to make money off our talent, intelligence, education, or determination. He was my friend! ~ Bruce
Pamela, I lost another colleague and friend to suicide two weeks ago. As he was an anesthesiologist and I am an obstetrician, I saw him every day and had no clue that he was in such a state of despair. How can we recognize others in trouble? ~ Elizabeth
Dear Pamela, I suspect that you would be hard-pressed to find one of us who isn’t at least sometimes suicidal. We’re just not allowed to admit it as it would end our careers. ~ James
 Sometimes I’m accused of harping on the problem of physician suicide without offering real actionable solutions.
Sometimes I’m accused of harping on the problem of physician suicide without offering real actionable solutions.
I’ve extensively outlined primary, secondary, and tertiary prevention strategies that could be implemented for no or low-cost way back in 2014. In fact, I presented these simple solutions in Washington DC at the American Academy of Family Physicians Convention and published my recommendations in an article that became the #1 most-read and commented piece in the history of Medscape—Physician Suicide 101: Secrets, Lies & Solutions.
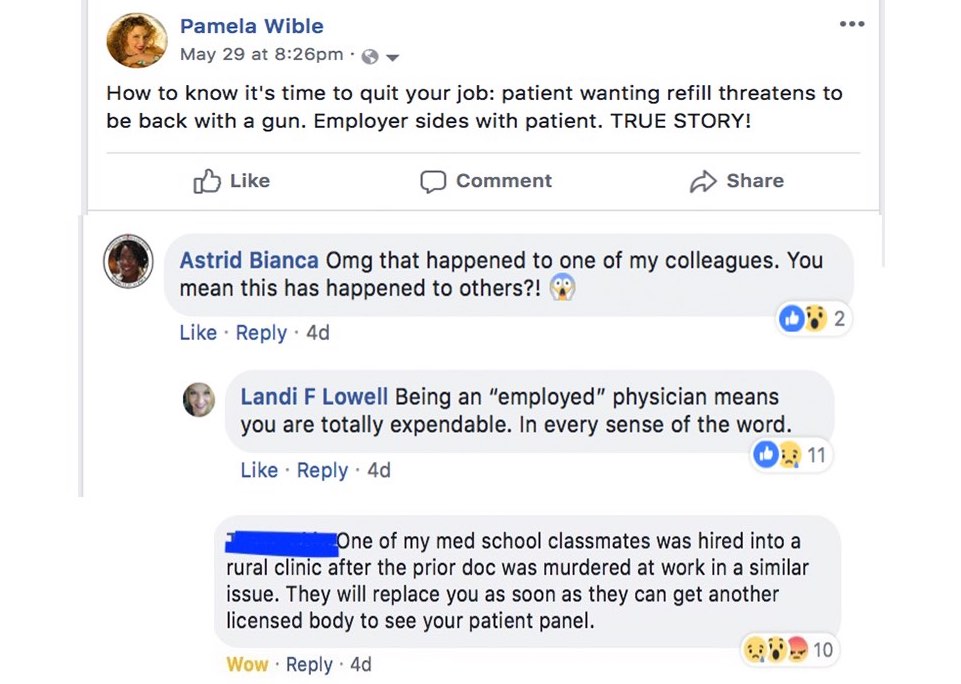
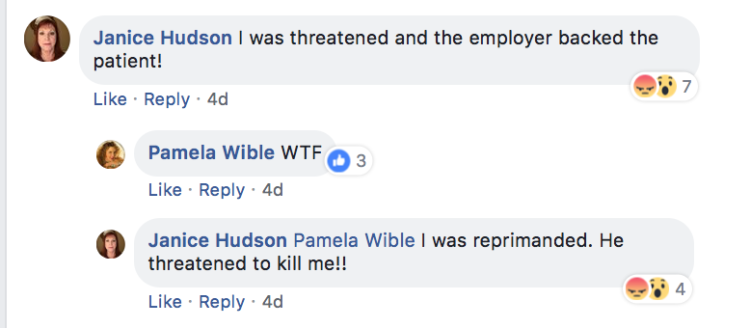
Four years later, I’m not asking for any special rights. What I’m suggesting is that doctors are afforded the same protections by the ADA, OSHA, HIPPA, and labor laws that all other Americans enjoy—including their First Amendment constitutional rights to free speech and to peaceably assemble to mourn the death of a colleague with a candlelight vigil.
Just extend those basic laws to include doctors. Then punish institutions that violate the human rights of their physicians.
If you or your colleagues have been the victims of human rights abuses in medicine, now would be a great time to file a class action lawsuit. Contact me if you need a good attorney. I’ve already got one lined up for you.
View movie trailer forthcoming documentary exposing the physician suicide crisis