I often say I was “born to be a healer.” Now I know why I attract so many wounded people.
I was nine when my family disintegrated. After she lost custody in the divorce, Mom kidnapped me. “Get in the car,” she said as I walked home from school in fourth grade. I didn’t see Dad again until high school. No surprise I chose to be a family physician—since I feel compelled to be in charge of helping to heal families.
My parents are physicians. (So I had to master physician psychology to survive my childhood.) Dad’s an obsessive compulsive pathologist. Mom’s been a suicidal psychiatrist. I’ve been suicidal too. No surprise I run a free doctor suicide helpline—since I’ve been helping suicidal doctors since I was born.
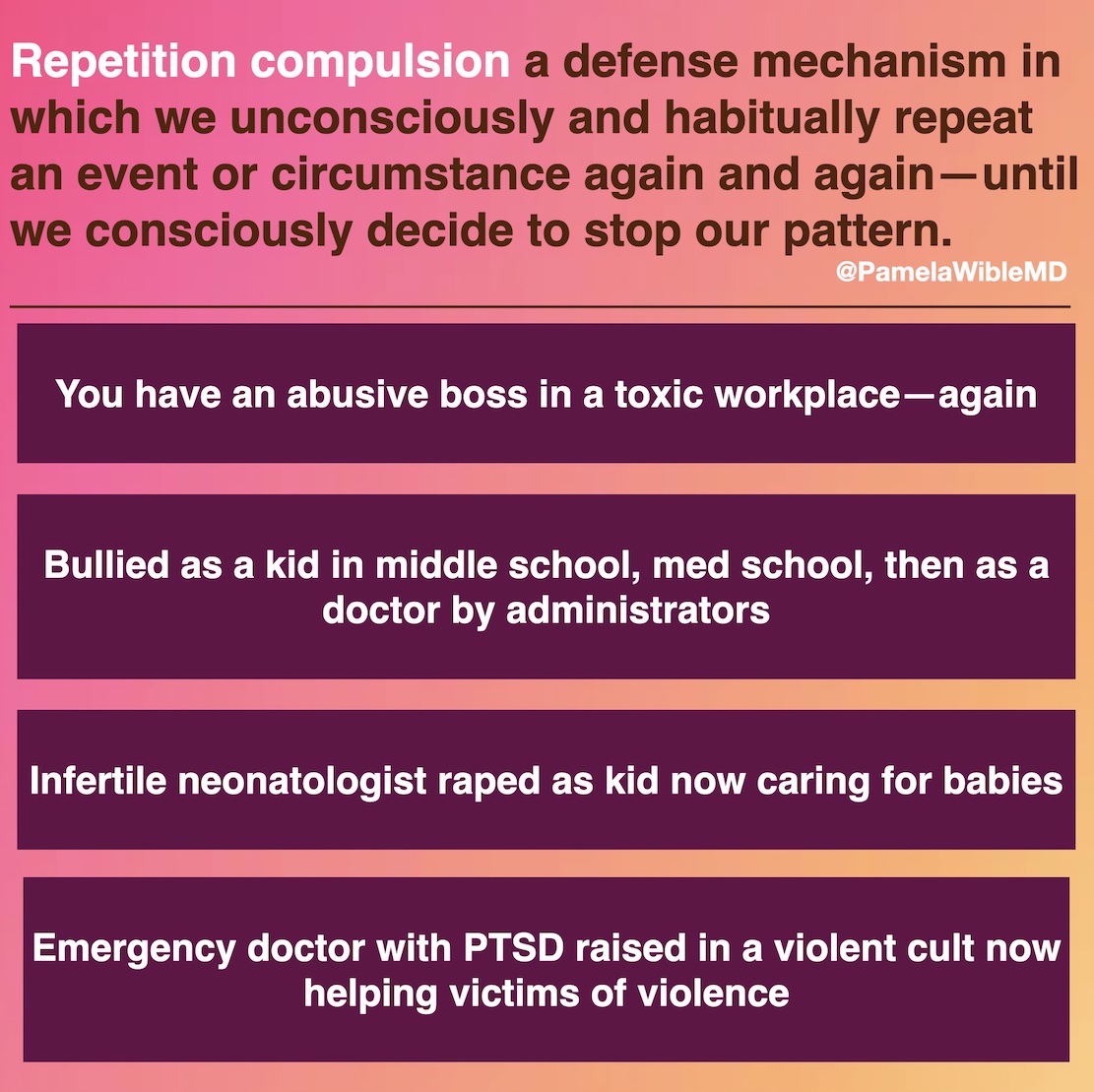
Repetition compulsion is a psychological phenomenon in which a person habitually repeats an event or circumstance over and over again. Like ending up with an abusive boss in a toxic workplace again and again. Bullied as a kid in elementary school, then bullied in medical school, then bullied as a doctor by administrators. We set ourselves up unconsciously repeat our most painful experiences—until we consciously decide to stop the pattern.
Repetition compulsion is a defense mechanism—a psychological strategy that we unconsciously use to protect ourselves from anxiety arising from unacceptable thoughts or feelings.
At a doctor “suicide retreat” I led last weekend, we confidentially shared our suicide attempts and depression with each other. Some of us realized for the first time that our childhood trauma dictated our career decisions. One physician shares (with permission): “I survived sexual abuse as a child, so to protect children I’m a pediatrician.” Others have shared: “I survived losing my brother to childhood leukemia so to help save kids from cancer, I’m a pediatric oncologist” and “I survived two suicide attempts as a teen, so to help teens I’m a child and adolescent psychiatrist.”
Helping others is noble and kind. Yet as a child I was ill-equipped to solve the emotional problems of my physician parents. So I’ve spent my life attempting to solve emotional problems of friends, lovers, and patients—often with great success. Now, of course, given my lifetime of expertise, I’m paid to do this professionally as a physician. Many physicians were caretakers as children who feel compelled to continue caretaking as adults.
Here’s the problem: Helping others without first understanding (and receiving help for) our own emotional wounds, we risk reliving our trauma. Like the emergency physician with PTSD who was raised in a violent cult now trying to help victims of violence. Like the infertile neonatologist raped as a child now caring for babies.
Workaholism is a physician coping strategy for trauma. If we distract ourselves with patients, we avoid our own pain. Eventually memories resurface, often triggered by our patients. Doctors then call me with panic attacks at work and insomnia and rumination at home—with no idea why they can’t function.
Last night an internist wrote me. Subject line: “Here we go again . . .”
“I’m not sure I can do this anymore. I’ve moved from multiple jobs and moved my family countless times. I’ve given my all to my patients and medicine. I was the second highest productive doctor out of ten and everything was going amazingly well. I was told that I was a great fit. After a year in my job I was completely blindsided with a contract non-renewal. I never had any problems with anyone; never killed anyone and always did what’s best for my patients. My family doesn’t want to move again. I’m completely dumbfounded and wondering what to do. I’ve seen counselors and psychiatrists and they have told me I’m fine but I’m completely at a loss. I’m ready to throw in the towel and not be a burden to my husband and kids. I’m grateful for what you’ve done. We’ve talked before. I have no words. All I wanted was to help people and can’t even help myself. I have no idea what’s left. I’m literally at the end of my rope.”
I get it. After six jobs in ten years, I was suicidal. I moved multiple times. I gave my all to my patients and medicine. I was the second highest productive doctor at one of those jobs. After a year in my last job I was completely blindsided with a contract non-renewal. Aha! My pattern: I realized I was a perpetual victim in a healthcare system that profits from dependency and victimology. As a disempowered doctor, I kept attracting disempowered patients who were overly dependent and sucked me dry. Over and over again. I hated my job. My patients hated their jobs. They kept begging me to complete disability paperwork. One wanted a workers comp claim filed for a paper cut that I couldn’t even find. Not kidding! I said: “Do you know how many people will get paper cuts dealing with the paperwork for your paper cut?” and I cut her off. When I launched my own ideal clinic, I stopped being a victim. Only then did I stop attracting patients who were victims.
So why do we compulsively repeat our most painful events? In our quest to gain a belated mastery over our own trauma, we yearn to relive it so we can finally create what we’ve always yearned for—a happy ending.
If you’re suffering, start journaling. Discover your own patterns. Need help? Reach out.