Can depressed doctors get emotional support without risking their license? Is confidential mental health care even possible?
I just got this email from a physician:
“Hi Pamela, Wondering if I could curbside you on the topic of seeking mental health services as a physician. I am not suicidal or impaired, but considering consultation with a psychiatrist for medication. Any chance you would be able to chat with me for a short bit to discuss tips for seeking consultation while avoiding stigma and labeling?”
Sadly, most medical professionals fear seeking mental health help due to stigma and labeling that can follow a physician for a lifetime.
I run a suicide helpline for physicians. So I’ve got a unique vantage point. I’ve spoken to thousands of medical students and doctors with anxiety, depression, and suicidal thoughts.
In fact, doctors seeking help may suffer lack of confidentiality, board punishment, and license repercussions. Punishing physicians for occupationally induced or exacerbated mental health conditions is cruel and all too common in medicine.
I have 13 tips to help depressed doctors get confidential mental health care. So keep reading (& take notes) . . .
Physicians have trouble asking for help. By the time doctors request help, they’re often in dire straits. By punishing the most vulnerable at their greatest moment of need, we increase the already-high suicide rate for doctors.
Even worse, when medical boards are involved, our private pain may be viewed publicly—in perpetuity—as one doctor shares:
“Do you know what really hurts? The fact that anyone can look me up on the Internet and read my dirty laundry. I’m publicly shamed [by my medical board], punished for being ill. I will only know peace when I am gone.”
So how can we prevent doctor suicides if we punish doctors who need help? How can medical professionals be assured their private suffering is not shared publicly?
My best advice comes from more than a decade of hearing worst-case-scenarios from med students and physicians who have faced persecution when seeking help. I’ve gleaned best workarounds and navigation strategies from victims—and their psychiatrists, many now adept at protecting physician patients.
13 proven strategies for confidential physician mental health care
1. Avoid care through your educational institution.
HIPAA’s privacy rule does not apply to “education records” or “treatment records” at educational institutions under the Family Educational Rights and Privacy Act (FERPA). I know trainees sent to school psychiatrists who breach their “perceived” confidentiality by sharing medical charts with deans and program directors. FERPA health records are HIPAA-exempt and courts have ruled students have no private right of action for a FERPA violation.
2. Beware of mandatory Physician Health Program (PHP) referrals.
Forced mental health care by an employer or medical board is never the best way to get confidential psychological support. Many medical institutions fund PHPs—a financial conflict of interest—plus PHPs charge medical professionals high fees not covered by health insurance. Doctors fear PHPs and some are left destitute after seeking help.
3. Bypass Employee Assistance Programs (EAPs).
If you suffer work-related mental health problems, seeking help from an employer-funded counselor presents a conflict of interest and risks a confidentiality breach. A surgical resident shares:
“I struggled with lack of sleep in a program which eventually was put on probation for duty-hour violations, though we were bullied into lying about our hours. Any violations were our fault, not the program’s. I was picked on by a more advanced resident, and the PD sent me to EAP because he thought I was the source of the problems. They sent me to a psychologist who diagnosed me with ADD. He sent me to a psychiatrist, who added bupropion and methylphenidate to my escitalopram. I ended up not having my contract renewed in the end.”
4. Confirm that your sessions are confidential.
Ask if your records and communications will be 100% confidential. Inquire about exceptions to your confidentiality. Health professionals may be mandatory reporters, legally bound by state laws to report abuse. HIPAA allows health professionals to breach your confidentiality if you are a threat to yourself or others.
5. Confirm that your private medical records are stored securely.
Physicians’ personal medical records have been accessed to discredit them and discriminate against them for disability insurance, licensing, hospital privileges, and medical liability cases (even during divorce and custody battles). Publicizing private medical records online is a form of extreme shaming and bullying. To protect physicians, some health professionals use biometric fingerprint safes to store handwritten paper charts with fake names. Psychiatrists may hospitalize docs under fake names and place VIPs (like high-profile athletes) in fake charts, never stored with other charts or in EMRs. An emergency doc reveals:
“I was sued. Overwhelmed with grief and fear, I took antidepressants and saw a psychiatrist. I paid cash and considered using a false name. I had already seen the Board send a physician to 6 weeks of inpatient alcohol treatment due to a complaint without any proof he was drinking. That saved his license but he owed an astronomical bill.”
6. Avoid having your mental health documented in an EMR.
From hackers and government agencies to prying eyes of peers, you are forever at risk of a confidentiality breach with electronic records. One physician wrote:
“Psychiatry has been weaponized against physicians . . . with libelous entries placed into the EHR by psychiatry sucking up to admin after a physician reported misconduct [and patient safety issues] at that hospital, the EHR becomes a battleground for a false narrative against YOU. If you complain to the board or any other agency, first thing they do is read your personal EHR, which is now ruined, falsely stating psychiatric diagnoses or substance abuse you don’t have! Reputational harm can be severe, and could cost you lots to defend yourself before a board, including hiring forensic psychiatrists to testify that you’re not nuts.”
7. Don’t use your insurance.
To keep the medical-regulatory complex out of your private matters, it’s best to avoid having psychiatric billing codes attached to you. A mental illness may be used against you by the board, in a malpractice case—even be grounds for denial of disability and life insurance policies. One psychiatrist reports:
“I deal with these issues all too often. Appalling that a patient should be afraid to utilize their expensive personal insurance to pay for mental health or be unable to ‘fully divulge’ the extent of their suffering to allow me to best help.”
8. Go out of town or go virtual.
Doctors in small towns don’t want to sit in a psychiatrist’s waiting room next to their own patients. High-profile physicians don’t want to be locked up on inpatient psych at their own hospital. To get confidential care, many choose telehealth services or travel out of town. A physician friend shares:
“After reading an article about one woman’s journey through hell after being honest on those [medical board] application questions, I sought care an hour away. I drove an hour in another direction to nervously fill prescriptions for antidepressants. I required several meds to stop thinking of suicide all day every day. My suicidal thoughts were 100% work-related.”
9. Consider pharmaceutical confidentiality.
To avoid picking up psych meds at the local pharmacy, doctors may fill scripts out of town. Medical boards and government agencies can access state pharmacy records so some doctors use Canadian mail-order pharmacies to avoid US mental-health persecution. Here’s one workaround a physician shares:
“I used samples of Paxil and had my spouse write me prescriptions for Lexapro, Buspar, Paxil, and sleeping pills over the years. I did not trust other doctors. I did not want any of this stuff in my records as I did not want to be seen as ‘crazy’ (this is how many doctors refer to psychiatric patients).”
10. Be familiar with your state board rules, statutes, and applications.
Most board applications ask mental health questions and threaten license revocation for lying. A physician shares:
“Applications also ask about gaps in education, training, or employment. Essentially they are fishing for more information. Responses like ‘leave of absence to get treatment for a chronic medical condition’ will be met with requests for medical records or other information. So even if you get past these first questions, applications are designed so you’ll have to disclose one way or another.”
Then, in tiny-font print before the signature line you will likely be waiving your HIPAA rights:
“The submission of an application to the Board shall constitute and operate as an authorization by the applicant to each physician or health care practitioner whom the applicant has consulted or seen for diagnosis or treatment—as a waiver by the applicant of any privilege or right of confidentiality.”
Physicians are terrified they may lose their livelihood—even if their job is killing them. One doctor reports:
“I’ve been in practice 20 years and have been on antidepressants and anxiolytics for all of that time. I drive 300 miles to seek care and always pay cash. I am forced to lie on my state relicensing every year. There is no way in hell I would ever disclose this to the medical board—they are not our friends.”
What happens when you declare your mental illness to the medical board?
Two doctors share their experiences:
“I was definitely subjected to discrimination, and it comes up EVERY TIME I apply for a new job, license, or malpractice. All I had was run-of-the-mill outpatient managed depression, and I probably should have chosen to just lie about it like 95% of applicants must, but I didn’t, and almost twenty years later it’s still hanging over my head.”
“By checking the ‘YES’ box: ‘Have/are you treated for depression?’ I was required to sign a five-year consent agreement, with stringent quarterly regimen; each quarter, the following had to be submitted to the state board: evaluation letters from multiple colleagues to affirm my fitness for practice and appropriate interactions with staff and patients, scheduled meetings with an assigned psychiatrist for validation of my fitness for practice, and a meeting with a board subcommittee, all completed prior to that month’s board meeting. All because I did not hide having been depressed and was (am) still taking an antidepressant. I’ve always wondered what would’ve happened if I’d just lied and said I’ve never been depressed.”
Of course, even if you lie, the board has the power to subpoena medical records.
Curious where your state medical board stands on mental health issues? Here’s my only peer-reviewed article that ranks every state—Physician-Friendly States for Mental Health: A Review of Medical Boards
11. Review hospital privilege and insurance applications.
Many hospitals ask similar invasive mental health questions. Check wording on applications for hospital staff, insurance credentialing, disability, and life insurance.
“I’ve seen good friends denied disability and life insurance policies tiered to same as 1-pack-per-day smokers because of history of depression (even well controlled with meds). Coercive and unnecessary referrals to PHPs. Sometimes boards take away the physician’s freedom, dignity, even license. Agencies and some boards don’t differentiate between illness and impairment. They apply policies of ADA and HIPAA differently to physicians in the name of ‘protecting public safety.’ Licensing agencies and corporate medicine can mandate release of information without any sign of impairment. Our physician ER colleague had to fight 10 years for her license due to disclosing feeling the ‘baby blues’ at work. Discrimination SHOULD NOT and DOES NOT only apply to a few listed categories of race, gender. Discrimination due to one’s profession is also a type of discrimination that is not addressed when it comes to physicians’ rights.”
12. Beware of sharing your mental health with colleagues (especially market competitors).
Sadly, physicians are highly competitive and they are encouraged to rat each other out by medical boards and hospitals as this woman explains:
“The only time my physician fiancé got into trouble with the boards of both Texas and Ohio was from a coworker. This other doctor believes that anybody and everybody who is medicated for mental illness is an immediate danger to his patients. So when he overheard my fiancé talking about being on antidepressants (chronic depression since 18 years old due to abuse in his childhood—a fact he always spoke openly about during college, residency, and career) he reported him to the Ohio board. They put him on probation for 5 years even though he never made a major mistake. Then the Texas board heard about it. He didn’t have money or time to run to Texas for the hearings, so he voluntarily gave up his Texas license. That blackballed him with Medicaid and several pharmacies. No wonder doctors are killing themselves.”
13. Consider curated and confidential peer support.
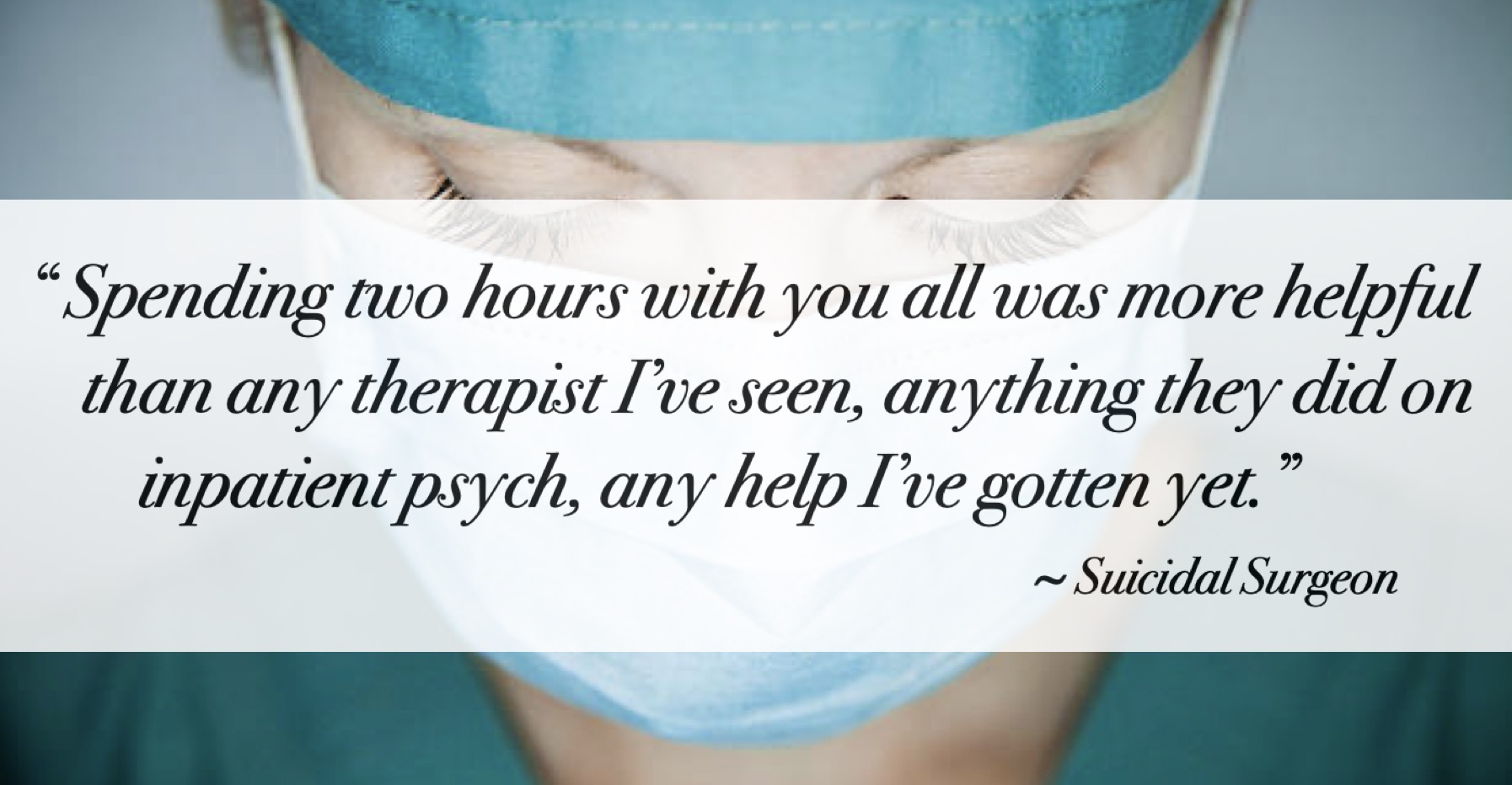
Often the most impactful first-line intervention for depressed doctors is peer support. Not with your coworkers or market competitors, but with an intimate group of up to 10 physicians who meet regularly to heal from suicidal thoughts, childhood or residency abuse, isolation, divorce, business problems, and more. No records. Nothing to subpoena. I’ve been curating physician peer support groups every Sunday for a decade. A suicidal surgeon shared, “Spending two hours with you all was more helpful than any therapist I’ve seen, anything they did on inpatient psych, any help I’ve gotten yet.”
No matter what—ALWAYS seek the care you need.
Despite the physician mental health witch hunt, YOUR LIFE IS PRECIOUS. Always choose your health first—no matter what the career repercussions—as this physician shares:
“Since being hospitalized with severe suicidal depression, I have lost my privileges, malpractice insurance, a current case (malpractice) now wishes to settle instead of defend my care (patient died of blood transfusion reaction not negligence on my part), my specialty society is failing to let me sit for MOC, and these events are all reported to the board so I will face an investigation soon. It breaks my heart that as a society and community of physicians we do not extend the same care and concern that we extend our own patients. I tried so hard to handle my own mood disorder without the help I desperately needed because of the repercussions I knew I would face. Going to the hospital was the very best thing I have ever done for myself. I am facing a total loss of my career and livelihood but I can now handle it and stay alive.”
So back to you—the physician who wrote me tonight for a curbside consult on seeking tips to avoid stigma and labeling when consulting with a psychiatrist for medication.
You wanted to chat with me. I called you twice this evening and got no answer. Then I texted you. Since I couldn’t reach you and I wouldn’t have been able to summarize my best advice in a quick call, I wrote this article just for you.
Bottom line—you are unlikely to be guaranteed 100% confidentiality unless you see a psychiatrist who keeps locked-in-safe paper charts (with a fake name) and claims no idea who you are if subpoenaed by Board. You’ll need to always pay cash, get meds filled at an out-of-state (or out-of-the-country) pharmacy. You’ll need to keep your mental health completely separate from your employer, med board, hospital, insurance plan, and anyone else who you do not trust 100%—and never agree to “mandatory” mental health care with “preferred” providers through your workplace or other medical institutions.
Of course, if you want 100% confidential peer support—join us Sunday. As always, if you need to talk—I’m available. Free. No chart notes. Nothing to subpoena. 😃 Yay! 🎉
Let me know if you have any more questions.
If you are a psychiatrist reading this, do let us know any other stealthy tips you use to keep docs safe.
Without help, here’s what depressed doctors do (when nobody’s looking)














I agree with everything you wrote. Can’t be too careful and it is getting harder and harder to maintain confidentiality. I think, unfortunately, sharing information even in peer support groups can be tricky. People talk more than they should.
I have had patients request paper records and such when they are very concerned. Disability applications are a big problem for people who use insurance, there is no way to withhold the records if you want to apply as you know.
Cash pay with a provider who doesn’t know the doctor or their colleagues and is trustworthy is so important. I don’t trust psychiatrists to maintain confidentiality when suicidality or substance use is an issue, especially the younger, more inexperienced doctors. The McCarthyism mind set is frightening. I would be much more trusting of a PCP to prescribe. Sad to say but true. You know what I mean.
Yikes! I still can’t believe some psychiatrists keep paper charts (with fake names) locked in a safe when they see doctors who (of course) pay cash & get meds filled at out-of-state (or out-of-country) pharmacies! All to keep med boards from mingling with their mental health! OMG.😳 This is the state of health care in America y’all. Explains a lot . . .
That’s how the wealthy elite do it!
Don’t ask me how I know 😉
As I am sure you know, the corporate systems cooperate with this completely.
With hiding the VIPs?
Like during VIP hospitalizations, they totally cover for the “royals” or “Hunter Biden” or whomever . . .??
I wanna know.
This is just fascinating—and so disturbing.
But psychologically just really interesting to me.
And trying to wrap an ideal clinic around these perverse situations is just nuts. Though I do think we have the edge when we do things properly out of the system.
Just curious (regarding the bottom line section) which of those things are you willing to do for clients? Can’t imagine most psychiatrists would be willing to do fake charts. I think only us fringe-worthy folks are willing to go WAY out on a limb. I do like my limb. ❤️
I have done all of them. It is not a common request. The doctors I work with are more guarded than you would imagine. Some laws are more protective over physicians in this way. Like you pointed out. I believe Michigan, Connecticut, Hawaii, ad New York have no mental health questions. I think trainees get more scrutiny in this environment (anecdotal experience).
When a very big VIP goes to a big-name hospital they can get a fake name and DOB. And if anyone outside of the treatment team looks at the chart they pretty much get reprimanded or worse. HIPAA gets enforced. I understand the reasoning because unscrupulous workers can sell information etc…They still use the EHR in the hospitals but in outpatient practice. Honestly I think it varies a lot.
If I trust the patient then the psych chart is purely a medication record and all of the process work is kept in storage in my brain. If I need to document extensively then so it goes.
I think the main conflict is when prescriptions are written. As you stated mail order is a bit easier and avoids any possibility that the local big chain pharmacy has the info on file for some reason (like an old antibiotic rx).
Oh and I don’t do “fake” charts, but spelling errors do occur 🤣
As a therapist, I always ask my physician clients if they want me to avoid giving them a mental health diagnosis. Keeps the medical board at bay. Most docs take me up on this.
Boards need to change their mental health questions to current competency questions. While we don’t want someone practicing medicine that has judgement altering conditions, our society and medical system violates the human rights of health workers—especially doctors—who have no labor law protection regrading work hours and such. Occupationally induced moral injury should not tarnish one’s career.
I see nothing that I disagree with in your article and everything looks true accurate and profoundly important.
and so disturbing!! I mentioned a few of these things to a friend at Farmer’s Market this morning and his eyes glazed over pretty quick and I think he had to look away. And he was the one who asked about this having a friend currently in residency. The level of trauma is beyond what most can comprehend. Just freaky as hell. I guess they never truly give informed consent to those going into psychiatry that they will be concurrently trying to document AND hide their documentation. What total dissonance!
The “You wanted to chat with me” paragraph at the end is powerful and elegant. It really defines your place in the world. I love it.
This article is a scary reminder of dangers of seeking help – and also the power of psychiatric notes.
My fear is less now that I am contemplating life without insurance entanglements. My own practice has ghost records, and any psychiatrist I see as a patient is out of the USA or record-free as well.
Pharmacy records can be a problem, also. I “earned” a mental health exclusion in my disability insurance because the insurance company dug through saw I had been prescribed Zoloft. I think. Even though I hadn’t disclosed visiting the doctor who prescribed it. (I had forgotten his name.)
GHOST CHARTS omg never heard of that . . . Per Google: What is a ghost in charting? Ghost charts, sometimes referred to as shadow charts, are duplicate medical records. Governance documents in several countries suggest that ghost charts present a risk to patient safety, to the extent that they contain information which may not appear in an official hospital record. Although most would agree ghost charts should not exist, their existence is widespread.
SO it appears from above that ghost/shadow charting is unintentional. I surely think intentionally creating a GHOST CHART for a living patient is some serious skeletons in the psychiatric profession closet!
I don’t think I made up the term “ghost record” but I don’t know. It’s been a long time since I considered those aspects of records. I’ve had mandatory EMR throughout my psychiatric career. Maybe it was something a psychiatrist a generation or two before me said.
My grandfather the GP had a drawer full of patient notecards written in Yiddish – seems like a good plan for me except for not knowing Yiddish.
WOW! Psychiatrist just told me this is so brilliant that she wants to put it on her website. PERMISSION GRANTED Anyone who wants to share this you may do so linking back to my website and posting me as author. PLEASE DO SHARE WIDELY.
It is getting worse and worse and more pervasive. Here in California, our Governor just signed into law a bill that potentially prosecutes doctors if they “spread misinformation” which seems to mean saying anything to a patient that does not flow exactly along the dictated protocol .
Read The Psychology of Totalitarianism.
I got denied log-term disability because I was on Prozac. Years ago.
I have had patients and colleagues have psychopharmacological use even if off label: migraines; PMS; sleep; even one that was prescribed but never filled used against them in lots of ways.
Peter YES – excellent point. Lexapro for hot flashes or fibromyalgia or something else.
Med records get busted wide open in dirty custody battles… You wanna destroy your ex? Here- accuse them of being crazy & see if they pick their career or their kid… Hint: they pick their kid – if they are even given the choice
Just amended the article to reflect the divorce/custody battle angle. Even if you are not a physician, these records can be used against you to deny life/disability insurance and disparage your character in any court proceeding (esp divorce/custody cases).
Meanwhile, I just have to point out the irony here: 75% of med students are on antidepressants or stimulants (or both)
“I am one of the many who are currently on BOTH antidepressants (2 types) & a stimulant (amphetamine). I lost my very dear friend (also a classmate) to suicide in my third year of med school. I have been on psych treatment since then.”
“Hi Dr. Wible. The number sounds high, but whether it is right or wrong is anybody’s guess. I can tell you about myself and my girlfriend—we both just started our third year at a DO medical school. I use 100 mg Sertraline to treat panic/anxiety attacks that were very bad when we had practical exams. I am also very depressed, but the Sertraline does nothing for this. I was diagnosed with ADD in 2013, right before taking the MCAT. I have been on and off of amphetamines and Concerta since then. Then there’s the alcohol and marijuana for the end of the day when I just get too tired of thinking. I have been offered various benzos by my family doctor to help treat the anxiety attacks. I haven’t filled that prescription, but do use them (from a friend) occasionally to help sleep, escape life etc. This is coming from someone who never touched alcohol or other drugs/mind-altering substances until I was 25-ish right at the time of taking the MCAT. My now significant other also uses Sertraline, Adderall, and Benzos to treat anxiety/panic attacks and ADD. Coincidence? I doubt it. So my sample size is two, but 100% are taking antidepressants and stimulants.”
“True. I’m on them, and every student I know is on them too. I’m on both; never took them before med school. Same with all of my friends. Eek!”
“I do recall around board study season hearing from half of my classmates about sharing Adderall and getting Rx from doctors they knew. I was even offered it, but never tried. However, my coffee intake has definitely gone up since school to the point having trouble controlling my bladder. I also know of about half of my friends taking antidepressants throughout school. So I would guess at least 50-75% of my class took stimulants and/or antidepressants.”
“I tried two types of antidepressants in medical school, lost more than 200 thousand dollars, and almost ended up homeless from medical school. All [my depression and debt] started in medical school. Yet my passion remains.”
“Hi Pamela, I agree! Students are afraid to speak about it and I know some who have even asked friends/family to get meds under their name so it isn’t on their record. I finally started talking about it with my classmates and found that many of my close friends were taking them and we had individually struggled alone not knowing there were others going through the same thing. Also, if everyone’s doing it and it gives you an edge, then everyone else has to do it.”
“Sounds about right. I never needed antidepressants before medical school. And it definitely made me rely on higher doses of methylphenidate than I’ve needed in the past.”
Read all the quotes here from med students who did not need meds before med school. Now on mutiple Rx—plus caffeine.
“I never thought I would take study drugs. But I was near the bottom of the class in my exam results, and then found out that several who were best in our year were taking study drugs. I cut my losses and copied them. Low and behold, my results improved drastically. I don’t like it, but for me it is better than falling behind and doing poorly. All my friends at other med schools use Modafinil and Adderall too. They also use recreational drugs like ecstasy, cocaine and acid when they’re partying. Drug use is very common amongst the med students I know.”
“In my med school class, I’ve heard of people on antidepressants, on sleeping pills, using pot to calm down, and then also on some kind of uppers for test days and days after partying which the partying was to de-stress..but I have no idea if it’s 75%…I don’t know enough of my class well enough to have that info, nor do I think anyone does…there are usually cliques of up to 25 people, but for people to say they know for sure details of 75% of their class would be hard for me to believe but maybe…there is a lot of it, I agree with that.”
“True. As a med student I was on antidepressants. No different now I am intern. Having just finished 12 days straight and >120 hrs. I can understand why people are also using stimulants.”
“True. I only have four friends in medical school that I know well enough to know which meds they take. All are on both. I went to the university psychiatrist in my Texas premed program for depression he asked when I felt better I told him when I took my friends stimulants to study, I expected him to give me a verbal wrist slap instead he gave me a script. I was on a steady dose for years but the first year of med school I kept upping the dose to try and keep up, ended up deciding I needed to stop after one episode of not sleeping for four days and having auditory hallucinations. Failed second year when I quit them cold turkey, didn’t feel like I was keeping up without them so switched to Modafinil which is much mellower than amphetamine but definitely not good for me. Everyone started antidepressants in school even folks without a history of depression. Being completely honest 75% seems a bit high, but I wouldn’t be that surprised if it were true, in my n=5 study it’s 100%.”
Thanks for the under-the-radar tactics. I am up late contemplating how I am going to get the help I need amid my toxic residency—without drawing attention from my PD or peers.
Happy to help and feel free to join us on Sunday or email me privately here.
I am horrified by the stories posted here.
I am a Family Medicine Dr “contemporary” of Dr Wible and support her advocacy for “mental health” (I prefer the term “thought disorders”) for all but especially those whose professional life triggers such dysfunction.
I am aware that there is an “out” for self pay care for patients who request it — for this care, a physician can provide care without disclosure risk to insurance companies.
It is openly listed as an option my EMR Practice Fusion although I have yet to use it.
Cheers to all!
Dr Matt Levin
Just east of PGH PA.
In practice since 1988, independent since 2004
Oooh Matt let me know what you discover in that secret section of Practice Fusion. I think many pilots, doctors, lawyers (and their treating physicians actively minimize the mental health issues in chart notes so as not to create a “career killing” chart note. Fatigue instead of depression codes. Stuff like that. Again, this is a compilation of real-life tragedies that have happened to docs and I have that unique vantage point where I am witnessing this for the past ten years. I think most people are oblivious to the risks. Due diligence suggests that we take these threats seriously if we are physicians or care for physicians.
Another Orwellian twist is that a medical board can not only request your medical records, but prevent the treating physician from informing you that you are under investigation, I know that is true in Oregon. So you can be getting treatment from someone who is sending every chart note to the medical board and who will be prosecuted if they tell you that this is happening.
Oh no Joe! One of the most disturbing comments I’ve read all day! Gosh, I hope you’ve never been placed in that situation. But I bet you have. Is this typical of other states? What a nightmare caring for a client while being a board snitch.OMG.
Fortunately the physician has always been aware that they were being investigated. So I was never in that position. But the fact that the clause was there was chilling to me. I checked with an attorney to make sure I was interpreting the clause correctly. It is stuff like this that is pushing me to move away from practicing medicine. It is less and less a profession of healing and more and more a tool of the corporate system and the state, which are becoming one system here.
I have been resisting shifting to mind-body coaching, but I think I need to move in that direction. I’ve been meditating for 50 years and teaching for 30 and my physician patients like learning the skills. I’m working with an attorney to figure out how to structure it to give people privacy.
Could you have predicted as an idealistic premed that you would ever be practicing in such a “unhealthy” environment?
Curious if the Physician Wellness Program in Lane County is impacted by such draconian laws. Do you know if docs are truly safe there (given what has been highlighted in this article & the comments)?
I retired from being the medical director of the PWP in 2021. I had gotten too busy. When I was there it was set up to have minimal charting, the physicians went to the LCMS office, and there was no insurance billing. The work was done by a couple of psychologists and I was psychiatric backup and no one needed meds or hospitalization. During that 9 years I had a number of physicians see me as a patient rather than go through the PWP. I never found it necessary to report anyone to the board. I don’t know how the program is being run now.
Thank goodness that all was well there at PWP. One final question: How many times in your career have you had to sent a patient’s chart to the Board?
Those of us who have been through malpractice trials know that anything public can be brought up. So plaintiff counsel can use a public post about mental health or suicide to say you’re a bad doctor. That’s why I had to delete some of my posts— it’s not worth the risk and that’s sad. My depression had nothing to do with my malpractice case
That is absolutely terrible. Censorship is outrageous
OMG so I just got this email: “Pamela, It’s been a while since we communicated! I would be happy to provide confidential healthcare to providers. My cash prices are affordable, I would document in paper chart format, keep the records secure in my office under lock and key, and could meet with healthcare providers after hours or even outside the clinic if necessary. I am in Arizona, so let me know if I could be of assistance. Thank you for all you do for those fragile overwhelmed fatigued providers that contemplate.”
I recommended that she leave a message in comment section & then realized she would be outing herself and the system might come after her. Man, this is a total witch hunt on our doctors. Control the doctors with fear and we are screwed trying to get mental health care from a system that undermines our health. Kind of like going to the place where you were assaulted or raped and thinking you could get mental health care. Incongruent from the get go.
Question from a surgeon (shared here for anonymity and to get some feedback for her): “Do you have any recommendations for those of us that already psychiatric notes filed affecting us with obtaining disability insurance? How can I make my record “clean”? Would getting an attorney help?”
Anyone know?
Wow. I knew it was bad. I’m a physician and a technologist, and a portion of my work focuses on privacy-protecting technologies. Here are a few more ‘gotchas’ that you may not know about; I’ll also make a few suggestions on how to protect your personal privacy:
1. HIPAA protections only apply to “Covered Entities”: health care providers that bill Medicare. Your school’s drop-in counseling service? Nope. Here’s an article about this issue:
University Of Oregon Violated Sexual Assault Victim’s Medical Privacy, Employees Claim
2. HIPAA has multiple “safe harbors” that allow the release of your medical records WITHOUT your knowledge or consent. These are:
(1) The “Treatments” safe harbor. The healthcare system that you receive care through may enter into a “Treatments” advisory contract with a “Business Associate”, where they transfer your entire identifiable medical history to a third party. Example: Project Nightingale, where Ascension Health legally transferred 50 million patient records to Google.
Google’s ‘Project Nightingale’ Gathers Personal Health Data on Millions of Americans
Google reveals ‘Project Nightingale’ after being accused of secretly gathering personal health records
Google Secretly Tests Medical Records Search Tool On Nation’s Largest Nonprofit Health System, Documents Show.
(2) The “Payments” safe harbor. Any “Business Associate” of a “Covered Entity” can access your medical records without your consent or knowledge if they assist with payment for healthcare services. For example, most large employers, including the Fortune 1000, use self-funded administrative services only (ASO) health benefits plans to provide health care coverage to their employees, where healthcare benefits are managed by traditional insurers such as United Health. If the hospital you work for offers its own insurance plan, then they have legal access to your medical record.
(3) The “Operations” safe harbor. Similar to the payments safe harbor. Any private company that provides “operational” support to health system, e.g. a supply chain management company such as a PBM that manages drug purchasing for your health system, can legally access your medical records.
(4) The “de-identification” safe harbor. HIPAA allows the release of your medical records to any party as long as the records are de-identified by (1) removing certain identifying fields, such as name and date of birth, or (2) using an “expert determination” method where an expert uses a statistical analysis to show that the smallest cohort defined by a specific identifying variable has no less than 20,000 patients. Both methods DON’T work. In fact, the following two articles published in STAT show that 95% of de-identified medical records can be re-identified via certain algorithms that correlate the data in the medical record with external data sets:
How a complex web of businesses turned private health records from GE into a lucrative portrait of patients
He founded what became IBM’s most valuable health database. Now, he’s sounding an alarm about patient privacy
WHAT YOU CAN DO TODAY to protect your privacy, your career, and your life: act as if you are living in an authoritarian state such as China and under continuous surveillance:
1. Create a new persona and false identity for yourself: a new name, a new birthdate, a new profession, a new address, a new phone number, and a new email address. You will use this new identity for ALL transactions related to receiving care for mental health or substance abuse problems. This new identity should be close enough to your current identity to not trigger suspicions.
1. Use cash to buy VISA or Mastercard gift cards. You will use these cards to pay for all online transactions and purchases, including your healthcare. DO NOT purchase more than $200 worth of gift cards at any one store. And DO NOT use a customer loyalty card to allow the store to track your identity when purchasing the gift card. And never withdraw more than $1,000 or more cash at any one time from your bank account.
2. Think like a homeless person. Purchase a personal mailbox with a real street address from a commercial service in a different state if at all possible. Homeless individuals do this. Prepay for at least one year’s worth of service.
3. Purchase a burner phone. Pay for it with cash. Pay for activation of the phone with a gift card. Turn location tracking off.
4. Purchase an email address and VPN service from protonmail.com, one of the most secure services in the world. Sign up for the protonmail.com email address using the phone number associated with your burner phone, and pay for the VPN service with your gift cards. Install the VPN on your phone, and use the VPN-protected phone for ALL internet connections
You now have a fairly-credible identity including an email address, a phone number, and a physical address that you can give to a mental health provider in another state.
Prescriptions should be sent to drug stores far away from you; most pharmacies only require a name, date of birth, and cash to pick up a prescription. ALWAYS pay cash if at all possible. Otherwise, use your VISA or Mastercard gift cards.
Good luck, and stay safe!
WOW! VERY COMPREHENSIVE. Have a meeting now. Will come back and read this again tonight.
I’m rereading this. Wow. Insane. Boggles the mind what one would have to do to ensure privacy & confidentiality. Thanks for sharing all of this info.
This is terrifying. Having worked in both the US and UK, I can say with certainty that UK and EU physicians do not have to take ANY of these precautions in order to get healthcare that they need. It boggles the mind. We need each and every doctor, administrator, and physician body to stand up to the legislators and demand change. Now. Before we lose another 400 colleagues.
Just wondering how to do this without any form of ID with your ‘new’ name and birthdate. Where I live, I would not be able to fill certain prescriptions, nor open a mailbox without a DL or form of ID.
It saddens me that anyone finds themselves in a situation where they have to hide getting care for a health condition because their employer actively uses it against them. I’m not a healthcare provider, but in a profession where I have faced stigma for the struggles I have. There is no support, just gossip. It’s good to see people here supporting each other, and what a beautifully written obituary for what was an obviously brilliant and wonderful woman❤️
Curious what is your profession. I’m sickened that so often psychiatry is weaponized rather than used as a healing art.
My insurance agent (who has been with my family for years) said if I ever need to see a psych, pay cash if I can.
I received this email from the Wisconsin Medical Examining Board. With people like Dr. Wible bringing attention to this pressing issue, maybe things are changing?
Wisconsin Department of Safety and Professional Services
October 2022
You are receiving this update as a licensee of the Wisconsin Medical Examining Board or as a subscriber to this communication.
While attending the Federation of State Medical Boards’ Annual Meeting in April, I listened to a presentation by Corey Feist, the brother-in-law of Dr. Lorna Breen. Dr. Breen, an emergency room physician in New York City, took her own life on April 26, 2020, as the COVID-19 pandemic had begun to stress the health care system and providers of care as never before, exacerbating the existing suicide, burnout, PTSD, anxiety, and depression challenges that were already facing the medical profession. Her death followed her recovery from COVID-19 in the midst of working extended shifts treating COVID patients.
Mr. Feist and his wife, Jennifer Breen Feist, created the Dr. Lorna Breen Heroes’ Foundation in Dr. Breen’s memory to advocate for support of health care professionals’ mental and behavioral health, reduce the stigma that is associated with the need for mental wellness care, and to increase funding for research and programs aimed at reducing burnout and improving mental and behavioral health.
The Heroes Foundation achieved a major success recently in its advocacy for national legislation to address mental and behavioral health concerns among health care providers. On March 18, President Biden signed the Dr. Lorna Breen Health Care Provider Protection Act (H.R. 1667). The Act provides grant funding through the Department of Health and Human Services (HHS) to the health care workforce, hospitals, medical professional associations, and other health care organizations aimed at improving mental and behavioral health among health care providers. It also directs HHS to conduct a three-year root cause study (e.g., the increasing role of systems issues contributing to burnout), a campaign to encourage providers to seek support and treatment, and to disseminate best practices to prevent suicide.
The results of the Feists’ call to action are long overdue. We have learned that, compared to the general population, suicide is disproportionately high among physicians, residents and medical students. The scope of the suicide problem is alarming. Each year approximately 400 physicians nationally take their own lives. That is more than one physician suicide each day, and roughly the equivalent of the combined graduating classes of the two medical schools in Wisconsin-the Medical College of Wisconsin and University of Wisconsin Medical School. Suicide’s lead progenitor, burnout, is also increasingly a concern: physicians are at a 40% higher risk of occupational burnout than other workers. In turn, there is an impact on patients. One finding indicates that between 210,000 and 400,000 deaths associated with preventable harm occur each year, and many may be due to physician burnout.
These figures are difficult to take, but solutions are within reach. Seeking care is essential not only for ourselves but our families, our friends and our patients. As we in this profession know, compromised physician wellness may also compromise the quality of the medical care provided.
Corey Feist’s talk spoke to me personally as the Chair of our Wisconsin Medical Examining Board. He noted that one of the primary factors contributing to physician suicide, including Lorna Breen’s, is fear that physician regulatory boards across the country will take an action against a medical license due to the act of a physician seeking mental health care. This is wrong. That perception prevents physicians in Wisconsin from seeking out the care they need. So let me clarify: As it states in our license renewal application, treatment for medical conditions is not in itself a basis on which an applicant is ordinarily denied licensure when the applicant has demonstrated personal responsibility and maturity in dealing with a mental health issue. The Board encourages applicants who may benefit from treatment to seek it. In addition to focusing on their own well-being and quality of life by seeking care, the mental illness may not lead to functional impairment, physicians may be less prone to harming a patient, and they may be more prepared to provide care with reasonable skill and safety. As for the physician duty to report (s. 448.115, Stats.), it exists to protect patient safety, not to target physicians for taking steps towards their own wellness. To underline the main point, care of the patient requires care of the provider.
Following the Heroes presentation, I requested discussion about mental health challenges among physicians and how the Wisconsin Board might support physicians who need assistance. I am pleased to report that we have made some progress. At our June 15 meeting, the Medical Board unanimously moved to support the expansion of the state’s Professional Assistance Procedure (PAP) program to address licensee mental health issues (in addition to its current focus on substance abuse issues). The PAP is a non-disciplinary program for licensed professionals with substance abuse issues that are committed to their own recovery. It is designed to provide an opportunity for qualified participants to continue practicing without public discipline while complying with the terms of a contract. Unfortunately, the Medical Board is unable to expand the program on its own. A state statute change is necessary, and the authority to change statutes resides with the state legislature and the Governor. So I intend to work with the Board to explore what role it might play in advancing its support for an expanded PAP going forward.
In addition, I want to emphasize the importance of physicians playing a leadership role in reducing stigma. Dr. Breen received some care, but it was brief. She confided to those close to her a fear of being ostracized by her colleagues and a downward career spiral due to a mental health episode. She felt exposed and embarrassed. This is what stigma does. Can anyone say that these stigma-driven fears are uncommon in the House of Medicine, reinforced and perpetuated by the traditions and norms we grew up on, or deny that the prevailing belief is that you will be perceived as unfit to practice or weak if you seek care?
Finally, on a more personal level, after exploring the topic of physician mental health and wellness with some of my OB/GYN residents, one of them, Dr. Alexandra Levy, volunteered to write a letter discussing the issue from a young physician’s perspective. Her letter is included (below). I commend Dr. Levy for having the courage to share her personal experience.
“Physician, heal thyself” – Luke 4:23
By Alexandra Levy, MD OB/GYN PGY4
The vast majority of physicians, at one time or another, have found ourselves sitting across from a patient who has confessed that they are feeling down, hopeless, and suicidal. They are bravely reaching across the aisle for help – and seeking out a healer for it. They believe in us and expect that we can set them on the path for healing.
I’ve spent hours holding hands and exploring fears, pain, and anxiety that have led my patients to such a dark place. I don’t judge them. I know that life is hard, that obstacles can feel insurmountable, that sometimes you’re looking from so deep within the chasm that you can’t really see where you fell in in the first place. And I know this because I’m just like them.
I was diagnosed with depression in 2018. I had a series of really devastating personal events that I did my best to ignore. Externally, I tried my hardest to project a competent intern who was unaffected by her surroundings. Internally, I felt ashamed that I was a fraud. I struggled with the same feelings of hopelessness, loss, and the accompanying shame of “not being strong enough” to solve my own problem. However, under no circumstance would I have ever turned to my supervising physicians for help – because I was deathly afraid of the consequences.
Medscape published a survey of 13,000 physicians this year, and the results are heart-wrenching. Thirty three percent of our colleagues report depression; ten percent report thoughts of suicide without attempt; one percent have attempted. It is not stratified by gender. Both male and female physicians report similar feelings.
When asked by Medscape to self-report why they have not sought help, the quotes all follow the same theme. “I’m afraid that if I spoke to a therapist, I’d have to report receiving treatment to credentialing or licensing boards,” wrote one physician. “Physicians cannot seek help for these issues because if we do that, these temporary issues will follow us for the rest of our careers,” echoes another.
The culture of medicine is not kindness to one another. My colleagues and I don’t mock patients for their weaknesses. We recognize that depression, bipolar disorder, anxiety disorders, and all other mental health problems are generally the result of organic issues and trauma, which is not the afflicted person’s fault. Yet who hasn’t witnessed a relentless verbal beating from attending to resident, senior to junior resident, or junior resident to medical student? Most of us in surgical specialties wear our tears as a badge of honor. Learning to become stoic in the face of horrific trauma, terrible outcomes, and public embarrassment is expected – or you are weak. And everyone will make that very, very clear.
The time for stoicism is over. Mental health is just as important as physical health. Seeking help for any ailment takes bravery and strength. One-third of your colleagues are struggling too. You are not alone. Therapy and anti-depressant medication will not prevent you from keeping your job and medical license. You have worked tirelessly to become the person you are. You matter to so many people.
Your patients need you to be healthy, your family needs you to be healthy, you need you to be healthy.
We need to talk about this. A third of us are struggling in the shadows. We can’t let one more student, one more resident, or one more attending take their own life because they are afraid to get help.
Be the change.
Get Help Now: Suicide Prevention Resources
Professional Assistance Procedure (PAP) Information
General Information
The Professional Assistance Procedure (PAP) is a non-disciplinary program for credentialed professionals with substance abuse issues who are committed to their own recovery. The procedure is designed to protect the public by promoting early identification of chemically dependent professionals and encouraging rehabilitation. It is also designed to provide an opportunity for qualified participants to continue practicing, without public discipline, while complying with the terms of a contract that is closely monitored by the Department.
If you are a credentialed professional struggling with substance abuse issues, we encourage you to review the PAP Instructions and submit an application:
PAP Instructions
Application
Contact Information
Professional Assistance Procedure
Department of Safety and Professional Services
PO Box 7190 Madison, WI 53707-7190
Phone: (608) 267-3817 (Press 6 for PAP/Monitoring)
Fax: (608) 266-2264
Please note that participation in PAP will not exempt a credential holder from discipline. It may be used in conjunction with the formal disciplinary process in situations where allegations of misconduct, negligence or violations of law exist, other than practicing while impaired by alcohol or other drugs.
Information About Administrative Rules
Click to edit this placeholder text.
Pending Rule Changes
Keep current with any pending rule changes affecting your profession by visiting the DSPS website to view the Pending Rules listing.
Administrative Rulemaking Process
Please review the Rulemaking Process page of the DSPS website to learn more about the promulgation of Administrative Rules.
Board Membership
The Medical Examining Board consists of 9 licensed doctors of medicine, 1 licensed doctor of osteopathy, and 3 public members members. The Board’s membership also includes the Chairperson of the Injured Patients and Families Compensation Fund Peer Review Council who serves as a nonvoting member of the Board.
Board Members:
Sheldon A. Wasserman, M.D., Chairperson – Physician Member (Milwaukee, WI)
Clarence P. Chou, M.D., Vice Chairperson – Physician Member (Milwaukee, WI)
Sumeet K. Goel, D.O., Secretary – Physician Member (Plover, WI)
Milton Bond, Jr. – Public Member (Milwaukee, WI)
Kris Ferguson, M.D., Physician Member (Wausau, WI)
Diane M. Gerlach, D.O., Physician Member (Kenosha, WI)
Carmen Lerma, Public Member (Milwaukee, WI)
Michael A. Parish, M.D., Physician Member (Milwaukee, WI)
Rachel E. Sattler, Public Member (Madison, WI)
Gregory Schmeling, M.D., Physician Member (Hartland, WI)
Derrick R. Siebert, M.D., Physician Member (Wausau, WI)
Lemuel G. Yerby, III, M.D., Physician Member (Barron, WI)
Emily S. Yu, Physician Member (Milwaukee, WI)
Information on how to apply for appointment to the Wisconsin Medical Examining Board, or other gubernatorial appointments, can be found through the Office of the Governor using the link below:
Enforcement Actions of the
Board
The Medical Examining Board, in collaboration with staff at the Department of Safety and Professional Services, can take action against its licensees to help protect the profession and the citizens of Wisconsin. You may search for any of the Board Orders listed below on the Department’s website by using this link:
Board Order Search:
Disciplinary options available to the Board
Disciplinary actions are reported to the National Practitioners Data Bank. Available options to the Board include:
Reprimand: A public warning of the licensee for a violation.
Limitation of License: Imposes conditions and requirements upon the licensee, imposes restrictions on the scope of practice, or both.
Suspension: Completely and absolutely withdraws and withholds for a period of time all rights, privileges and authority previously conferred by the credential.
Revocation: To completely and absolutely terminate the credential and all rights, privileges and authority previously conferred by the credential.
Non-disciplinary options available to the Board
Non-disciplinary actions are not reported to the National Practitioners Data Bank. Available options to the Board include:
Administrative Warning: Issued if violation is of a minor nature, a first occurrence and the warning will adequately protect the public. The issuance of an Administrative Warning is public information, however the reason for issuance is not.
Remedial Education Order: Issued when there is reason to believe that the deficiency can be corrected with remedial education, while sufficiently protecting the public.
Board Orders
April 2022-August 2022
Order Number
Order Date
Respondent
Profession
ORDER0007980
8/29/2022
Guite, Christopher A
Medicine and Surgery, MD
ORDER0003234
8/18/2022
Kaiseruddin, Mohammed A
Medicine and Surgery, MD
ORDER0008022
8/18/2022
Kiser, John Patrick
Medicine and Surgery, MD
ORDER0008120
8/17/2022
Komanduri, Mukund
Medicine and Surgery, MD
ORDER0008121
8/17/2022
Bautista, Soliven C
Medicine and Surgery, MD
ORDER0008126
8/17/2022
Rodriguez, Emmanuel N
Medicine and Surgery, MD
ORDER0008119
8/17/2022
Mateer, James R
Medicine and Surgery, MD
ORDER0008123
8/17/2022
Dahlgren, Matthew A
Medicine and Surgery, MD
ORDER0008122
8/17/2022
McMillion, Virgil Waid
Medicine and Surgery, DO Compact
ORDER0008124
8/17/2022
Coonan, Kevin M
Medicine and Surgery, MD
ORDER0008125
8/17/2022
O’Shaughnessy, Irene M
Medicine and Surgery, MD
ORDER0007227
8/3/2022
Maskil, Craig D
Medicine and Surgery, MD
ORDER0008019
8/2/2022
Nelson, Todd A
Medicine and Surgery, MD
ORDER0007226
7/28/2022
Galdieri, Ralph J
Medicine and Surgery, MD
ORDER0007606
7/27/2022
Thompson, Anthony J
Medicine and Surgery, DO
ORDER0008021
7/21/2022
Klopfstein, Jennifer N
Medicine and Surgery, MD
ORDER0007940
7/21/2022
Nosal, James M
Medicine and Surgery, MD
ORDER0007649
7/20/2022
Thomas, Manuel J
Medicine and Surgery, MD
ORDER0008041
7/20/2022
Lu, Kang
Medicine and Surgery, MD
ORDER0008045
7/20/2022
Lenz, Michael A
Medicine and Surgery, MD
ORDER0008042
7/20/2022
Mejalli, Nedal S
Medicine and Surgery, MD
ORDER0008043
7/20/2022
Yount, Beth Judy
Medicine and Surgery, MD
ORDER0008044
7/20/2022
Leiser, Lori A
Respiratory Care Practitioner
ORDER0006795
6/23/2022
Kuester, David J
Medicine and Surgery, MD
ORDER0007129
6/23/2022
Wynsen, John C
Medicine and Surgery, MD
ORDER0008032
6/21/2022
Rowe, James J
Medicine and Surgery, MD
ORDER0008019
6/15/2022
Nelson, Todd A
Medicine and Surgery, MD
ORDER0008023
6/15/2022
Greiber, Kyle
Medicine and Surgery, MD
ORDER0008022
6/15/2022
Kiser, John Patrick
Medicine and Surgery, MD
ORDER0008021
6/15/2022
Klopfstein, Jennifer N
Medicine and Surgery, MD
ORDER0008024
6/15/2022
El-Khatib, Abd G
Medicine and Surgery, MD
ORDER0008018
6/15/2022
Ahmad, Farid A
Medicine and Surgery, MD
A few concerns Myra,
It appears that they are using at least some of the money to fund programs that have harmed physicians: The PAP is Wisconsin’s version of the PHP. Not sure if Wisconsin is quite as bad as other states where doctors fear PHPs and have died by suicide under their “care.” See video: Beloved doctor dies in physician health program. Her husband wants to know why.
Fascinating that they are patting themselves on the back for being so progressive in their email while publicly shaming thirty doctors at the end of their letter.
Yep. Also worry that the funding is going to “study the problem”.
Yes another 50 years of studying the problem. Creating scales and questionnaires, studies, conferences—and then funneling people into PHPs or some such things. Dreadful. Can’t really solve a problem if we are not willing to look at the truth and address the human rights violations in medicine.
What is most concerning to me about this post is that the board chair extolls the fact that WI PAP is now going to cover non SUD issues. However, like almost all PHPs this one still describes itself as existing for the treatment of SUD in licensees. Therefore it is almost certainly, like other PHPs, going to apply SUD contingency management to all comers…which means, if a physician requests help for a pure mental health issue they will be required to contract for years of substance monitoring, according to the guidelines/recommendations of the Federation of State Physician Health Programs (trade association for all US PHPs), which was built upon the model established by the American Society of Addictions Medicine, and its adherence to principles of strict abstinence for almost any illness. Here’s a horror story about a physician who ultimately refused such SUD monitoring for her NON SUD issue in WA, because it vicariously re-enacted her prior sexual abuse, and lost her license and livelihood as a result. What was her impairment? Suboptimal Press-Ganey scores.
Others have reported being denied life or livelihood sustaining treatments for long established diagnoses such as Narcolepsy or ADHD, or even depression on the same basis.
It is not appropriate for any agency to countermand legitimately prescribed treatments (for example, anxiolytics or stimulants for appropriately diagnosed conditions) FOR THE SAKE OF SUBSTANCE MONITORING, yet this is precisely what these pseudo-governmental entities (acting under the auspices of a medical board, typically a state agency) almost inevitably do.
Most states have, for decades, promised “safe harbor” protections to physicians who are in treatment for SUD with a PHP, so that they do not have to report this treatment on medical board applications. However, in order to be entitled to such “safe harbor” protections, the physician must be strictly compliant with all contingency contract provisions. So for example, they can ONLY take those specific medications recommended or prescribed by providers named by the PHP, and not necessarily those that they have been prescribed for years or decades by their own providers. Also, they are prohibited from using many other legal substances (such as asthma inhalers, hand sanitizers, antihistamines, even pickle juice or poppy seeds) that might give false positive test results for alcohol or drugs of abuse on required monitoring screens. When such “positives” appear, the physician can be reported by the PHP to the medical board as “noncompliant” with contingency contracts mandating strict abstinence, and subjected to discipline.
Hardly a “safe” harbor then.
GREAT ARTICLE!!
I agree with all of it! I would add GoodRX is another way to get scripts filled (at a discount) without involving insurance. I have used it with patients a lot.
Honestly, reading through that article just solidified my decision to work outside of the system. I personally don’t want to be a part of a system where I have to hide like that. 🙁 I think the problem is that all that hiding and secrecy is necessary, but at the same time, it only further perpetuates the stigma and feelings of shame. So it’s a catch 22. 🙁
I would of course add that people should try and seek more holistic docs, if possible. Getting put on drugs to numb the pain associated with being a doctor is just a bandaid solution that will actually cause more problems longterm. 🙁
Also, as you know, the ultimate solution is to GET THE FUCK AWAY FROM THE JOB that’s CAUSING your mental health problems in the first place!!! This one is HUGE!!!!! As I know YOU know, most mental health problems are not due to some chemical imbalance but rather a LIFE IMBALANCE. And just getting “treatment” for your “mental health” is BULLSHIT bc these people are having NORMAL responses to ABNORMAL situations.
THANK YOU FOR ALL THAT YOU YOU!!
Really admire the work you are doing in the world. You are a true trailblazer to stand up to the insanity WITHIN (who would guess) PSYCHIATRY.
Love your article on mental health for docs and how they can seek help
My brother had to go cash to see a therapist and drive three hours out of town to do so to keep confidential his sessions. The real issue is when they need meds for depression or anxiety. Then there is a paper trail and medical record of this. Many resort to stealing them and having other co worker write a script for them. They take care of their own.
One of the real issues now that both my parents were subjected to plus multiple friends is physical abuse and neglect by the providers. My father lost his life as a result even with my intervention. These institutions are death camps and all they say at the end is we wil do a root cause analysis which they most likely never did. They, the hospital administrator, also never followed up with me about my fathers death after any analysis. I even fear they bribed the coroner as I knew something was really wrong and nothing was found on autopsy.
Another incident is my mother being placed in a straight jacket for refusing a blood draw from an inexperienced lab person.
Now software is being developed to identify combative patients so they can type/ label them exonerating the bad actors harming patients in the hospital. Hopefully this is addressed soon so these places are safer for all of us!
I am lucky to practice in Michigan, one of the more progressive states in this respect. I’m also old enough to remember times before our current Michigan systems that are designed to help, not hurt, health professionals. I sadly remember many doctors and patients who died due to the fact that health care professionals did not receive necessary care.
Even in Michigan, we have a long way to go. Your cautions, such as avoiding institutional services such as employer or school care, are still unfortunately needed. Behavioral health care, for all of us, should be handled like any other health service need. Physicians can start by educating ourselves and our students regarding professionally appropriate knowledge, attitudes and behavior in this area. We can also advocate for improvement, starting at our own workplaces and educational institutions. We need to take even small steps, such as addressing the nationally used EMR that says “WARNING; you are entering a behavioral health record.” There is no such warning when entering the record of patients with highly confidential medical needs such as STI or terminal illness. ALL of our health services should be equally private.
Please do take care of yourself, it is an investment in you, your family & patient care. How you do this is very important. You have outlined many of the same recommendations that I have made to others. Out-of-pocket, confidential, wellness, etc… Avoid insurance it must always have a dx & a paper/EMR trail if & when you can. But if serious enough, no matter what, get Tx.
Pamela, as always, you speak some hard-hitting truths.
It is a very sad reality that physicians are terrified of getting help because of the potential adverse consequences to their hospital credentialing and state licensing.
Amongst many issues you’ve courageously raised, I want to speak to one here – the misuse of the term “stigma” to convey as though legitimate one of the reasons why docs don’t get help. That term connotes that the doc him/herself is afraid of shaming and being labeled as weak or crazy. While the term might have been applicable decades ago when seeking help for psychological distress and when emotional illness was actually considered a personal weakness or evidence of incurable mental deficiency, I don’t believe that’s the case today, at least not to the extent that it’s being portrayed by AMA, NAM, FSMB and the likes. Most docs – especially younger to mid-career – know well the widespread acceptance of therapy and, where needed, meds. Employing this term puts on onus on the doc, as if to say “you’re afraid of what other people are going to think of you.” Frankly, I think that b.s.
What docs are really afraid of is the irreparable, career-lethal harm that will come from their seeking help. And that harm comes from abusive medical boards, healthcare institutions, and PHPs, the last manifestly set up to help docs. Instead, their exclusively contracted mandatory referral relationship has become a predatory scheme to screw physicians by putting them in an impossible bind that is even worse than Wes Boyd’s characterization of it as extortion. In fact, it is cruel and approaches the level of psychological torture.
No, this is not stigma. This is overt sadistic abuse, putting docs in an impossible situation and forcing them into a predatory regulatory capture system that abuses them even more, gaslighting them about their newly diagnosed “impairment,” all the while portraying their services and concern as benevolent. And I believe there are many aspects of it that are overtly illegal. However, the legal system itself is ill-equipped to appropriately and aggressively fight these abuses, not least due to the sheer immensity of the cost and effort of assertive litigation.
Yes, in addition to exercising extreme caution in getting truly qualified and trustworthy help, I encourage docs to connect with each other and learn from advocacy groups the applicability of multiple laws that can be used – with sufficiently informed counsel – to protect their rights. Amongst these, the ADA; HIPAA( and its more recent modification the HITECH Act); 42 CFR Part 2 governing strictest confidentiality of alcohol and substance-related treatment; civil rights protections against unwarranted forced psychiatric evaluation, amongst others.
There is absolutely no reason why docs should be terrorized by these entities. And if the various medical associations that were formed to protect physicians’ career well-being weren’t such complicit cowards, this reprehensible torture would not be allowed to continue.
And again, I want to thank you for the extraordinary, deeply compassionate work you do. You have saved countless physicians’ lives.
Agree 100% with the professional abuse and vilification, retaliation against doctors who even consider seeking help. I do think among some group (Asian immigrants, for example) there is a HUGE stigma to admitting a mental illness (even if occupationally induced). So maybe stigma applies more to the personal cultural, religious, family-of-origin realm. Thoughts?
I suspect you know more about the prevalence of stigma in certain populations, esp as they pertain to the seeking/avoidance of MH care. My population is predominantly docs who’ve been abused by boards / PHP / sham peer review. Their fears re seeking treatment or having been in tx were around the harm that resulted.
And yes, I can readily see how certain cultural/ethnic populations might be more susceptible to stigma and thus avoiding seeking help.
Bingo! I gotcha Kernan.
Hi Pamela,
Great article. So glad you mentioned confidential peer support outside your employing org.
Please consider adding our Physicians Anonymous peer support groups — free, confidential, anonymous, facilitated by and for doctors — to your resource list, and in the article above? They happen online several times a week on different days and times.
Pamela,
Thank you for continuing to fight the good fight on behalf of all healthcare practitioners at a time when they are needed more than ever, but are most at risk. We want and need competent health care, but put so many obstacles in the way, I see more and more health-care professionals, including psychiatrists, who are becoming “health coaches,” giving up their licenses, etc. so they can be free to offer help to others without putting themselves at risk in ways that their profession often requires. I continue my own work with men and their families.
Check out our latest offering at MoonshotforMankind.com
Yep. I retired my license in 2021 and I am busier than ever (without a regulatory board).
This is horrible. I live with an individual seeking their best. But the business world and professional career cannot accept the human condition. Even if their business is the human condition, you aren’t supposed to be anything but well done. No help for you while you drain your human mind soul and body for medical practice. This immorality causes them to break further
In these days of electronic expediency there should be little difficulty in setting up patient notifications when their EHR is accessed. I wonder what a health care entity would do if a patient asked for an audit trail of their record.
HIPAA should be amended to include these notifications.
It’s really eye-opening to read about the struggles doctors face with mental health, especially when they feel like they can’t seek help due to the stigma. This article does a great job of highlighting the need for confidential support for physicians. I hope more people in high-pressure jobs feel comfortable reaching out for help. There are services that provide private, discreet mental health support for professionals who need a safe space to talk.
As a primary care provider (now retired) I was owned by a hospital based group. I had a number of physician patients and was forced several times to battle the coders who wanted to place diagnostic codes for Major Depressive Disorder on these physician patients because they were taking low dose antidepressants for mild anxiety or sleep. They were not dealing with any major mood disorder and the meds were probably sub-therapeutic for a true depressive disorder but coders insisted that more than 6 months of any dosage was a major depression and would get paid more.
Quite the nightmare.
Still so unbelievable that we have to waive our HIPAA rights to acquire a medical license.
I am a dentist and been referred to my states PHP for treatment…. They are given me a diagnosis my current psychiatrist disagrees with that has been seeing me for a few years. I would love to speak with you in regards to some advice! Thanks!
I am always avialable for same-day sessions here.