Medicine is full of ethical dilemmas that we often have to face alone. Here’s one I’ll never forget.
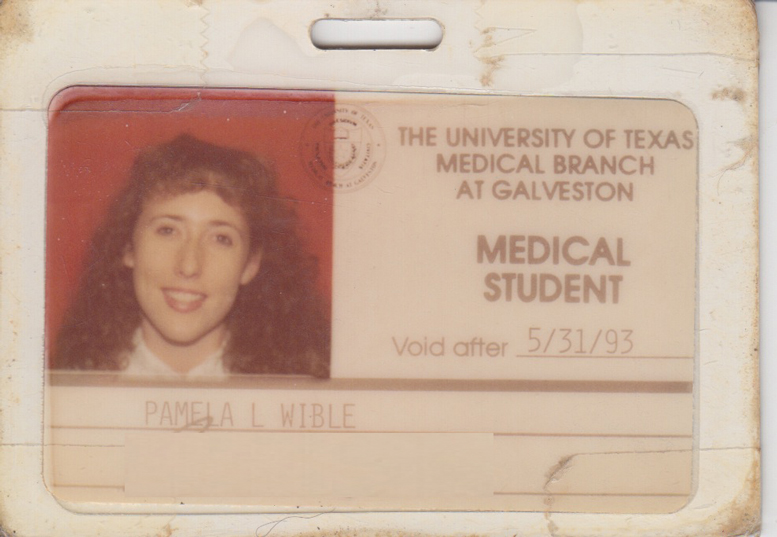
As a med student at University of Texas Medical Branch at Galveston, I had to provide health care for Texas prison system inmates, many on death row.
They say everything is bigger in Texas, and they’re not just talking about hair, land mass, and guns. Turns out Texas leads the nation in executions performed per year (1/3 of all US executions)!
In fact, the prison hospital is conveniently attached to the main university hospital like right next to my apartment.
Anytime, day or night, with a flash of my school ID, the guards press a button and I’m in.
I remember the massive door opening ahead of me. Then a series of steel gates unlocking one by one as I made my way past rows of caged men.
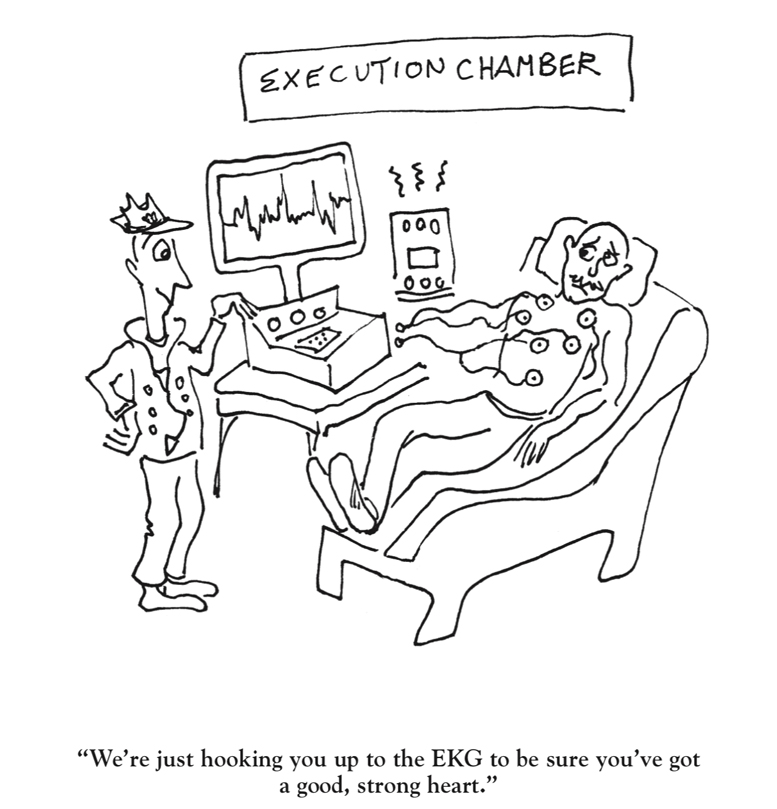
Death-row health care is an oxymoron.
How do I reconcile “first do no harm” with the death penalty?
How do I care for someone soon to be killed?
I’m only twenty-three years old and med school hasn’t prepared me for this. Imagine little me as a young naive med student just standing alone and totally baffled by the ethical dilemma ahead of me. (of course, I couldn’t act like I was uneasy)
I believe all patients deserve the same kindness and respect. I’m basically an idealistic humanitarian who believes everyone is good at heart and those who aren’t have been wounded and are terribly afraid of something.
But all the rules of life and medicine are not the same on death row.
I’m in a place where “How are you?” is a loaded question, a place where men find Jesus and prepare their last statements before lethal injections.
I enter a cell. Sitting in front of me is a white man in his fifties recovering from a hernia repair. As I take his blood pressure and listen to his heart, I wonder how many people he may have shot or stabbed or killed.
“Blood pressure is normal. Your heart’s good.”
“Thanks, Doc.”
He disrobes and I examine his groin incision, testicles, and penis. And I wonder how many women he may have raped or dismembered.
“You’re healing just fine. No signs of infection.”
I flip through his chart to see how I may best serve him. I notice his cholesterol is high.
“When was your last complete physical exam?”
“They check me pretty regular,” he says.
Here’s where it gets really confusing for me. He’s due for a colonoscopy, but do we do colonoscopies before executions?
And I want to discuss his cholesterol, but first I need to know one thing: can death-row inmates get heart-healthy meals?
This is completely nuts.
I haven’t treated anyone on death row since med school (not exactly my ideal patient in my solo practice), but I’ve had some patients just out of prison—mostly for non-violent crimes like marijuana possession. And I’ve had other patients involved in unusual possibly illegal activities.
Hey, as long as you’re not hurting anyone your secrets are safe with me . . .
By the way, if you’re thinking of jumping off the grid from big-box medicine, I’ll walk you through how to liberate yourself from assembly-line medicine. Contact me for an invite to our free webinar.
Ethical dilemmas in medicine are numerous. Is it safe to practice assembly-line medicine in seven-minute visits? Should folks on death row receive free preventive care that isn’t even available for law-abiding citizens?
Opening the conversation on the hidden doctor suicide crisis has been an ethical dilemma of huge proportions for our profession. I certainly never predicted that I’d be inserted into the aftermath of doctor suicide scenes leading eulogies for my lost brothers and sisters in medicine.
I guess jumping into the unknown has it’s benefits. I’m totally fearless now in a way I never was walking among my patients on death row.
What’s the weirdest ethical dilemma you’ve faced as a physician?
I’d truly love to know. Please post (even anonymously) here.














we are taught detached concern which is an oxymoron and to deal with patients not care for them and treat a disease, “here’s a pill for your depression, and not the person who has the disease and why they are depressed. Medical information is not an education.
Detachment seems so unhealthy. I never liked the notion of professional distance (except maybe on death row).
Ironic. I went to a college campus doctor at 17, who diagnosed me with depression. I couldn’t afford counseling, so he had me go to him once a week, and he counseled me instead. Detached? Nope. Wonderful doctor? YES!!
Oh man so many! Helping install fancy insulin pumps at the same clinic where other patients were going hungry to afford their insulin so the nurses GoFundMe for them. Helping inject a $300,000 spinal medication for children who didn’t have much life expectancy in the morning followed by an afternoon hearing how a mom rations out her single inhaler between all her children and herself.
Is it EVER okay to decide care based on insurance coverage? The entire medical industrial complex we live in is an ethical dilemma. This is not healing, it’s not human.
Wow. I would hope that this does not happen in Canada and UK. At least is other countries there may not be this unethical disparity in access to care and meds. OMG. So sorry Giselle.
Dr Pam..I have followed your site for years,I wish one day I could actually meet you. I’m not a physician although I would have been had the military not misdiagnosed me. Sadly,it continued with the VA. What caught my attention to text you is that you are speaking about the very issues I’m finding totally exacerbating. I have written before on the activity of patient profiling.Somehow I know God is listening because no one here seems to be. Dealing with physicians who admit they think they are God,makes it difficult to converse especially when nothing you say to them is true,you simply lie because…. The way things have changed due to someone deciding that ALL pts even legit ones who have depended on opiates for quality of life,the very ability to function,not as candy but as last resort. I am almost ready to join the ones who have found that life hurts beyond physical pain,when the physician intimidates,demeans,bullies,defamed with unethical behavior calling the person mentally unstable because they believe in God,and refuse to agree with the arrogance leveled at them. What do you do when you are fearful of medicine because of adverse effects YET the Dr says you’re a liar,you just read the side effects and chose some thinking you’d get pity. To be given another drug,only taking this one,you can’t see because double vision so bad you can barely walk straight,but once again,you are told you are simply fabricating for sympathy. I’m 65yrs,and my pain regime for almost 25yrs never had to be elevated.The MEDS were last choice after ALL OTHER attempts to effectively treat me,yet sudden termination,not because I had an overdose because there wasn’t any reason except I disagreed that my doctor did not know everything and I felt his approach was bordering on unethical behavior and abuse.I’m now completely without anything for pain after 25yrs and I can barely function.I can’t afford to keep paying to have chores done. I have asked for assistance,even my thyroid Dr says this continues to deranged the treatment plan he has,but the doctor won’t even listen to someone who knows me better and longer. Abusive behavior,I can understand if a person felt threatened but the doctor has caused so much unnecessary pain and suffering just because he can. I’m sorry for doctors who have to endure such bosses as this while training…but I’m a patient being deliberately abused with zero accountability.because this is happening
within the Veterans Hospital.Too many suicides are being perpetrated by doctors abusive unethical behavior. It has to stop!
Fear-driven assembly-line medicine is harmful for patients and doctors. We went to medical school to help and heal others and unfortunately have been locked in a cycle of abuse. We are allies and blaming each other is unlikely to be a winning strategy to overcome what ails us. I am so sorry you are suffering.
Pamela,
We have a dilemma here in California. A person with no family has a very poor prognosis. The person is kept in the ICU in a full code status, unconscious and ventilated, multiple vasopressors, blood product transfusions, surgical procedures, dialysis etc…etc… until death which can be weeks or months because no doctor will make the patient a DNR status. One patient came from a facility with a DNR paper but the second page was not signed by a doctor so the patient was kept in ICU as a full code. I don’t know what happened after that but by the time I found this information, the patient had been there for several days. Medicare pays for it. Another patient, the story was overdose and possibly intentional……..the guy looked almost dead when he arrived…. full efforts to save him, knowing that he is going to die and we are just prolonging death. I tell myself that the only thing possibly good that comes out of these cases is that it gives the nurses experience and practice to use on the patients that can actually recover. I have no control over this. Its a waste of resources for sure. When the legal system is involved…. no one cares about the expertise of doctors unless the lawyers direct the particular expertise to be useful…. lawyers have more power than doctors…. Its very scary actually that lawyers have so much more power than doctors do when it comes to healthcare… The practice of defensive medicine exists because lawyers have a power over doctors practice yet they are not trained as doctors. Pamela…. I am a DO NOT RESUSCITATE. DNR. I AM A DNR. I dont trust my husband okay. If anything happens to me, I do not want to be intubated or tied down in the ICU. That is my worst fear. I am claustrophobic. I watch what we do to people in the ICU, especially old people who just want to be left alone. I feel so bad…… so bad……Its terrible….. terrible….. what we do to people. And when the person has made their wishes known but become confused or unconscious and then the family goes against the wishes of the person…….horrible horrible….. I would rather die than be subjected to what these people endure in the ICU. I never want to be in the ICU. We are a cruel species, humans. In the name of helping,healing, and protecting we violate basic human rights. We tie them down. We deny food and water, we stick tubes in holes and needles everywhere else, while they scream…. We leave them in pain without adequate pain control. We give them diarrhea that scorches their skin, we treat them like bodies, not human beings….. its horrible…….every day I live in dilemma, in the ICU.
Shalena you are handing over your DNR orders to me. OMG. The ethical dilemmas we face in health care daily require some sort of debriefing. This is insane.
What a great story and experience Pamela. When I worked in trauma at San Francisco General we would routinely have patients, with guards, from San Quentin. Like you, I often wondered what they were incarcerated for BUT REALLY DIDN’T WANT TO KNOW! I treated them like any other; with dignity, compassion and respect. Peace and love to you! Charley
Definitely distracts from the care if one focuses on the crime.
well, i gotta say, you are certainly interesting. definitely never heard a doctor talk like this before
🙂
Hi Pam,
cared for death row inmates in Pennsylvania as a young doc working as a sub-contractor. It gave me a different perspective on life and healthcare.
What bothered me most was the huge amount of intelligent and talented men( and women) who claimed innocence but were unable to afford competent legal representation.
Derrick
So sad. Huge racial (and economic) disparity in our criminal justice system.
Dear Friends, Pamela does it again, and again, and yet again, and with such insight. Anyone who was not touched by this piece and who would not question the ethics involved may need to have a psychiatric evaluation done. Dr. Wible is trying to make us aware of what we’re doing as a society and what our actions are doing to us. Way to Pamela! James M. Kenyon
I’m lucky to work in the UK, where we don’t have the death penalty and where the NHS pays for everything for every patient, rich or poor, good or “bad”.
I’m training in psychiatry, and am coming to the end of a 6 month placement in forensic services. It’s fascinating to meet the patients, get to know them as men, then look into the violent offences* that have found them at my clinic; and has really helped me to iron out any judgmental attitudes I hadn’t already shaken! In this setting it’s important to know what they’ve done – to assess ongoing risk, to see what it says about their mental illness, and to see how that informs the treatment they need.
*Not all of my patients have criminal convictions- some have been admitted to general adult wards, and assaulted staff and patients so often they’ve had to step up to PICU, LSU and on to MSU, but have been so unwell at the time that they haven’t had the capacity to answer charges, so have never been to court.
In the Trust where I work, there is a LOT more funding for secure services than for other clinical areas, and by all accounts that’s a national pattern, with higher security settings attracting the most money. It’s a risk-to-others thing; a lot of my chaps have killed, so we don’t want to discharge them until we’ve done EVERYTHING to rehabilitate them so they don’t reoffend. But this is a step in my training and at heart I’m an old age psychiatrist to be; and as wonderful as it is to see my forensic patients building complex metalwork projects in OT, seeing clinical psychologists regularly for years and learning to sail on their Section 17 leave, there’s a bit of me that wants to scream “not fair!” and snatch some of those resources for the dementia patients who get a colouring book and half an hour playing with a beachball, or the 20-bed elderly functional psych ward where only 3 patients at a time get psychology because there isn’t the funding.
Sorry, bit of a rant – and nowhere near the unfairness seen in the US, although our government are pushing for privatisation.
I’m trying to think now of what my weirdest ethical dilemmas have been! Might have to come back to that one, it’s an excellent question!
Thanks Bex! Always good to hear how things are handled (or mishandled) in other countries. I know we can do better.
As a clinical and political research psychologist I have practiced for decades with concern initially for individual clients and couples but eventually for our whole nation and for the whole world. I have learned how to reliably measure the violence-proneness of teenagers only to find that school systems don’t want reports revealing details on a given individual for fear of “political” backlash by one or the other of the student’s divorced parents. I have developed a technique for accurately measuring the warmongering-proneness of historical and political figures, past and present, but when I sent the article to a professional journal they told me that the ratings have to be done by academics, not the general public, even though when the general public uses the instrument their scores for leaders are extremely reliable and valid, just as a steel tape measure gives accurate information that enables carpenters without degrees in physics to measure building materials accurately enough to create safe and worthwhile structures. I have recently had half a dozen adults rate and measure the warmongering-proneness of our president, whose scores are high, similar to those for G.W. Bush. Their scores are between those for Genghis Khan and Attila the Hun. Dare I publish this information for the general public to see? Would I put at risk my clinical contracts with the Veterans Administration and the Social Security Administration if I published such results?
I have data on a quarter of a million children from around the world over a 10-year span that shows human intelligence is dropping 6/10 of an IQ point per year. The cause appears to be air pollution, based on correlations between the IQ scores and World Health Organization air pollution data from the year 2014. In as little as 50 years average human intelligence could drop 30 points such that half the population will be mentally deficient and unemployable and the smartest of us will only have average intelligence, too low to earn Masters degrees or PhD degrees. Too low to complete law degrees or medical degrees. Will I find a professional journal willing to publish these findings? Or will pressure from the fossil fuel industry prohibit this? I’m 79 years old. Do I owe it to my wife and myself to retire, and live carefree for the last decade or two of my life? Or am I morally bound what I have discovered as a concerned member of the community who has enjoyed vast privilege to learn the dangerous information I now hold in my head and heart? Am I morally bound to publish what I know, come what may?
What a dilemma this is. My outlook on healthcare as a future doctor is that everyone should have proper access to healthcare, but this def puts a spin on it. When I was in line checking in for my own chemo appt, the gentleman behind me had been escorted in wearing shackles, with two police officers. I knew my infusion bill would be about $14K for the day which thankfully my insurance picked up “most” of it. This guy behind me was getting it for free. Who do you have to kill to get some free healthcare?
Pam what I think is crazy is that wardens botch executions left and right when any medical student could 10 different ways to efficiently and painlessly kill someone with readily available medications. Somehow medical societies decided it would be unethical for a doc to participate in an execution. Personally I think one can clearly aid someone in their painless passage to death without broaching any ethical line, nor does one even have to support the death penalty. Then again I have no problems with abortion either. Ethical dillemnas abound.
I’m looking back on my training so far, and wondering whether I’ve actually had many true ethical dilemmas. The occasions when I’ve felt stuck haven’t been between two ethical principles (apart from autonomy vs beneficence/non-maleficence, which is psych bread and butter), but between What Is Right and The Boss.
The biggest, I think, was as a very junior doctor, with the additional stress of very close monitoring by my regulating body because of a mental health condition. I was working on a stroke ward, and a patient came in with a huge TACI, no movement, no communication. Standard procedure at 2 days was to start NG feeding and monitor for improvement- some patients will make something of a recovery from this, others won’t. The lady didn’t have relatives, we had no contacts for her, but at about day 5, friends started to appear- and beg us to stop tube feeding. She had very strong views on it, no artificial nutrition or hydration. My consultant ignored them. I tried to argue, but he was adamant. A few days later, a friend produced a valid Advanced Decision to Refuse Treatment. At this point, legally, it is BATTERY to continue to feed. My consultant insisted we carry on – it was against his religious beliefs to stop lifesaving care. I argued, the nurse in charge argued, I vaguely threatened (in a very non-threatening “dizzy trainee looking for education on why I don’t understand this totally valid thing we’re doing” way) to take it to the Medical Director (who was giving me guidance because of the regulating body thing), and the consultant weakened to “we’ll keep feeding while this tube is in, but if it falls out, we won’t insert a new one”. I had him commit it to writing- HIS writing – but how was a feeding tube going to fall out of a totally immobile patient? I waited for him to leave the ward, and popped in on the patient to check that her symptoms were controlled and she wasn’t in any pain. It remains a mystery how, by the time a nurse went in 30 minutes later, that tube had come untaped and fallen clean out 😉
I’m getting better as I progress through my training (and now that my regulating body have stopped policing my every move) at standing up for what is Right; and as I get more settled in my new hospital, find I’m more likely to have a nurse or several behind me, because they know I’m behind them when they’re Right. I just hope I stay approachable and human enough that they’ll tell me, if and when I make consultant, that I’m wrong!
THANK YOU for defending the patient’s right to die.
Loved this!
My ethical dilemma is strange. In my first residency, our director did not believe in birth control. He was 38 and had 13 children. I asked him if he was Mormon or Catholic. Nope, just a personal religious belief. I asked him if he believed in Viagra. He said yes because it treats a medical condition. Thus, I trained in Family Medicine with the ethical dilemma of strongly believing in birth control but lying in charts to prescribe it for patients. I didn’t want to be judged by the director so I had discussions with patients requesting or needing birth control and then prescribing it without documenting it in the record. Later in my first year, a child came to me who was impregnanted by an uncle who raped her. Her mother, she, and her twin sister sat in my office crying and asking me about options. I gave them the speech I was expected to give by my program (who also forbade the referral or giving of any information regarding abortion services). I then proceeded to tell them ALL of her options with numbers to Planned Parenthood in Atlanta including termination of unwanted pregnancies. I delivered her later that year and it was gut wrenching. She labored next to her sister in the room. One was delivering a baby conceived by rape and that event would alter her life forever; the sister blew bubbles with her bubblegum and watched TV while she labored. I felt conflicted about whether the “talk” encouraged by my very pro-life program had done this patient harm by clouding her decision. Despite many calm discussions with this director during my time, I never changed his mind nor he mine about women’s rights to care for reproductive services. I’m sure I upset him towards the end when I finally shot back a comment that went something like this….”Well if you think birth control is wrong because you are preventing a baby God wills then perhaps Viagra is just as wrong because perhaps God doesn’t want that man to have an erection.”
I could cite so many dilemmas that I can remember. But this was the first biggie that made me acutely aware of the challenges I would face as a physician!
Pamela,
Talk about skipping a beat, ladybug… You’ve got to write a book!!! I don’t think you realize how absolutely special and different you truly are.
Not that I know many physicians,… but Pam,… you’ve got one amazing background, not to mention your youth!!!
I could sit and read your stories all day… they’re thoughtful, insightful, and often, soooo amusing…
Yes- I say WRITE A BOOK!!!! A novel idea, eh?
And to all of your lucky patients,… I don’t think they realize how blessed they truly are! Your hearts made of a super sweet, squishy sort, … full of loving, yet rock hard constitution girliegirl…
Yes,… lucky, I say! Most folks docs have none of these amazing life experiences you have, muchless any of these very, very unique ones!!!!!!!!!
Hey- enjoy your weekend, kiddo!
Oh,… by the by,… you may find this comical:
I have a colonoscopy Monday at 2:30 at UNC-Chapel Hill lol
HOW IRONIC WAS THIS…(and, I plan to share your post with my doc,… LOL
MUCH LOVE,
Carolyn
I just want to add that not everyone on death row has done something horrible. Unfortunately, there are many on death row who are innocent and some who will be found innocent through, The Innocence Project. So treating them as human beings and having a kind medical student may be a worthwhile endeavor. Overall, prisoners do not get the best healthcare or preventative care, and they should.
Absolutely Hisla.
As an anesthesiologist, I got a call from my ENT surgeon one afternoon regarding a patient he had just seen in his office. The patient is a 62 year old male with a supralaryngeal pedunculated mass of uncertain etiology, and given the propensity of the mass to suddenly obstruct the airway the surgeon wanted to schedule its removal as soon as possible. I quite concurred, but suggested to the surgeon that such a procedure might be more appropriate to an inpatient hospital OR, and not at my outpatient surgery center.
Unfortunately, the patient was recently unemployed, had lost his insurance coverage, and becoming eligible for Medicaid would take too long for a man whose next breath could literally be his last. As such, the patient would have to pay for the procedure out of his own pocket, and it would be about 10 times more expensive at the hospital, and the for-profit hospital wasn’t receptive to giving him a break on the charges.
Thus it was a conflict between clinical and financial considerations, and any surgical misadventures or subsequent hospital admission would be considered detrimental to not only my reputation, but that of the surgery center. I reluctantly agreed to proceed.
The patient arrived on the morning of surgery, and as I’m getting his history the only thing he wants to discuss is how he’s going to pay for my services. Keeping in mind that he had a life-threatening pathology, I told him we could deal with that particular concern at a later time, but he was quite persistent. I finally told him that I would not be sending him a bill for my services so that we could get on with what I considered to be more pressing matters at hand. At this he was dumbfounded, and finally asked why I would do something like that. I simply replied, because I could.
Once in the operating room, the more immediate problem became airway management. Simply manipulating the airway might precipitate an airway obstruction which could result in anything from brain damage or death to tracheostomy or unplanned admission. And so, with no small trepidation I sedated the patient, instrumented the airway and saw…nothing resembling normal airway anatomy. And as the patients oxygen saturation and my spirits began to drop, I told my surgeon to prepare for tracheostomy. As he was preparing the instruments, I managed to move the pedunculated mass out of the way with the endotracheal tube, and insert the tube into the trachea. My spirits lifted with the patients oxygen saturation. The lesion was then excised, and the grateful patient discharged home without complication.