Shawn C. Kelley, M.D., died by suicide under the care of Washington State Physicians Health Program. She was referred to the WPHP based on one unsubstantiated allegation unrelated to patient care. Her husband shares his thoughts and experiences about the program tasked with protecting his wife—and he appeals for a more objective and transparent process for helping vulnerable physicians. (interviewed on date 9/20/19)
I’m Vince Nethery, professor of clinical physiology, and my wife Shawn passed away six years and 55 days ago. I received a phone call at midnight on a Saturday night, and that’s never a good time to receive a phone call. It was from a law enforcement group in Seattle informing me that she had passed away. I got in the car and drove to Seattle. The circumstances that led to this are complicated, multifactorial, and questions come up all the time. We will probably never get answers to many of the questions, even today, six years later.
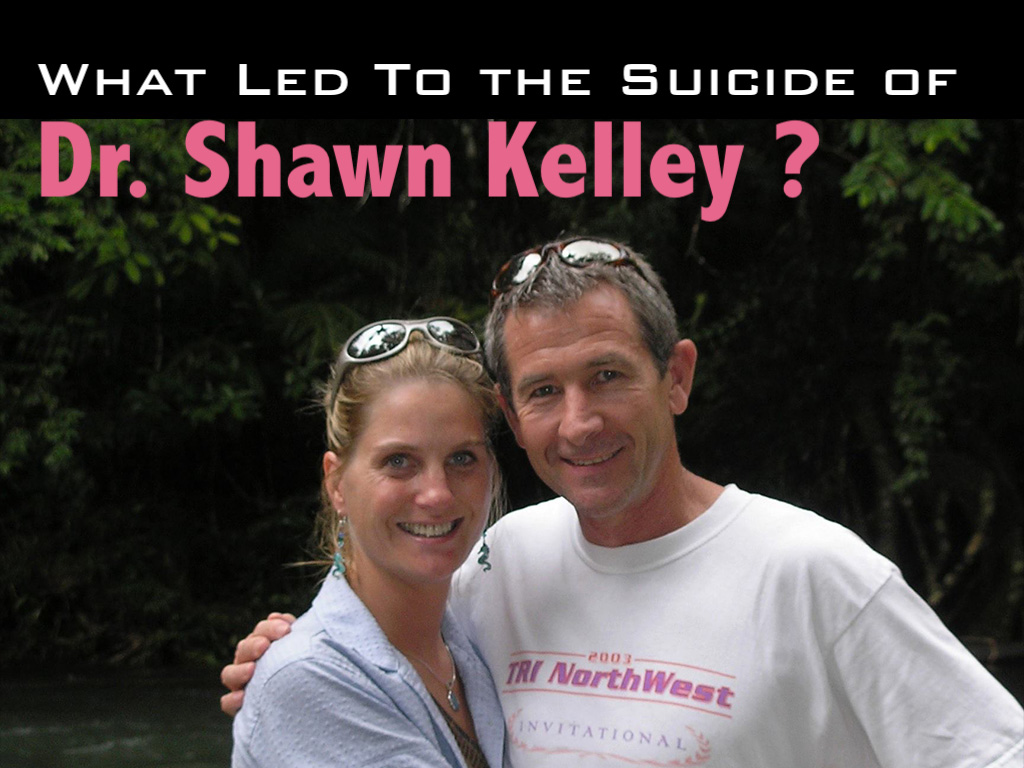
Shawn was a loving wife, tremendous mother of two children, 1,000 patients or more lost their physician, the medical community of North Central Washington lost one of their longtime members, and how this all came about, as I mentioned, we’ll never know. What we do know is that there are circumstances that led to some level of discontent in the workplace with one particular individual. That individual filed a complaint to the medical director of the hospital. Later we learned the complaint had something to do with an out-of-work experience. It was a private function that had nothing to do with the workplace. The complaint expanded to the workplace with the individual saying they would never work with Shawn again. We asked for an investigation to say, “Well, what’s the basis of this? Give us a root cause analysis of the situation. See how many others were affected by some allegations of . . . I don’t really know what they were, but whatever those allegations were.
Ultimately, Shawn was directed to go to the Washington Physicians Health Program. She wasn’t exactly sure why, but she was directed to go there and based on that directive she had no choice but to go. She met with two individuals in a conference room and those individuals discussed or asked or interrogated her, I don’t know, I wasn’t there, for about 45 or 50 minutes. At the end of that time period, the medical director of WPHP came into the room and within five minutes indicated that she was to go to an inpatient facility within a few days [Note: she was to pack her bags, leave her family, and travel to Georgia to enter their “preferred” inpatient facility at her own expense for four days. She was not given a diagnosis or a clear reason for their decision].
She walked out of there. She called me. I remember it as clear today as it was then. She was incredibly upset, as anybody would have been I would think.
We communicated about how it went and I asked her what was the basis for the directive that came from the psychiatrist at WPHP. She indicated that he was in the room for maybe five or 10 minutes and when he made the directive to her that she needed to go, she asked why, and he indicated to her that her speech was pressured or pursed and that was the basis for his evaluation. I wasn’t exactly sure what that meant so I asked Shawn and she indicated that, “Well, that’s usually a sign of stress, that you have pursed or pressured speech, and it’s a sign of stress.” And she said, “Well, how do you think I would be? I just spent 50 minutes in this meeting having these fairly one-sided conversations with two individuals and I was stressed out. It would be unusual for somebody not to be stressed.”
I asked her who the two individuals were who were in the majority of the conference meeting with her and she wasn’t sure. She knew the names because they introduced themselves, but she didn’t know what their role was, what their qualifications were.
A subsequent meeting with the medical director of WPHP many months later where I accompanied Shawn to that meeting, I asked the medical director who the two individuals were.
His first response was, “They are professionals in WPHP.”
I said, “Okay, are they trained psychiatrists?”
He said, “No.”
I said, “Well, perhaps they’re psychologists, right, they’re certified through psychology?”
He said, “No.”
I said, “Well, do they have a bachelor’s degree?”
He said, “They have a substance abuse certification.”
I said, “Okay, how do they get that? What level of education do they need to get that?”
He said, “They received that through a program at a local community college.”
I said, “So we’re making a decision that’s going to have a significant impact on somebody’s life here on the basis of 45 minutes of questioning discussion with two individuals who have a community college certification. That doesn’t seem right, does it?”
He said, “They’re professionals in our organization.”
I then followed up with the medical director and I asked him, that given the heavy emphasis in medicine today and for the last decade or more, on evidence-based being the base for making critical decisions, I asked him to explain what the evidence base was for the medical decision that he made. He got up and left. Came back five minutes later and said, “Our meeting is finished.”
We had spent about 90 minutes in this meeting with him to try to get to the bottom of a basis for his decision. He would not provide a rationale for it, none whatsoever. He provided no evidence to support it beyond the hearsay or the allegations made by a single person that were unsubstantiated in a following followup investigation of the setting in which this individual worked.
I was flabbergasted, actually, that an individual who had so much quote unquote “power over” the functioning of a physician could make those types of decisions and make them without being able to provide a justification, especially to the person to who that decision was being rendered. I’ll take a break.
Of course with 20/20 hindsight there are probably some things that might have been done in a different way that may have averted the outcome that did exist. One area I personally think would have benefited this particular situation would have been the development of a clear pathway to the resolution. That is, what are the specific areas that need to be addressed and completed in order to have a return to normalcy of the workplace? It seemed like we were forever chasing a moving target. One thing was asked to be done, it was complied with. At the end of that, there was another thing, and that was done. Then there was something else. And at the end of the day there was no clear pathway to resolving the matter and allowing individuals to return back to a professional environment that they were trained to be in.
In addition, the establishment of an ombudsman type of person within the setting to provide an objective evaluation of it without the workplace evaluations being conducted by essentially some of the individuals who were inherently at the root cause of some of it. And that didn’t exist. There wasn’t an objective individual who was doing a root cause analysis to find out at a very basic level the underlying factors and the veracity or lack thereof of the allegations that were made.
There was really no support provided from a physician perspective. Shawn felt like she was out there like a shag on a rock. Just at the whim of whatever direction the wind was blowing. To put a more defined mechanism in place and to have a clear set of directives that need to be addressed, to find out whether they need to be addressed, and then determine the pathway to follow for addressing them, if there is validity to them, would have been extraordinarily helpful in this case.
Questions that remain unanswered:
1) Why is it that one disgruntled individual in a social setting can leverage a complaint (unrelated to patient care) against a competent physician and undermine a doctor’s entire profession?
2) Why are two individuals with 10-month community college certificates in charge of determining the fate of a doctor’s career in 45 minutes?
3) Why are physician health programs not using evidence-based medicine?
4) Why is there a lack of transparency in physician health programs so that the physician and family and not given a diagnosis and treatment plan with a clear pathway to resolving the unsubstantiated allegations against the doctor?
5) Why are physician health programs unwilling to answer questions about physicians who have died by suicide under their care?
If you have answers to these five questions, please share your insight below as Dr. Shawn Kelley’s family deserves to know what happened to her.
Questions raised about physician health program safety:
Doctors fear PHPs—why physicians won’t ask for help (TV report)
Physician Health Programs: More Harm Than Good
Physician health programs: ‘Diagnosing for dollars’?
Top 10 things you need to know about PHPs
After investigating more than 1,300 doctor suicides during the last seven years, I’ve noticed a disturbing trend in which physicians have been dying by suicide under the care of physician health programs. Victims are sent to PHPs for unclear reasons, mandated to one-size-fits-all “preferred” substance abuse treatment centers for up to five years at great personal expense—even though many had no substance use issues. If you have been harmed (or helped) by a PHP, please share your story below.











I just read your post on the Wa. php followed physician who committed suicide. My husband had also been directed to go there to the wa php. I was in that same conference room with two staff and the director… he wouldn’t follow through with the process of an intake interview. Unfortunately, he lost his license this year and pretty much lost all after that. We are no longer Together…. so sad after a decade together. He’s basically homeless. I tried for years to steer him in your direction but his ego kept him from reaching out. He voluntarily gave up his license and is no longer a family practice physician.
Hello Pamela Wible, do you mind if I contact you? I’m a resident that’s at the but of an investigation against me where I am possibly going to have to report to physician health services of Massachusetts’s. I didn’t do any of these allegations against me and I’m afraid that this is where they want me to go. I am not agreeing if they want me to but could I ask you a few things by email?
Email me via my website contact page. Sure.
Iam another person who was mandated to go to the WPHP, for patient satisisfaction scores that were not in the 90th percentile – which is the necessary number to get medicare advantage money.
I quit their “voluntary” (hint: it’s not) program when the witnessed urine screens provoked severe PTSD.
I almost killed myself; in fact, I am unsure how I am not dead.
I’m grateful for you speaking to me, Dr Wible, when I was so very lost and broken and alone.
Sent to the WPHP because your patient satisfaction scores were not 90th percentile? RETALIATORY REFERRALS that have destroyed the lives and livelihoods of so many. . . Physicians destroy each other and the infighting is so so sad to watch.
I’m so glad you didn’t follow through ?
Me too, Melissa!
If it walks like an organized crime syndicate and quacks like an organized crime syndicate, it may be an organized crime syndicate. If any healthcare professional would rate, on a scale of 1 to 100, the extent to which they WANT to believe that THEIR healthcare profession could NOT be under Racketeering Influence, what numbers do you think we’d see. If you are reading this and are a healthcare professional, how would you rate yourself on this scale? How do you think your peers would rate themselves. What do you think the basic descriptive stats on this would be? In the story here, bravely shared by Dr. Kelly, and in all the other stories so creepy in their similarities, we must ask, “Did these strange authority-figures walk like competent, trained, ethical, healthcare professionals? Did they quack like the same?” Each story of this type of domestic-terrorism shake-down I have heard, and I have heard plenty, something seems very wrong from the get-go.
My heart goes out to every victim of these medico-criminals. I become angry. It SHOULD NOT be that there are such elements among us but the plain fact is, there are. There is absolutely NOTHING that would exempt healthcare professions, entities, and institutions from being infiltrated by organized crime. WORK for a better system and a better world. If you try to WISH it into shape, your denial will simply exacerbate the problem and extend it for countless others to come. Sadly, tragically, denial = passive complicity. We HAVE been infiltrated by organized crime and we must call it what it is. May peace come to those who have suffered at the hands of criminals.
Christian,
Thanks for fighting for docs. What should we do to fight? I know we all want the courage to fight, but sometimes we don’t know where to start.
Where to start in my opinion:
1) Share your mental health story. Share your PHP story. Share your medical board story. When we are divided, we are conquered. The truth will set us free.
2) Love each other as brothers & sisters in medicine. When we have unity and we have each others’ backs we don’t have to worry about so many third parties swooping in to “save us” from each other and patients.
3) Get 100% nonpunitive and confidential health care. If we were all doing this we would not be drinking, doing drugs, or having mental health issues that escalate to the point of needing emergency treatment at a “preferred” center. Mental health care is not optional if you want to survive with your heart and soul intact within medicine.
Short of all that, I stand by the conclusions at the keynote I delivered to the Pennsylvania Medical Society/ Pennsylvania PHP. Read (and listen to it) here for more strategic advice for changing medical culture at the system level: Keynote: Physician Suicide—Prevention & Intervention
Right on, Pamela! Very well said. As A member of Rotary International, I subscribe to our motto which is “Service above self.” By NO means is this “service to the excusion of self,” or even “service BEFORE self.” I think most of us have heard the generalizable sage advice about oxygen masks in an airplane incident. The BEST thing you can do for others is to put your OWN oxygen mask on FIRST. You will not do anyone else any good if you, tourself are not well sustained.
To add to Pamela’s thoughts on where to start, I’d suggest JOINING others in a palpable and real-time alliance. Join HARBR-USA (you can google that and it should get you to our website at HARBR-USA.org. There, you will find the contact information for some of our brother and sister groups like Michael Langan’s Disrupted Physician, Kernan Manion’s (Center for Physician Rights), Linda Cheek’s Doctors of Courage, THIS site (Pamela’s), and more. Collectively, we will hope to see you become a part of us in this work we are doing.
Hi Kate – I am on board. Where can we start? Can we get others to stand together? Many docs are being unjustly destroyed. This husband describes it … Out there like a shack on a rock at the whim at whatever direction the wind was blowing. The wind is the breath of these unethical leaders who have absolute and unchecked power.
So many doctors are being ordered into PHP’s that are unnecessary and hideously expensive. Even innocent physicians are strongarmed, told that they have to undergo evaluations in facilities that all too frequently are not even accredited, or lose their licenses. It seems incredible that while everyone else has the right to choose a provider if they do have an issue, physicians who are bright and well educated are not allowed this option, this right.
The key is knowing how the PHPs are funded and what their relationship is like with the state medical board. Dr. Peter Yellowlees’ book is a source of explaining how PHPs are funded differently in each state.The MBC has even written articles about complaints coming from relatives or friends of physicians in competition with each other. Sadly, psychiatry and the physician-patient relationship has become a sociopolitical weapon. An interesting perspective or insights could potentially come from mental health criminal defense attorneys and what their standards are for evaluation.
Thanks EA! I didn’t know you were so full of wisdom on this topic.
The AMA at the behest of its HOD, over vigorous objection by representatives of FSPHP and ASAM, studied the sources of funding of PHPs back in 2010.
Although the page has been taken down by FSPHP, you can use WayBack machine (Web Archive) to find the source of funding for your state’s PHP as linked in the AMA 2010 CSAPH report.
Basically, entities originally designed to deal with substance abuse (and staffed by substance use or other types of low level counselors, sometimes “supervised” by physicians) have, with the blessing of the FSPHP and FSMB, expanded their potential cache of physician clients into all arenas of “potentially impairing” conditions affecting professionals. The AMA HOD has recently endorsed the concept, without any evidence that the AMA itself either knows the particulars or is studying the legality of methods by which PHPs do this.
Many of the policies promulgated by the FSPHP to its member PHPs (including WA) routinely violate the federal protections due to all citizens under the ADA. All WA physicians already fund their program via licensure surcharges (which are to be increased dramatically in 2020), and in addition pay for all mandated evaluations, out-of-state inpatient evaluations, and up to 5 years of witnessed drug monitoring out of pocket if they become PHP “enrollees”.
Those who most vociferously promote this “new paradigm” (RL DuPont, ASAM and FSPHP) do so by endlessly perverting a federal legal term, without any basis in law or precedent, that healthcare professionals occupy “safety-sensitive positions” and therefore require more intensive and prolonged surveillance, treatment and monitoring for potential substance use than normal citizens. These very same individuals have built fortunes from profits emanating from the requisite prolonged drug testing, and organizations too have profited in various ways by inducements from the inordinately restrictive and expensive drug treatment such “preferred” programs demand of physician patients, reportedly often without meeting criteria for bona fide substance use.
Average cost to individuals caught up in these programs has been documented by one of the perpetrators (RLD) to be in the range of $250-$320K (Judges Journal 2018;57(1, winter):1:32-35).
This is a VERY long term, well planned strategy for maximizing the extraction of profits (from ostensible “deep pocket” physician clients) using regulatory takeover and mission creep.
And it is killing some of us.
Thank you Louise and so many others on here who have truly dedicated so much time and energy to research and protect our vulnerable physicians from harm. I now understand that PHPs are going after medical trainees & med students too. Heard some terrible cases of suicide attempts of med students (without substance use) entrapped in these programs that have injured them, ended their medical careers before they even got started.
Money is certainly a big part of this situation. I assume boards get kick backs in some form. Otherwise, the PHPs are businesses. They want/need to make money to at least keep the lights on. They desire to grow. And like a private prison they have beds and programs to fill and most importantly a captive clientele without any constitutional or due process rights.
But there is something more beyond the above. You are dealing with psychopathic individuals at the hospital, board and PHP level. Folks that actually enjoy torturing you. They get off on the power to break you – but it’s for your own good according to them. From what I hear PHP programs operate like reeducation centers.You admit you are an addict even if you have never used drugs or alcohol
Anyone playing the game with the medical establishment using their rules and playing on their field is a fool. Defense will not work. Offensively attacking using the North Carolina Dental Board of Examiners v FTC SCOTUS decision of 2015 as a backstop to argue antitrust and constitutional violations by what are literally trade associations called boards.
drdovervsomb.weebly.com
harbr-usa.org
Can you share any central database of resources/actions related to PHPs?
Yes, I can. Here is a link to a Federation of State Physician Health Programs. This page lists Official PHP’s by state. In the News section at HARBR-USA.org, you can find a couple of PHP “investigative reports” I wrote. I’ve done Colorado PHP affiliate CPEP and I’ve done the twin Acumens located in Lawrence, Kansas. I have done Indiana but have not written the report up yet. Imagine though, that this is not just me, but dozen or scores or 100’s of us. These folks would start to feel the heat, and sadly, it seems as if FEAR is the only thing which these folks respond to besides the shiny coin. We are mere mortals, but it is NOT impossible to instill the fear of GOD in these fallen humans.
I also recommend reading some of our collective, excellent PHP activist authors such as Tom Horiagan, MD on LinkedIn, Louise Andrew, MD – also on LinkedIn, Anne Phelan-Adams (often on Medscape) just to name a few.
This is very scary. I am currently having ongoing issues with an NP who works under me. I cannot fire her as I work for a large hospital. They basically cannot fire her. I am afraid that I am going to soon lose My temper as she is already accusing me of acting unprofessional. What is my option? How can we prevent ourselves?
Sending you a private email with help. I know the perfect person who can strategize a quick resolution in your favor here.
Dear Dr. Wible,
I am a medical professional. At my hospital job I experienced appalling conditions where verbal and physical abuse of staff was a daily event. I also saw a lot of lateral violence among nurses in particular (I will never understand why women cannot stick together). My career ended prematurely a few years ago after I sought counseling and word went around that I was “cracking up” and couldn’t do the job anymore. Although I don’t regret seeking help (much), I can’t help but wonder if things would have ended differently if I had just developed an alcohol or drug problem like men in the fire service often do instead of crying in a peer counselor’s office (or if I had been a man). It was not a happy time in my life, but I kept working in the ER for a little while longer. Your articles and book had a lot to do with my decision to leave hospital based healthcare and look for other ways to practice. I knew what I was doing was breaking my body and my heart and it was time to stop and do my own thing. I don’t want to be sour grapes, but it still hurts when I run into guys I used to work with. Somehow they managed to salvage their careers in spite of disciplinary matters, injuries, family problems, trouble with the law, getting fat, blah, blah, blah….;) Thank you again for all your work and for giving healthcare professionals hope!
You are the third person I’ve been in touch with this week with the same complaint. Gender discrimination in physician health prgrams on top of everything else is the icing on the cake.
Anonymous Doc, please join us in vehemently eschewing the term “sour grapes.” My Oregon HARBR colleagues and I encountered this in an act that marked our founding. We issued complaints against several DoJ attorneys to the state bar association. We were very pleased with the fact that we must have leveraged enough power that all these attorneys “lawyered-up.” The first response from their attorney was a direct attack on the integrity of the 12 complainants. We were all painted as a bunch of “sour grapes.” We put a GRINDING halt to that notion. We don’t let people call us “sour grapes.”
When attorneys “lawyer up” now that’s exciting.
Those who are on the defensive from attacks by those who are exposing and trying to reform the system respond with “sour grapes” because they don’t want to admit that it’s actually “the fruit of the poisonous tree” that healthcare professionals are being coerced into partaking. T’is no wonder some are dying.
Please watch the follow up video A Plea to Anesthesiologists 2. I detail my struggles with addiction and recovery in a raw, nothing held back, brutally open and honest manner. If you know or suspect anyone struggling with a Substance Use Disorder please send them these links. It may save their life, their career and the life of a patient.
Jose Ramos MD
I LOVE YOUR VIDEO!! And your authenticity is LIFESAVING. Still have plans to help you help others. More to come. YOU are on my desktop and my next project and adventure. Keep the faith. YOU are AWESOME!
Physicians, follow Dr Wible’s advice. This is not the first story that I have heard. It’s unacceptable and denies you the right of access to caring clinicians.
Please share your story.
I will never get my license reactivated. The secretary at the PHP said she didn’t like my attitude and she had decided I was unfit and would never practice again. I was a victim of domestic violence. My then husband admitted he was a drug addict and cooperated. He is a practicing psychiatrist. He nearly killed me and our children. He belongs in prison. He was abusive to multiple patients in our shared practice. I refused to say I was a drug addict. I was forced to sign a false confession. I was told I could not tell the board what he did to me because they would assume I was making it up and would suspend my license. I am an excellent psychiatrist and would like to open a trauma recovery center. That will never happen.
OMG. Unreal. I’ll email you privately as I have some excellent resources for you! Never give up. ALSO I would love to know what you wish you would have done differently (hindsight is 2020) AND what do you recommend for others who are dealing with retaliatory/frivolous PHP referrals?
I had returned from a wonderful conference that I had designed and delivered for a regional public health department. I was so happy. I sat down in my office to answer my phone messages And had a message from the Dept head of substance abuse asking me to give him a call about my “impairment “. As someone who rarely drinks alcohol and never takes drugs I was shocked and initially thinking he dialed the wrong number. As I told him that I did not have a drug problem I realized that was what most addicted people say who are in denial about their problem and the Dept head clearly didn’t believe me. I contacted the Physician Wellness program who had referred me to rehab BUT they refused to give me any information about the referral initially. My approach when I have experienced an injustice is TO Make IT Public. So. In my anger and disbelief I talked to every possible person who had supervisory roles over me- the chiefs of both inpatient and outpatient medicine, my clinical station lead, the nursing supervisor and none of them said they had EVER had a complaint or concern for my “alleged”impairment. I talked to every colleague I’d ever worked with and asked then point blank if the had had concerns about my patient care AND told them what was happening. One of my fellow docs suggested I get a drug test which I did immediately. Finally the Physician Wellness chair who was also in my department shared with me that they had received an anonymous letter about me. They were not at liberty to share exactly what it said but it lead the committee to recommend treatment in our rehab department. When I spoke up about getting an attorney they dropped my getting help for impaired physicians. An anonymous letter lead me to the physician impairment program in my hospital. It took me 6 months to let go of the resentment and anger. I couldn’t look anyone that I worked in the eye as I would wonder , “Was it you?” Im convinced that this experience had the power to completely unravel me BUT I had personal and social mechanisms in place that protected me from going down the road of isolation and depression. In my heart I feel like Dr Kelly would be alive today if the process was not shrouded in mystery and she and her husband had been empowered to seek litigation
So having an attorney protected you and they dropped their investigation/evaluation? What would you suggest for others who are entrapped with frivolous or retaliatory referrals?
I believe making it PUBLIC was the key. Fighting back. Not accepting their plan. Being up for a negotiation. I also recognize I was in a special place in my career that made it easier for me to fight back I was mid career I had worked in this organization for 10+ years I had mini relationships with many people. I know it would’ve been harder if I were a medical student or resident or early in my career. I would recommend for anyone in a situation like mine or like Dr. Kelly’s to immediately bring allies into the conversation get different perspectives and most importantly don’t jump to comply with what is being asked of you take some time to think about the allegations and their long-term consequences. We have to support each other when situations like this occur at work
Aha! #1) DO NOT ISOLATE #2) MAKE IT PUBLIC #3) LEGAL SUPPORT. Don’t accept any abuse or predatory “help.” Real mental health care is non-punitive and confidential based on trust mot coercion.
I made my situation public as well and was directed to an external evaluation that showed I was fit for duty, did not habe a drug problem and that I should join the PHP for my safety. I now have that documentation. I don’t mind taking mo they drug tests and the PHP knows I have no drug issues so in my case it protected me. Mine was a report to the board that I was impaired with a drug I never took in my life. I’ve never heard from the board again and hopefully I never will but the whole situational almost gave me a nervous breakdown. I agree that going public and then having all those recommendations from people that know you helps. DO NOT ISOLATE!! GET AN ATTORNEY!!
Wow. How did your situation start? With a complaint?
Hey everyone, check TWITTER as the thread on this conversation going bonkers over on social media.
People take on the identity of their profession. This is their life. When you are accused and publicly defamed for something you did not do. It is devastating. The medical professionals who have not experienced this , have no idea what it really entails. You are looked at with shame. The boards/ agencies print a pile a lies just because someone who is retaliating said it. They know it is not true, and try to make you think you are crazy. Gaslighting is what they are doing , bullying as well. And who will people believe ? If its in print, and posted by an agency people (even the ones in the profession) believe it to be the truth , or they can sue them . (They have all the money and power to fight you, the judges are corrupt, the agency is corrupt. It is over whelming to lose it all what you have worked so hard for , just taken by nonsense, using mental health as a cover up ) Those doing this kind of “work ” will have a huge dark cloud over their heads . While the victim in all this is screaming why can’t people see it? What kind of country do I live in ? Is this America ? Why is this allowed to happen. While your colleagues are thinking all along , it won’t happen to them .
Many organizations blindly refer to PHPs for a range of issues (not just 12-step substance abuse)—communication/boundary issues, postpartum depression, test anxiety. One Program Director recently found herself trapped inside a PHP and boy did she regret sending so many residents there over the years. Now that she has had first-hand experience she is so apologetic to those who she referred. I know some people feel PHPs have helped them salvage their careers and that is fabulous. Others have lost their lives under PHP care and they deserve justice. Certainly their family deserves answers.
Required disclosures made during the ongoing procurement battle regarding Colorado PHP funding show that overwhelmingly the most common source of referrals to Colorado PHP in the last two years were founded on third party complaints. Public stakeholder spoken and written testimony about CPHP utilization show that organizations that employ physicians, very frequently residency programs were the majority of these “third parties”. The forced fitness for duty medical evaluations of employed persons, INCLUDING physicians is strictly constrained by ADA Title I. The Colorado PHP published a partial list of the contracts that it has with residency programs in the body of its sole source procured contract with the State of Colorado. CPHP, as a private organization, is not required to divulge these contracts. However, some of the signatories are state-funded residency programs that must disclose these contracts. A CORA request for one of these contracts was made last week and it is possible that the contract bound one of the parties into violating ADA. We’ll know soon.
It’s curious to me in reading these testimonials, that there is not a presumption of innocence, but of guilt, in these unjust cases. It makes me angry to hear of these injustices. I agree with Dr. Wible that the medical community needs to support one another, first and foremost. No one else is going to help to defend us. Unfortunately, we as medical professional are sometimes our worst enemies, envious and vindictive, rather than nurturing, empathetic, and supportive. Until our professional culture changes, these atrocities will simply continue.
We started out with noble humanitarian intentions and the process of medical education has pitted us against one another in a race for survival. Then the rampant human rights violations has caused (or exacerbated) mental health issues which we can now be punished for having. Please see Human Rights Violations in Medicine for details. Kind-hearted human beings who are not traumatized don’t behave this way. We have been placed in harm’s way through medical education and beyond. When we need help, we are often punished. Tragic.
This is a shocking story. So sorry for her family and friends about this unnecessary loss of life.
Hello Dr. Wibble,
Thank you for sharing the story of Dr. Shawn Kelley and others who have lost their lives in the health care profession. Having been a nurse for over 20 years and an NP for 5, I have seen the toll that it takes on health care providers. It is brutal! I also live in Washington State and suffer from severe burnout. I have had 4 jobs in the last 5 years. At my last job I was working 60-70 hours a week and getting paid for 32, and not well at that. I got the flu and was sick for 7 weeks and was only able to take 3 days off from work. I was so sick and exhausted and then the final blow, a needle stick injury. I realized at this point that the job was killing me, and I had to leave. I am now unemployed since May and pretty much unemployable in my area. I am trying to start my own business, but it is hard with no money. I feel like such a burden to my family. I wish I was dead, but don’t think I have it in me to end my life because I could never inflict that kind of pain on my family. I have worked all my life to relieve pain and suffering and love my family dearly. Instead, I suffer silently…under tens of thousands of dollars of student loan debt…with no way out. I am deathly afraid to get help, and you clearly understand why. And as far as I can tell, there is no real help out there for me anyway. I am even afraid to share here anonymously, because what is anonymous anymore anyway? I would love to participate in your programs, but, unfortunately, I can’t afford it. I do follow your blog and it does give me hope. Thank you for all that you do for doctors and other health care professionals in need. Blessings to you!
Happy to help you with your wounds. Please reach out & share more confidentially here: https://www.idealmedicalcare.org/contact/ (and then we can talk).
In Ontario, Canada, the Ontario Medical Association’s Physician Health Program seems like a mechanism that mainly allows hospitals and the accused to avoid the courts. It may also have some drivers that are well-intentioned (in addition to citing the service as addressing its members concerns or the desires of those the organization negotiates with), but there is much room for improvement if a priority is truly improving physician wellbeing and patient care.
The burden is largely on the physician once they enter into such a PHP contract in Ontario. Hospitals, licensing bodies (CPSO), and even mandatory CMPA dues-collecting agencies (and often OMA partners) provide little support towards the additional costs physicians can occur that limit their ability to care. This seems to force physicians down the rabbit hole of falling in line to act as an ill-equipped Band-Aider for a breaking healthcare system rather than work towards healing the wounds. The faster you can put them on without looking up or speaking out, the higher your quality of life according to your bank account.
In my humble opinion, upfront support would be more effective from a non-conflicted PHP. This may be especially helpful for the minority of physicians who come from lower socioeconomic backgrounds and/or enter medicine with the primary goal to heal, especially if a greater goal is to help provide health equity for all.
Prevent the hazardous working conditions and rampant human rights violations within medicine and very few people would ever be impaired or need help (especially if we had NON-punitive on-the-jog psychological support. Results of 7 years of research into 1,300 doctor suicides reveals some simple solutions: Human Rights Violations in Medicine: A-to-Z Action Guide. Prevention is key. Waiting to be the next victim is not a great strategy.
Why? This shit is so hard for me to read. I appreciate what you do greatly, but it’s scary how neglected physicians are currently. Thank you for taking your time to publicize and attempt to reduce stigma related to mental health. I admire you and your desire to confront that which others shy from regularly.
Classic cycle of abuse. Physicians have become victims–and playing that role for years with multiple third parties.
Thank you Professor Nethery for sharing your touching story about your wife Dr. Shawn Kelly’s suicide as a result of the abuses she endured by WPHP.
The abuses of the exclusively contracted PHP system and the complicit state medical boards which refuse to investigate their insider referral extortion racket must be exposed and confronted. At CPR – The Center for Physician Rights (www.physicianrights.net), we are actively educating and guiding physicians as they become wrongfully ensnared with these state-protected opportunistic predators in a veritable Kafkaesque nightmare
The pattern we’ve discerned in literally hundreds of cases is that the physician is wrongfully “referred” to the exclusively contracted PHP, usually by the MLB or by the physician’s hospital or group employer. Too often, an anonymous complaint initiates this gruesome cascade.
Claiming they’re benevolent programs for physician wellbeing, they newly diagnose the physician with a psychiatric condition and “recommend” that the physician be sent out of state at exorbitant cost to one of their “preferred programs.” Sadly, your wife’s story fits this reprehensible pattern.
If the physician declines the referral, he or she risks being reported to the MLB as being “non-complaint” and the MLB threatens to publicly revoke the physician’s license on the alleged right that it needs to protect public safety.
If the physician goes, chances are extremely high that the specialized “preferred 4 day program” will confirm the PHP’s referral diagnosis and “recommend” that the physician whom they’ve labeled as being in denial of their substance abuse illness be “enrolled” in a three month inpatient program. At the completion of this, the physician will now be placed on a monitoring program for five years, labeled as an “impaired physician.”
There is no escape from this nightmare apart from preemptively severing one’s medical identity prior to the MLB publicly and humiliatingly revoking one’s license declaring the physician “incapable of practicing with reasonable skill and safety by reason of mental illness.” There is no other word for this unconscionable behavior than torture.
Physicians and all concerned others must now demand of their medical societies and their state legislators and state executives a comprehensive, truly independent and transparent investigation of this corrupt movement, operating as it does as an extortion racket with the government’s tacit permission, doing so behind the seemingly impenetrable wall of sovereign and other immunities.
I would encourage all concerned – physicians, their families, their patients, their colleagues – to join with us in halting these abusive practices and holding wrongdoers accountable. You can sign up on CPR (www.physicianrights.net) to receive updates and be notified of emerging initiatives.
I would also welcome speaking with Professor Nethery about potential pathways he might pursue, especially as he is uniquely positioned to have his voice heard.
It’s so telling, Kernan, that despite so many (hundreds) of stories you have had, Chris bundy. While these are impressive outcomes by any measure, there remains a small minority of physicians who are not willing or able to effectively engage with their state physician health program (PHP). Such cases are often complicated and heart-breaking, resulting in a cascade of distressing personal and professional consequences that can irrevocably impact the physician, colleagues, patients and families. Under these circumstances, it
is not surprising that a few will become disgruntled, intent on unfairly disparaging PHPs and the PHP model. Their public protestations and allegations are shielded
Update! Vol. 9 Fall 2019
WPHP Report
from scrutiny by strict confidentiality protections that preclude PHPs from responding with facts that might prove illuminating. These one-sided stories can generate sympathetic support from well-intentioned, but often misguided, champions of perceived injustice who draw upon these anecdotes as evidence that PHPs mistreat physicians and that the PHP model is broken. This phenomenon is not new or unexpected given the nature of our work and, because most know otherwise, it has not appreciably tarnished WPHP’s reputation or weakened our stakeholders’ support.“
He is gaslighting harmed physicians at the same time he is celebrating the PHP reputation not being harmed (yet) or having stakeholders’ support weakened.
Who are said stakeholders?
We really do need to have this conversation. Seems that by investigating those who are injured by the PHP (or any program) data could be collected that would benefit and strengthen a program. The main issue here seems to be the secrecy (lack of transparency) that leads to such polarization. Why hide the truth? Why leave families wondering years later why their loved one died of hopelessness and despair under the care of a PHP?
I’m ever hopeful that justice and truth will prevail. Every life matters. Physicians and medical students deserve care, love, and support. By sharing our voices, our stories, our proposed solutions we can create a true safety net for physicians.
I also would love to know who the stakeholders are. Of course stakeholders used to be the ones to hold the stake driven through the heart of a suicide victim in the 1800s. May we now move out of the mental health dark ages. Punishing those who need psychological help is an antiquated and brutal way to treat a human being in 2019.
it is absolutely abhorrent that he minimizes the harm done to people under his eye – he states that the WPHP is not involved in medical care; doctors are ‘participants’ and not patients – trying to absolve himself and his program from harm done.
it’s not OK.
if you want to dictate care for people, order & interpret laboratory tests, dictate terms of medication use – you are a health care provider for them, end of story, and you should be responsible for outcomes. if this is not the case, then an MD license would not be necessary to oversee a PHP in any state.
Curious how you ended up in WPHP if you care to share publicly. If not for SUD I wonder why you are there.
it was for patient satisfaction scores (see above) not being 90th percentile or higher.
So effed up. Infuriating. Who’s idea was it to refer you? Are you in a large megaclinic?
no, i was but i left my job because of the unreasonable traumatic demands of the WPHP. i have an article forthcoming that describes the circumstances.
Thank you for being so vocal. Your are speaking for so many who fear repercussions. Grateful for your courage.
There is ABSOLUTELY NO QUESTION that PHP’s engage in medical inquiries under ADA Title I. This business about whether they practice medicine or provide treatment is a script from FSPHP and a complete red herring.
PHP’s are not in technical violation of the law. These programs completely ignore ADA. My opinions do not follow below. These are quotations from EEOC and USDOJ regulatory guidance.
According to the EEOC’s own published regulatory guidance: “A “medical examination” is a procedure or test that seeks information about an individual’s physical or mental impairments or health.” PHP’s perform fitness for duty evaluations on persons currently employed in and/or licensed in medical practice.
“Title I of the Americans with Disabilities Act of 1990 (the “ADA”)(1) limits an employer’s ability to make disability-related inquiries or require medical examinations at three stages: pre-offer, post-offer, and during employment.”
“At the third stage (after employment begins), an employer may make disability-related inquiries and require medical examinations only if they are job-related and consistent with business necessity.”
“Generally, a disability-related inquiry or medical examination of an employee may be “job-related and consistent with business necessity” when an employer “has a reasonable belief, based on objective evidence, that: (1) an employee’s ability to perform essential job functions will be impaired by a medical condition; or (2) an employee will pose a direct threat due to a medical condition.”
“An employer’s reasonable belief that an employee’s ability to perform essential job functions will be impaired by a medical condition or that s/he will pose a direct threat due to a medical condition must be based on objective evidence obtained, or reasonably available to the employer, prior to making a disability-related inquiry or requiring a medical examination. Such a belief requires an assessment of the employee and his/her position and cannot be based on general assumptions.”
“What action may an employer take if an employee fails to respond to a disability-related inquiry or fails to submit to a medical examination that is job-related and consistent with business necessity? The action the employer may take depends on its reason for making the disability-related inquiry or requiring a medical examination. Any discipline that the employer decides to impose should focus on the employee’s performance problems. Thus, the employer may discipline the employee for past and future performance problems in accordance with a uniformly applied policy.”
“May an employer require that an employee, who it reasonably believes will pose a direct threat, be examined by an appropriate health care professional of the employer’s choice? Yes. The determination that an employee poses a direct threat must be based on an individualized assessment of the employee’s present ability to safely perform the essential functions of the job. This assessment must be based on a reasonable medical judgment that relies on the most current medical knowledge and/or best objective evidence.(61) To meet this burden, an employer may want to have the employee examined by a health care professional of its choice who has expertise in the employee’s specific condition and can provide medical information that allows the employer to determine the effects of the condition on the employee’s ability to perform his/her job. Any medical examination, however, must be limited to determining whether the employee can perform his/her job without posing a direct threat, with or without reasonable accommodation. An employer also must pay all costs associated with the employee’s visit(s) to its health care professional.”
“An employer should be cautious about relying solely on the opinion of its own health care professional that an employee poses a direct threat where that opinion is contradicted by documentation from the employee’s own treating physician, who is knowledgeable about the employee’s medical condition and job functions, and/or other objective evidence.”
“May an employer require an employee to receive or change treatment for a disability to comply with a conduct standard?
No. Decisions about medication and treatment often involve many considerations beyond the employer’s expertise”
“Under current Commission regulations, an employer may justify action taken against an individual with a disability, including reducing work hours, where the individual poses a direct threat to the health or safety of himself or others. The term “direct threat” is defined as “[a] significant risk of substantial harm to health or safety of self or others that cannot be eliminated or reduced by reasonable accommodation.” 29 C.F.R. § 1630.2(r). A determination that a direct threat exists must be based on an individualized assessment of the employee’s present ability to perform the essential functions of the job safely, considering reasonable medical judgment that relies on the most current medical knowledge and/or the best available objective evidence. Id. Factors that must be considered include: (1) duration of the risk; (2) nature and severity of the potential harm; (3) likelihood the potential harm will occur; (4) imminence of the potential harm. Id. The availability of any “reasonable accommodation” that would reduce or eliminate the risk of harm must also be considered. See also EEOC Enforcement Guidance: Disability-Related Inquiries and Medical Examinations of Employees Under the Americans With Disabilities Act (July 27, 2000) (available on our website, and also discussing the “direct threat” standard).”
Medical boards do undermine physician mental health by breaching physician confidentiality and privacy. Discrimination against qualified, competent applicants who report mental health conditions is a violation of the Americans with Disabilities Act. In their search for criminal behavior among physicians, medical boards must not become criminal in their own behavior. By breaking federal law and the AMA Code of Ethics, boards have weaponized mental health diagnoses against physicians. Recommendations for all state boards:
1) Remove mental health questions from medical licensing applications. Replace with current impairment questions such as: “Do you currently have a condition that impairs your ability to practice medicine safely?” Comply with federal law by following best practices of Grade A states. Move criminal/predatory behavior queries to the criminal section alongside felonies and DUIs.
2) Address impairment from hazardous working conditions. Rather than focus on individual victims, engage in high-yield activities that resolve hazardous conditions impairing physicians en masse. To truly protect patients, align with all other industries invested in public safety that have legislated (and enforced) maximum 16-hour shifts, 60-hour work weeks, with minimum 30-minute breaks every 8 hours.
3) Encourage nonpunitive 100% confidential mental health care. Physicians require safe, accessible mental health care to be well-adjusted human beings. Most physicians enter medicine as humanitarians with noble intentions. Help them be well. After all, how can physicians give patients the care they’ve never received?
“Physicians are treated as criminals and tracked more closely than Level III sex offenders,” reports a general surgeon. “Answering all these questions on applications, the subtle, unspoken lesson is ‘you had better be squeaky clean, mentally, morally and physically! If you step off the shining path, bad things will occur.’ I have known 7 male physicians who died by suicide. Most with a ‘happy’ exterior. Why? They cannot confide in colleagues for fear that their colleagues will turn them in to hospitals and boards—and there goes their privileges and livelihood. They cannot confide in their spouses because during rough patches mentally, their marriages are already in trouble. If they share psychological problems, they probably fear that the wife may use this as ammunition in any future divorce. So they keep on smiling—right up to the hour they die.”
Even until their last breath, physicians retain their work ethic. Some doctors are completing chart notes, returning lab results, and checking in on hospitalized patients in the hours before their suicides.
By injuring physicians, we aren’t protecting the public.
Let’s end the physician mental health witch hunt.
Conclusion from Physician-Friendly States for Mental Health: A Review of Medical Boards
This hurts my heart to hear of this in a so called free and just society.
I feel I’m being abused and extorted by my PHP. I tried to get non-punitive and confidential care for my problems with alcohol, but my PCP talked me into going to the PHP. The PCP deceptively allayed my concerns about PHPs 00 0I0 felt desperate so, without doing any research, I went to the PHP for help with alcoholism. I’ve never regretted anything so much. They’ve been making jump through expensive hoop after expensive hoop.
Despite never testing positive on any of their multiple drug tests of multiple modalities and never having a single professionalism/behavioral/legal issue or complaint neither before nor after going to them, they’ve been escalating my “treatment” and taking more and more money from me. First they increased the cost and number of drug tests. Now, due to minor compliance issues (being under an hour late for their required twice-daily breathalyzer tests) a few times, the PHP is sending me out of state for a $5000-$7000 four-day evaluation which I will have to pay out-of-pocket with student loan money. Again, I’ve been required to use this breathalyzer twice a day for nearly a year and despite never testing positive for alcohol, the PHP is coercing me into spend all this money and go to Kansas under threat of getting kicked out of medical school. There is no meaningful consent for any of this. They have a tremendous amount of power over me and no oversight.
It feels as though this is a power-play by the director (who has no training in addiction medicine) who sees my minor infractions as deliberate insubordination and wants to punish me for that. Using medical treatment as punishment is not right, especially if it’s not even evidence-based, which these four-day evaluations are not! I don’t feel I’m being listened to by the PHP. The director has demonstrated on multiple occasions that they know little about my case. I feel depressed and defeated. I have no choice but to do whatever they say. If they require me to do an inpatient stay I will have no way to pay for it which means I’ll get kicked out medical school due to lack of compliance. Everything I’ve been working towards for the past 8 years will be destroyed leaving me nearly $200,000 in debt with nothing to show for it. I don’t know what I’d do then.
So upsetting. I will email you with some resources to help you. So so sorry.
I shadowed Dr. Kelley as a pre-med student and she was such an inspiring doctor and mentor for me!!! Such a bright ray of sunshine whose light was dimmed too soon? I was heart broken to hear about her suicide years ago. I’m so glad her loved ones have spoken up- the only way for the system to change is to acknowledge and address the problem!! Thank you for your continued hard work and efforts to expose and prevent physician suicide – mountainsbeyondmedicine on IG
Oh her family would I’m sure LOVE to hear from people who knew and loved Shawn and saw her in action with patients. Thank you!
Dear family of Dr. Kelly [cc to Dr. Wible]
So tragic, all my thoughts and prayers.
From the many posts, it sounds like WPHP has gone “rogue”
Perhaps a civil action in a court of law could at least send a message– and get WPHL to think twice
Five years ago I tried to kill myself with a massive overdose of tricyclic antidepressants. I was in a very bad marriage and really thought there was no other option for me then to kill myself. My then husband said he would ruin my life if I ever tried to leave him. Ironically I was the medical director of my practice and had a thriving and wonderful practice of medicine.
When I woke up after My failed suicide attempt and a week in the ICU I was sent to the psych ward for 72 hours and when that 72 hours was up I was sent to a 90 day rehab in Atlanta Georgia.
I don’t take or do any drugs I’ve never had any problems with the law, I never drank during the day only in the evenings. My only crime was clinical depression. My now ex-husband told them that I drink too much therefore the solution to my mental health problem was to send me away for 90 days rehab.
The first few days I was at rehab they made me call my state PHP to let them know I was in this 90 day program. the Rehab said it was mandatory I let the PHP know I was getting help. I have had to pay to be monitored these past five years. The cost, time, expense and shame over being a monitored physician is crushing. This has been embarrassing and frustrating.
I am treated by the PHP exactly the same as some other people in the program who diverted drugs had arrests for DWIs, going to work drunk or on drugs. I never did anything illegal the only thing I was guilty of was attempting to commit suicide. of note The fallout from being torn away from my family and sent to rehab for three months because I was clinically depressed -devastated and alienated me from my children, my friends, my patients, and my coworkers. it was like insult to injury. I have never felt such despair and hopelessness and the only way out was to follow their rules and submit to a program of random drug tests and mandatory AA meetings for the past five years.
I could go on and on. But having your medical license and the threat of being outed to the medical board hanging over your head was a new version of hell.
So basically, the lesson I learned is if you are horribly depressed And are in an abusive marriage don’t mess up trying to kill yourself or else you will be condemned to the PHP?
My only crime was clinical depression.
Says it all.
This is heartrending. In your case, the “stakeholder” (agency that held the stake to your heart after your suicide attempt) was whoever referred you to the inappropriate and uncalled for substance use Rehab program for your depression, and the PHP now holding you to the contract on threat of reporting to the MLB.
The abominable lesson from your case is clearly that if you are a suicidal physician you had best be sure that the method you use is effective. If you either ask for help (and it sounds as if you were already in treatment, to have been on tricyclics), or admit that the help is not working (e.g. overdose), you risk years of expensive abuse at the hands of these agencies, abuse that clearly drives some to suicide.
I hope that you are nearing the end of your sentence, and that you are VERY careful at this point with drug testing, insisting on witnessed duplicate specimens being sent only to bona fide, forensic labs; many have reported that non FDA approved, overly sensitive tests are being substituted for real forensic testing in some programs. Then when such non approved and overly sensitive, or even falsified, tests are reported to be positive, the entire cycle can begin again. It’s truly criminal abuse.
Our loving and supportive thoughts are with you. You did not deserve to be further abused by agencies pretending to advocate for you.
I remember a resident in a cardiothoracic surgery rotation who was sliced on the forearm with a scalpel by the lead physician every time the resident made a serious mistake or moved his surgical tools in the wrong manner. The CT surgery resident fellow had several scars on his forearms from the “discipline”. He pretended not to mind and often said it was the price he had to pay for his mistakes and to be a CT surgeon. It seemed like real life slavery and rape to me as a medical student. Needless to say I had seen enough of my future and became depressed and eventually changed careers. The senior CT surgeon was later fired from the hospital but apparently he had been using the same training process at other top Ivy League hospitals for years. Pam, your tweets bring back so many memories of the abuses I witnessed in my medical school years. I just had to share this story to let it out after holding it in for decades. Thank you for this space to share.
Amnesia can be protective. I think we all have similar tales to tell. Some buried very deep.
Reading about this really scares me. Is the purpose to destroy medical care in America? To subjugate medical professionals under the corporate health care owners until they are no better than a person who works any service job? I am hearing from more young people that they are deciding against college, against being in insurmountable debt, and this is sad. But I understand. I am considering dropping out of my masters program due to being warned about the corruption in my chosen mental health field. I don’t want to be blind sided one day by a phone call. It feels like we are now the United Mafia of America, everything must generate a profit or else. And if you dare speak up, your life is over…
After reading and listening to this statement it has occurred to me that the doctors who are expected to comply with the rules of confidentiality are not granted the same rights that they extend to their patients. Where then does a wounded healer turn when help is needed? Hopefully an answer will be found soon.
Doctors are supposed to be superhuman and they are held to superhuman standards in which they have their human right chronically violated. I have an entire chapter in the book Human Rights Violations in Medicine dedicated to confidentiality breaches.
Confidentiality Breach ~ When a medical student’s or physician’s sensitive and private information is intentionally disclosed or acquired by a third party such as an employer or medical institution that has power over the victim’s medical career.
Medical students and physicians develop high rates of occupationally induced anxiety, depression, PTSD, and suicidal ideation. Yet we’re offered no debriefing or on-the-job support after witnessing trauma and death. Instead we risk interrogation and punishment by medical boards, hospitals, and insurance companies when seeking mental health care. As physicians, we comply with laws protecting our patients’ medical information; however, our confidentiality is often breached by hospitals and medical boards when we receive care. As a result, doctors either don’t receive needed care or drive hundreds of miles out of town, use fake names, and pay cash for psychiatric treatment.
There is no way in hell I would ever try to get any type of mental health care under my own name. The PHP that I have seen collegues be forced into have been abusive and uncaring. They do not care about helping the physicians but only flexing their “power” over the physicians. I know one physician who has committed suicide over this after years of abuse and not being able to get her licensure resolved. She was one of the most talented surgical students I ever had the pleasure of working with but as she came under the care of the PHP, she became more and more dysfunctional and depressed. She complied with everything they asked of her but it didn’t make a difference in the long run. I also believe the medical boards in the various states have unchecked power to ruin a physician’s life unless they are independently wealthy to fight the medical boards as the medical boards have no one to account to.
Physician health program (PHP) related suicide typically occurs during a period of extreme crises that creates an overwhelming feeling of helplessness, hopelessness and defeat. The “Cry of Pain” model states that people are particularly prone to suicide when life events are interpreted as a “failed struggle.” Unable to identify an escape from a defeating situation, a sense of entrapment proliferates with the perception of no way out, and this is what triggers suicide.
In the 24 or so cases I am aware of almost all of the suicides were triggered by events that would most certainly be interpreted as a “failed struggle” and th perception of no way out.
More than half were triggered by the PHP reporting “non-compliance” to the medical board. If a PHP reports “non-compliance” to the medical board disciplinary (typically summary suspension) is an absolute certainty. There has never been a case of reported non-compliance that did not result in disciplinary action and this is common knowledge among those monitored by PHPs. The majority here killed themselves before any board action was taken and a few did so immediately after the board imposed disciplinary action
The PHP requesting a re-evaluation was the 2nd most common trigger found in 7 or so cases.
All of these suicides occurred during the final year of a 5-year contract and most requests for re-evaluation were due random urine screens positive for an alcohol biomarker. Re-evaluations must be done at one of the out-of-state “PHP-approved” assessment centers and it is common knowledge that the 4-day re-evauations (as with the initial evaluations) result in further “treatment” (typically 1-month inpatient treatment for “relapse prevention”) followed by a new 5-year monitoring contract. Nearing the end of their 5-year monitoring contracts these physicians would most certainly know what was in store for them and felt no way out of the situation and killed themselves.
The current PHP model constructed under the Federation of State Physician Health Programs (FSPHP) is toxic and it is irredeemable. The problem is not PHPs The problem is the extortion racket constructed by these charlatans they are calling PHPs. The FSPHP is a corrupt organization. PHPs are good organizations that have been corrupted by the FSPHP. This corruption needs to be recognized and addressed. The PHP model as it is needs to be bulldozed and rebuilt anew.
Thanks for your crystal clear analytical approach to this topic; thanks also to Pamela Wible MD who sheds light on situations such as these; condolences to the family of Dr. Shawn C. Kelley’s family, friends, colleagues and patients for her death is an untimely and great loss.
The association of “non-compliance” designations with physician suicides in PHP needs to examined in all PHP’s. It should alarm readers to know that the Colorado PHP, and the state agency that contracts with it, announced at a public meeting this past May that declarations of non-compliance were done with no reference to any standards or PHP process. The declarations were arbitrary.
The association of fatalities with these declarations adds to the weight of concern about PHP’s in the FSPHP model. It is already clear that CPHP and WPHP are state monopoly contractors and the population of persons that they serve are at least regarded as disabled or have a record of disability. Many of these persons may also have acute impairments.
The point is that persons with a disability under ADA are forced into a state contractor monopoly program that is completely free to treat them in an arbitrary manner without reference to any standards. This is a systematic civil rights violation that targets a group of persons with disabilities under the ADA.
And now, we have reason to suspect that these civil rights violations may be death-dealing. Corporate employers of physicians who send their employees to an FSPHP model organization retain liability for bad outcomes and civil rights violations.
The liability of individual medical board members for putting these abusive systems in place is a big enough topic to warrant its own discussion.
Reading this article reminds me – as though I need a reminder – that two of my colleagues committed suicide – one due to the virtual advertisement by the PHP of his mental health problems to the community, the other one out of fear of seeking help. I personally would have committed suicide had I not rejected the entire PHP paradigm. I knew it and I also was aware that I would be giving up a career for which I am well-suited and for which I spent years in training. Better not a doctor than dead.
In all, I had a terrible experience with the NY physician’s health program. I was sent there after reporting being raped by a fellow house officer. Medicine was my life and the hospital backed by the PHP put me on leave for depression. They just took away the most important thing in my life, and they wouldn’t let me back until ….. It felt like they were saying “we are going to put you underwater, and as soon as you learn to breath on your own under the water we will not let you have air”. When I moved to NJ they put me in touch with that PHP. I don’t know how many tens of thousands of dollars I spent trying to jump through their hoops. While I am licensed now, I have never been able to go back to what I loved.
In memory of Greg Miday on his birthday.
Greg Miday was to hospital medicine what Pablo Picasso was to painting, what Babe Ruth was to baseball, what Muhammad Ali was to boxing, what Lucille Ball was to comedy. Every once in a while a prodigy is born, someone so gifted they could practice their craft blindfolded. Greg breezed through med school. he spent much of his time helping his peers keep up. He was an amazing hospital doctor. He admitted the most number of patients in one night at Barnes Jewish Hospital in Saint Louis—ever. Years after his suicide so many patients are still overflowing with gratitude on his obituary page: “Dr Miday was not only a great doctor, but a great comfort to my husband and I when my husband was in Barnes hospital. Danny (my husband) coded twice and I thank God Dr Miday was there both times. The last time I will never forget as he gave me the sweetest look and said I am bringing him back. And he did, Danny was terminal, but because of Dr Miday we had 2 extra years with our husband, Dad and Papa. So sorry for your loss, to my family he was a genius and we loved him.”
Yet Greg was mistreated by his own profession for being human, for having anxiety (I bet most prodigies have anxiety because they are so far ahead of the rest of us), for drinking in his personal life. Bankers and realtors drink on their personal time without being policed and punished. Dr. Miday was never impaired at work. If you are ever in the ICU, Dr. Miday is the doctor you would BEG to have at your side. Yet none of us will ever have Greg Miday as our doctor. Why? He was punished by the medical board and physician health program for having HUMAN vulnerabilities in a profession that does not permit doctors to be human and have their constitutional human rights to life, liberty, and happiness respected. So at 29, Greg ended his life in a bathtub a few blocks from the hospital where he worked his ass off to save everyone else. WE LOVE YOU. <3 WE MISS YOU <3 WE WILL NEVER FORGET YOU.<3 HAPPY BIRTHDAY GREG MIDAY (11-13-82 — 6/22/12).
The Washington state medical board seems to have received federal funding. So, the applicability of the Rehabilitation Act, in addition to the ADA, seems apparent.
Great info. Thanks for sharing.
Some information shared with me from a medical board investigator:
1) Medical boards do have a hard time finding programs for doctors to participate in to satisfy state licensing statutes. It seems some states have more leeway than others. What may help in the struggle to get medical professionals help is to approach it through state legislative measures.
2) Some Board have a process allowing licensees to go to one of several approved programs (mainly outpatient) for monitoring and diversion based on settlement agreements. These programs are within the state so that the state can also monitor them and the professionals running those programs. Some licensees can go to out-of-state programs if warranted and upon request (Betty Ford Clinic etc.). Monthly reports are required from each program regarding every licensee in diversion so we can monitor the progress of the licensee as well as monitoring whether that particular program is helping that licensee. Goal is first to protect the public however, also always want to get the licensee the help they need whether it is diversion or prescribing or more training in their field.
3) From a Board’s perspective, there are a small few (more than you would think) who are always going in and out of diversion programs. Everything from patient abandonment to surgery nightmares can happen in these cases. We have doctors who literally leave patient records in garbage bags on the curb, refuse to get help and run off into the sunset. Contrary to what some might think…it is sad when we lose a physician to a ‘breakdown’ or ‘breakout’ of medicine. Many difficult decisions are made when these situations arise.
4) Boards do try and figure out new and, more importantly, meaningful ways to help licensees while still protecting the public. It is definitely a gentle balance.
5) Bottom line is….most Boards are willing to work with their licensees if they are honest about their situation. (It may be necessary in the future for physicians to determine where they practice based on the state Board!)
Thanks Pamela. I agree that medical boards may be in precarious situations these days and usually little is gained by demonizing them.
BUT, the levels of engagement of medical board physician members may be variable and sometimes is less than optimal. Physicians who serve on medical boards are usually gubernatorial appointees who may receive no or minimal compensation for their time and limited compensation for travel and lodging. Much of the work of the boards is actually conducted by permanent staff and board counsel. The latter are frequently junior assistant attorneys general with a focus on the “score”.
In some states, the medical boards may be likened to long-impaneled grand juries who are at once well-credentialed, over-subscribed, at utterly at the mercy of staff and counsel.
Add to this, the problem a party aggrieved with a medical board must overcome to deal with the common board defenses of ministerial vs. discretionary functions, policy-making vs. adjudicative functions, and claims of qualified and absolute immunity in the absence of active state supervision of medical boards in every US state. Aggrieved parties are always faced with the need to bring lawsuits against all board members in their official and individual capacities in the rare instances when lawsuits cannot be prevented with meaningful negotiation. It is understandable when board staff and counsel use tactics of bluster, intimidation, paperwork inundation, shaky due process, and the like in an effort to protect volunteer board members. The current legal environment inhibits a spectrum of reasonable responses and pushes counter-parties to undertake either full-fledged pitched legal battles or capitulation depending not on the merits of the case but rather on the resources available to the contestants.
Also, and this is definitely true in Washington State, it is not statute but administrative regulations that may “paint” a medical board “into a corner”. There are portions of the W.A.C. that did not come from the legislature and which simply seek to supersede the ADA and Rehabilitation Act. Those rules need to be struck down in court or modified before they face legal defeat.
I rather doubt the scenario of discipline diversion “frequent flyers” being a significant factor. Remember that there is a rapidly-emerging secular trend to physician employment and employed physicians comprise a plurality or majority of all physicians. Employment of physicians arose at the same rate as “disruptive physician” policies expanded. Disputes about conditions of work, abuse in educational programs, whistleblower concerns, staff rivalries, and the like can now all be taken to medical boards and PHP’s. In Colorado, the statistics disclosed during PHP procurement showed that the most common source of referrals to PHP’s were from third-parties, mostly residency programs and hospitals. The specter of labor disputes being “medicalized” by employers who are not prone to follow wage/hour laws, discrimination laws, and occupational health and safety laws should strike most people as chilling.
The idea that some physicians simply will be unable to practice in certain states is no longer true. It has not been true since the passage of HCQIA in 1986. Moreover, half of the states have joined the Interstate Medical Licensure Compact and must harmonize their licensing and regulation standards. If a medical board or a PHP violates a physician’s civil rights, then the answer is not by striking the right “balance”. A right is a right.
Medical boards have a duty to comply with federal law. Early attempts to use ADA against medical boards were largely defeated in state courts in the 1990’s but Congress was serious about ADA passage in 1990 and reinforced it with passage of ADAAA in 2008. ADA has a new lease on life and medical boards who ignore it do so at their own peril. The USDOJ has begun the process of challenging systemic ADA violations in occupational licensing and there is no reason to believe that this enforcement cycle has reached a crescendo. Any state law that requires treatment of a medical condition as a condition of medical licensure is in the wrong. There is NO list of essential medical fitness qualifications that can be applied to all categories of physicians. A medical board is free, and has always been free, to get assessments of whether an individual physician poses a direct threat to others based on a legally prescribed process of considering expert third party opinions. In doing so, contracting with a PHP “home team” does not allow a medical board to weigh one opinion on anything but its merits. Also, the FSPHP practice of only permitting “second opinions” from sources PHP’s approve of is now, and has been since 1990, blatantly illegal. Medical boards retain responsibility for their own compliance with ADA Title II and the Rehabilitation Act and may not outsource or delegate the duty of compliance to a PHP.
I would lay much of the blame on FSPHP. FSPHP has required full member PHP organizations to have a monopoly in each state according to data retrieved from the Internet Archives and as recent as 2015-2016. FSPHP clearly want their business model and perspectives to dominate medical board reasoning about physician impairment, the need to mandate physician health, and the need to address potential impairment. But, the boards are the organizations with ultimate responsibility and, in bitter contests, it will be the individual physician board members involved in lawsuits. It is primarily FSPHP dogma, rather than state statutes, that limit treatment options for physicians. (This assertion may be the MOST inaccurate of an array of incorrect or incomplete statements from this medical board investigator.)
State legislatures across the nation have kept medical boards in precarious positions since the 2015 SCOTUS decision in N.C. Dental Examiners v. FTC. Medical boards are no longer protected by the Parker immunity doctrine. That is a dangerous position to occupy when it is the core business of medical boards to engage in anti-competitive activity. Absent corrective state legislation, these boards are professional cartels that do not answer to voters. It is the board members who face liability when states do not place medical boards under the active state supervision that restores their Parker doctrine immunity. Not a single US state legislature has done this for a medical board.
It is noteworthy that the State of California did away with an official state PHP altogether. Discipline diversion did not limit legal contests in a state with an already “hot” and litigious relationship with its physicians and the medical board. California will simply be a harbinger of the status in other states if FSPHP abuses are allowed to continue and a more aware and militant cadre of physicians is willing to take them into legal battles.
A complete process for addressing “direct threats” posed by individual physicians has been available to medical boards since 1990. There are no consensus or universally-applicable essential medical qualifications for physicians. Medicine is not a “safety-sensitive” occupation under ADA. Drug abuse, or criminal drug diversion, has never been covered by ADA and neither have a variety of dangerous psychosexual disorders enumerated in statute. “Coerced” treatment of mental health or substance abuse disorders has turned out be be an idea that is nothing but a placebo in a healthcare environment that does not make such treatment readily-available, affordable, and free of stigma. We now see that mandatory, court-ordered drug treatment has done little more than create another category of incarceration that offers fewer rights to participants and indistinguishable outcomes compared to non-medical discipline. What started from a likely benign impulse, now approaches the Soviet-era abuses of psychiatry in actual practice.
PHP’s and medical boards are simply not the places to deal with unregulated enterprise liability in US corporate medicine and medical workplaces that afford physicians all the accountability and none of the control. PHP’s certainly have a role in modern US medicine. They can follow the successful, and ADA compliant, model of employee assistance programs. Never before have the work conditions of US medicine been so toxic or more likely to produce devastating adverse health outcomes for physicians. Such EAP’s have PLENTY of work to do. They simply cannot do it without confidentiality and a total lack of coercion. Medical boards still can exert a disciplinary influence but the notion that every one of their sanctions consists of a binary choice between coerced counter-productive medical treatment or a professional “death penalty” is just preposterous. A schedule of offenses and proportional sanctions seems like a good start. There are simply no data to support the assertion that the current state medical board disciplinary regimes measurably improve public safety.
State legislatures have long looked to the profession of medicine for an arena on which to impose “feel-good” symbolic statutes. State executive branches have grown used to “see no evil”, “take no responsibility” approach to medical regulation. I believe that this explains the nation-wide lack of enthusiasm to place medical boards under active state supervision. So, while individual physicians may serve as “liability sinks” and “fall guys” for corporate medical enterprises over which they exert no control, state executive branches apply a similar principle of leaving state medical boards to take all the accountability without the protective layer of active state supervision and the obligation to face the voting public.
In summary, the medical board investigator you cite may have some interesting anecdotes but he or she has no useful diagnoses or prescriptions.
You have amassed quite the knowledge base on this topic, Tom. Impressive! I myself (btw) almost applied for the open spot several years ago on the Oregon Medical Board. While inquiring as to my duties and responsibilities, I never heard back from the several people I attempted to make contact with. Odd. I took that as an indication that my services were not needed. I would love to work on behalf of vulnerable physicians for system-level change. Would love to feel that there is a receptivity to dialogue and engagement. Often it feels there is a lack of interest in listening to new viewpoints and unnecessary polarization between groups. I’m a community organizer at heart and my gift is bringing all sides together to resolve conflict and to create health care systems that work.
Pamela,
Your board has unfortunately long been known as one of the most repressive and unenlightened in the country. See documents how a self referred physician with an iatrogenic medication related manic episode has spent over a decade and spent hundreds of thousands of $s trying to maintain employment in the face of a board that equates low level mental illness with (non-existent) substance abuse. OR in fact follows the ADA inimical FSPHP model almost to a T. And also practices such racketeering and conspiratorial practices as using non FDA approved, overly sensitive alcohol testing (invented by FSPHP/ASAM stalwarts) to entrap those nearing the end of their abusive monitoring contracts with indefensible false positive results, designed to recycle the scheme against the unfortunate physician victim, thus increasing kickbacks and other profits from “preferred rehabs” and drug monitoring programs, from which the progenitors of this system directly benefit.
It is not at all surprising that the OR MLB rejected your application without even responding. I know someone else who applied there and was interviewed. This experience made it obvious that they are not looking for honesty or fresh approaches, but simply for others who will unquestioningly continue the status quo.
I suspect the same is true of many MLBs across the country. Their motto would seem to be “If it isn’t broken, don’t fix it!”. Problem, of course, is that it IS broken. Which is becoming more and more obvious as physicians come forward with their personal stories detailing how the PHP racket is perpetrated with the collusion of the MLBs.
It is going to take a major case, ideally one involving federal agencies involved in RICO, antitrust, and ADA, to forcibly bring the egregious practices to light and to end them. Let’s hope it happens before many more preventable physician suicides occur.
Such a terrible and tragic story. Practices such as this must not stand. Physicians stand in the gap for so many patients and it is at times incredibly stressful. For physicians who need help this will only serve as an example of why so many do not speak up and get help for fear of retribution. Unelected peer oversight boards must make changes so as not to be culpable in future tragedies given their unchecked unregulated power.
I am a UK EM physician. What a tragedy that this physician died, what a loss for her husband, her children, her family, her friends and her patients.
This video makes my blood run cold. The lack of transparency is horrifying.
A cowardly political power house hiding its failures out of fear. Where ever you live in the world, the right to independent, confidential medical treatment needs to be paramount. Without independent oversight this will continue. Professor Nethery is right, an Ombudsman is necessary, crucial.
I hope this comes to pass soon. I fear for all of us, where ever we are, if we do not have the right to independent review of ‘due process’.
All of us are human, physicians or not – we make mistakes, we fall out with friends & colleagues – of course we are accountable but so are those who regulate our practice. Time they set a good example of equity, transparency, trust and justice, free of corruption or bias. How can I trust my regulator or my doctor who fails to live up to the very values which informs all medical practice?
The saddest part is doctors by en large are overly honest and by disclosing in good faith their human vulnerabilities (occupationally induced anxiety, depression, PTSD, insomnia) they are publicly flogged and humiliated and risk losing their entire career.
I am another physician whose career was ruined by the Washington Physicians Health Program and the Washington Medical Commission. Here is my story:
Background
29 years in practice as a rural FP and rural ER physician. 25 years working in critical access medically underserved rural communities.
Board Certified AAFP for 29 years.
President of Okanogan County Medical Society 2001-2009. Served on Reference Committees and at the House of Delegates for both the WSMA and WAFP multiple times.
2001-2012 Rural Coordinator for the WAFP Family Medicine Exchange Program between Family Physicians in Washington State and Mexican FP’s in Veracruz Mexico. Very functional in Spanish and Medical Spanish. Made 4 trips to Veracruz and hosted Mexican FP residents in Omak, Tonasket and Brewster.
Medical consultant and weight management assessor for 4 different High School Wrestling Teams. Volunteered as part of the medical staff for the Washington State High School Wrestling Championships at the Tacoma Dome annually for 23 consecutive years. Chief Author of Pinning Down Skin Infections, Journal of Sports Medicine, December 1997.
1998-2018 Member of the Loup Loup Ski Patrol
Peace and Human Rights Activist for Palestinians and for Syrian Refugees. Between 1985-2016 I made 11 trips to Israel/Palestine and one trip to Greece, where I was the medical coordinator for 3 different NGOs serving Syrian war refugees. Author of over 50 related online articles. Editor and Co-Author of 2 related books, Freedom Sailors and Leaving Syria. As an ACLS instructor, I partnered with a cardiologist and taught an AHA certified course to Gaza physicians for the first time in the history of the Gaza Strip in 2016.
All this, until I was forced into early retirement.
Trajectory- A brief summary of a very long ordeal
February 2011- I was caught smoking marijuana while on call. I immediately enrolled with WPHP in good faith. I was sent to an inpatient program at Hazelden, in Newberg OR for 2 ½ months at a cost of about $65 K. There were no options offered by WPHP for treatment in Washington or for more affordable outpatient programs. I was told that by participating in the WPHP diversion program, the Washington Medical Commission would not intervene, as long as I was compliant with WPHP. This turned out to be false.
May 2011- I was finally released from Hazelden. I immediately received a notice from WMC informing me that I was being investigated and I wasn’t told why. I began “aftercare” with WPHP which required that I drive 180 miles round trip (4 hours) from Omak to Wenatchee weekly for 2 years and then bi-monthly for 3 additional years to attend one and a half hour 12-step type group meetings with a facilitator and other physicians from North Central Washington in the WPHP program. Additionally, I was subjected to 3 random urine drug tests per month for 5 years which included screening for alcohol metabolites. I was completely abstinent with negative tests for over 5 years. For each test, an observer watched me urinate into a cup, a humiliating experience. This “aftercare” cost me approximately an additional $35 K over 5 years.
September 2011- After 4 months, I finally found out what the WMC (MQAC) charges were about: some grandparents that I had never met had heard about the marijuana incident in February 2011 because of articles in local weekly newspapers, and raised concerns with WMC about care I had provided to two of their grandchildren in the summer of 2010 who were in a motor vehicle collision. In small rural communities, there is no privacy. This is one of many reasons why it is so difficult to recruit and retain physicians in rural areas. I reviewed the medical records: the care was completely appropriate, and the diagnoses and management were correct, outcomes were as expected. And it was completely unrelated to the Feb. 2011 marijuana incident. I wasn’t worried.
October 2011- I agreed to meet in person with an RN WMC investigator. By this time, I had been schooled in the 12 step program to practice “rigorous honesty,” i.e. self criticism and confession as a therapeutic tool. I was naive enough to actually believe in this. I met with this investigator. She seemed pleasant enough and I explained everything that had happened. I thought that this would be the end of it since I was abstinent and fully compliant with WPHP and thought I was covered by their diversion program. WRONG!
May 2012- Just as I had managed to resume working again as a rural ER physician after 15 months of unemployment related to the Feb. 11 marijuana incident, I received a letter from WMC asking me to sign a STID alleging “inadequate documentation” in the care of the 2 children during the summer of 2010. WMC had hired a board certified ER physician who worked in University based tertiary care centers, who made these allegations. This was “rural primary care bashing.” I was also to be placed on probation for the Feb. 11 MJ incident. This was not acceptable, since my privacy was supposed to be protected by being in the WPHP program. So I finally hired an attorney.
November 2013- After about $30 K in legal wrangling and attorney’s fees, and as I was stressing out 2 days before our scheduled hearing, WMC finally agreed to drop the bit about “inadequate documentation,” but the probation for 5 years until May 2016 would stay in place. My attorney felt that contesting this further in a full hearing would be a major gamble and would result in thousands of dollars more in expenses, and so I reluctantly settled. But this traumatised me even further. It’s like finding out that you have boarded the wrong train going in the wrong direction, but now you can’t get off the train.
November 2012-February 2014- WMC’s actions resulted in multiple additional news reports (at least 6 or more) in Okanogan County newspapers and radio stations about my February 2011 MJ incident over several years. This humiliated me and made it impossible to work anywhere close to the rural medically underserved community where I lived. And it was horrible for my wife and 2 daughters living in our small community who were also being ridiculed. This ultimately resulted in divorce from my wife after 32 years of marriage and estrangement by one of my 2 daughters.
Multiple Jeopardy- WMC reported me to the DEA in December 2012 after I had been abstinent for almost 2 years, and this resulted in about $8K of additional legal fees, and a year restriction in my ability to prescribe controlled substances: a real problem if you are a rural ER physician. This resulted in many more months of unemployment. Then my malpractice insurance company did not want to cover me, and we had to fight over that. Then the American Academy of Family Physicians threatened to withdraw my board certification and I had to struggle with them over that. Then years and years of “credentialing hell” which made it very difficult to obtain or maintain employment. I estimate that WMC’s actions in spite of my compliance with WPHP has resulted in over $400,000 in lost income.
June 2016- My 5 1/3rd year contract with WPHP and the probation with WMC finally ended.
2012-present, Chronic Pain- I had developed chronic pain over several years due to severe osteoarthritis of both ankles, the left ankle was compounded by a valgus deformity caused by a deltoid ligament tear from a 2012 ski injury. Tylenol and NSAID’s were not effective. By 2017, marijuana had been legal for 5 years and medical marijuana legal for over 10 years. I did not want to use opiates for chronic pain. Instead, I sought evaluation from a health care professional and obtained a medical marijuana certificate. I used marijuana sparingly, on my days off when I was skiing or working in my garden. It was quite effective and much safer than using opiates for chronic pain.
June 2017- I was seeing a patient in the ER who was complaining of RUQ pain. She had a history of IVDA and her family physician had already doubled the strength of her Hydrocodone/APAP the week before. She had an ultrasound scheduled for that very morning, but skipped that and came to the ER instead. I ordered tests, but refused to give her more opiates, as this appeared to be drug seeking behavior to me. She left the ER AMA before the tests could be completed. She apparently knew that I had been sanctioned based on the multiple media reports in Eastern WA during the years before. She made the false claim that I “smelled of marijuana.” If I had just given her opiates inappropriately, I could have avoided this predicament. Based on her complaints, the hospital I worked at required that I submit to a urine drug screen, which was positive for THC, and I was referred back to WPHP.
Fall 2017- Through my attorney, I offered to undergo an independent evaluation for chemical dependency by an expert here in the State of Washington. WPHP refused, insisting that I again undergo an out of state evaluation by one of their designated facilities. I was looking at another 5 years of crippling expense, so I refused. WPHP then reported me back to WMC. At my own expense, I underwent urine and hair drug tests every 3 months to demonstrate my renewed abstinence from THC, alcohol and other drugs. In an effort to try and mitigate my chronic pain, I went ahead and had a left ankle fusion which required 3 months of immobilization.
July 2018- I started a new job in Raymond WA, near Aberdeen, as a Family Physician at a Federally Qualified Health Center. The town of Raymond and this clinic had been without a full time Family Physician for over 2 years, ever since the WMC had revoked the license of the previous Family Physician. I was very happy to return to work and I was being well received by the clinic and local community.
August 21, 2018- WMC abruptly summarily suspended my license. I had an afternoon clinic full of patients, which all had to be abruptly cancelled. They had hired the same tertiary care center expert that had launched the “inadequate documentation” charges against me previously back in 2012, that were dropped after I spent $30 K in legal costs. This time, WMC spent a whole year, looking at all my records, and finally finding 4 old charts from 2-3 years before in a sham peer review process intended to destroy my livelihood and my career.
November-January 2018/19- While embroiled in legal limbo, I spent 9 weeks in Ecuador bettering myself. I did 9 weeks of immersion Spanish, including 2 weeks of Medical Spanish. I did this to improve my language skills. I did this to further serve the Hispanic populations that work the fisheries in the Raymond/South Bend area. The left ankle fusion that I had in 2017 resulted in a nonunion and more chronic pain. It affected my gait, which then resulted in a left quad tendon rupture. I had to come home to Washington to have it surgically repaired.
April 2019- Again I was crutch dependent and socially isolated in Raymond recovering from the Quad tendon surgery. WMC wanted me to spend another $6 K more to go to San Diego and undergo a multidisciplinary fitness for duty evaluation, which, more likely than not, would result in more sanctions, 5 more years of indentured servitude expense and more credentialing hell. At this point, I was having frequent bouts of suicidal ideation. At age 60, it just wasn’t worth killing myself, so I surrendered my medical license.
WMC/MQAC claim that they are “protecting the public.” But what they are really doing is imposing impossible expectations on doctors who are trying to provide service in critically underserved areas; in this case, denying the community of Raymond a full time family physician.
In summary, the combined actions of WPHP and WMC easily cost me more than half a million dollars in “treatment” costs and lost income due to stigmatization and unemployment, not to mention emotional trauma, destruction of my marriage and family life. We physicians carry malpractice insurance. But the costs of an investigation by WMC and treatment costs by WPHP can be crippling and much worse than a lawsuit. The coverage for these expenses can be haphazard and choppy. Some organizations cover these types of expenses, but most do not.
I have several docs on suicide registry who have been investigated similarly for using marijuana in their free time for occupationally-induced anxiety and insomnia (and in states where it is legal recreationally!). The current punitive mental health witch hunt on our doctors is leading to a loss of physicians (through unnecessary license suspension, early retirement, or the ultimate exodus through the highest suicide rate in any profession!). Med boards and PHPs are not helping the public when they punish and destroy the lives of good physicians.
I’m reading this again in 2023 and still horrified by your treatment by WPHP.
Can’t help but wonder why these programs continue to be referred to as PHPs – Physician HEALTH Programs – when they pose such a threat to one’s mental and emotional health, personal and professional well being?
Such a title does indeed appear to be a great misnomer and clever euphemism for concealing rampant abuse and injustice. I would propose that, under their current Modus Operandi, they ought much more realistically and accurately be referred to as PMPs, or Physician MONITORING Programs, for that is in fact what they are. For those who are ‘Participants’, the greatest threat to one’s overall ‘Health’ in most cases comes from these very same organizations.
And projecting forward, mindful and most appreciative of the growing conversation around these topics, and on a national level, I agree not only with the enormous need for reform and justice, but would propose that there be a complete overhaul and restructuring of the PHP model as it currently exists.
Perhaps we could look towards a national PSN – ‘Physician Support Network’ with regional / satellite centers where issues around workplace environment, personal issues and struggles could be dealt with in a truly professional, mutually supportive and comprehensive manner and without fear of reprisal or coercion.
Just a thought!
Agree that language can be utterly confusing. Yes concealing the truth in clever euphemisms. PHPs are more like monitoring programs and should be labeled as such. And don’t get me started on medicine’s favorite victim-blaming buzzword “burnout.” Now there’s a 40-year obfuscation of the truth: Physician “burnout: is a coverup for human rights violations in medicine. (explained in a quick 2-minute cartoon)
I’m not a doctor but I have had some very absurd and horrible experiences with the 12-step rehab scam which seems to have alarming control over the professions. After witnessing the ridiculously protected fraud that I fellow taxpayers end up paying dearly for, with no recourse, I started investigating the New York State social work system myself, and the result is notpowerless.com. There are definite patterns of fraud and abuse throughout this system and I’m always happy to hear others speak out about the scam, even though I know it means that they have trekked through hell to find out about it. There is no doubt in my mind that it is a criminal racket with blood on its hands.
Are you in New York now? I’m speaking this week in NY on the human rights violations in medicine leading to poor health of doctors——and patients. Would love to meet up with you! I’ll email you.
I had a similar scenario it has been an unbelievable strain on my reputation and career. I have managed to recover professionally by moving my academic practice to a different state but it is pain that is still felt on a daily bases. Others in a persons institution can use these PHP’s to take a person out by allegations that can never be verified and happen outside the hospital. It is a life changing experience that can not be easily rectified. I am sorry for those who are experiencing this process.
I find it equally sad and disconcerting to read the personal testimony of
Dr. William Dienst. A story with a different ending, but a ‘death’ nonetheless and seemingly premature end to a previously very meaningful career.
These tragedies remind me of yet another WPHP suicide that I heard about the summer before last in 2018. A woman in the Tri-Cities area of Washington State and a Plastic Surgeon who was fully involved with WPHP and ended up taking her own life. Got the distinct impression at the time that WPHP was ‘sweeping it under the rug and treating her tragic end in a very ‘hush hush’ sort of way.
What really stands out to me in all of this is that, collectively, we need to speak out more and more forcefully against the practices and abuses of the various PHPs. Historically speaking, meaningful reform has only ever come about when there have been major efforts at consciousness raising in the public sector. Think Civil Rights movement, etc., etc.
Can’t help but wonder why an interview such as Dr Nethery’s isn’t aired on King 5 News in Seattle, or the printed version published in the Seattle PI? And for the General Public to see how its ‘wounded healer’, physicians among us are so often treated behind ‘closed doors’.
There really needs to be a growing sense can of outrage and uncompromising outcry, and even the threat or reality of a ‘class action lawsuit(s)’, to bring about TRUE reform and justice!
I posted here a few days ago. Is my post rejected or lost or awaiting approval by the moderator, please?
since there was no reply to this, I will simply give up trying to post. richard
I loved Dr Kelly both me and my wife were her patients. Loved talking to her allows bright and gave her all to us. Miss her daily. I am heart broken for your loss. After reading this I am also mad as hell. I hope the kids are doing well.
What really concerns me is that for those of us, like Dr. Kelley, who have found ourselves ‘trapped’ in the PHP system, and by WPHP in particular, there is absolutely no way out under the current state of affairs. It’s truly a case of “our way or the highway” with the threat of loss of licensure always hanging over one’s head for any deviation from total compliance with what is basically a glorified ‘policing’ / monitoring program.
I say that without ever having had even the slightest complaint about my patient care. If anything, it was just the opposite! And yet with no due process, no oversight or third party supervision or critique of how how WPHP conducts its business, one is unarguably bound to a 5-year contract at $480 / month.
Have to wonder on what legal and legitimate basis, such a ‘contract’ can automatically be demanded of all ‘participants’, or else? In all honesty, have arrived at a place of being able to reclaim my own dignity and identity, but it took the best part of three years to get to that point.
It comes as no surprise that Dr Kelley herself would have experienced the potentially soul-searing effects of being bound by such a contract with WPHP. There are certainly many others who have experienced the same. And in my own case, I would have to say the initial assessment at WPHP headquarters in downtown Seattle was one of the worst, most disillusioning experiences of my life and subsequent interactions the greatest threat to ’emotional sobriety’. And all under the guise of being a ‘Physician HEALTH Program’.
I continue to see no way out on the practical, day to day level, until there are major changes on the LEGAL level. That’s just the reality! How and when that will come about is anyone’s guess. In the meantime, there are many of us who simply have to ‘play the game’ and forge forward the best we can. Not an easy task, but the ONLY way to preserve one’s license to practice and for the good of our local communities.
Wish things were otherwise, but that’s the harsh reality in the here and now!
First, my sincere condolences to Dr. Kelley’,s familiy However, unfortunately, Medicine is NOT the profession it once was, certainly not the profession that I became attracted to at age 5 years old.
I’m a 64 year old African American male OB/GYN physician, who grew up I The projects of St. Louis. Despite this I became a physician in 1983. My sole reason for going into medicine was to be of service especially to the underserved. I’ve NEVER let money factor into my practicing of medicine. With the exception of a year of Fellowship in Pelvic Surgery mall of my encounters with my patients have been in underserved areas. I trained at Harlem Hospital and workedin Community Health Centers primarily.
In 2009. I moved to the state of Mississippi and really felt appreciated. Unfortunately, in 2016, after the sudden death of my father and return to Mississippi I was reported by the Nursing staff at my hospital during a repeat cesarean section because of operating slower than normal, unsteady gait, and seemingly depressed. I was subjected to drug testing which was all NEGATIVE and had no history of illicit drug was referred to the Mississippi PHP, who referred me to Pine Grove Evaluation Center. The clinical psychologist asked about drug use and I told her that I was being treated for an anxiety disorder ( since 1998), and that my doctor had me on Lunesta PRN ,and had recently placed me on Ativan 1mg BID PRN. When asked about my work history I related two terminations, The first was 2 years prior to coming to Mississippi when a patient alleged that “chewing gum was placed in her vagina” during a chaperoned exam. I was terminated immediately by the physician employer but. I was investigated by the state who found the chaperone, and subsequently cleared with a letter stating such with no action against my license. Obviously when I applied to Mississippi for Licensure they knew about it and never even asked me about it.
The second termination was while working at the hospital at Fort Campbell as a civilian physician the reasons for which were baseless but one was a patient who complained that I performed an episiotomy on her even though she didn’t want me to and that she was still having pain from a vaginal sweep to remove retained placental tissue six weeks later. Again on my return to Mississippi I told the Board about this . They renewed my license and said it wasn’t a problem
As a result of this the psychologist diagnosed a mild substance use disorder and recommended an intensive outpatient treatment program and monitoring. Additionally, she labeled the two termination events as “Sexual boundary allegations “. I’ve been fighting with them since that these were never “Sexual “ in nature, but more importantly THE MISSISSIPPI LICENSURE BOARD KNEW ABOUT THESE IN 2003 and 2011, and had no problems. I told MPHP that I was not going to waste my money nor my time or the time of therapists going through the motions in a treatment program for a disorder that I know I didn’t have. Thier response was that I “was a good negotiator “, so they wouldn’t make me go through therapy but monitoring for five Years
There’s a lot more but that happened 2016, Since that time I was diagnosed with Parkinson’s syndrome ( which accounted for my gait and speech concerns).
Have not worked since August 2016.
Fell in my house, broke my hip and underwent surgery in June 2017.
Lost my car in September 2017.
Lost my house in December 2017.
I’ve been homeless since.
There is no reason that any governing body especially one charged with oversight and operating under the guise of “protecting physicians “ should not be responsible to a higher authority !,
No, this is NOT the profession that I was attracted to 59 years ago!
So fucked up. Really upsetting. Where are you now?
These stories are pretty appalling, and there are quite a few others published elsewhere. Considering the shame and resultant secrecy that PHP/MLB encounters and even moreso resultant suicides generate in physicians and their families, no doubt these reported cases are just the tip of the iceberg. Psychology Today has just published an essay by a former PHP Associate Director on the extortionate nature of the coordinated efforts duplicated in many PHPs throughout the country.
WA PHP seems to figure prominently in regular reports of abuse and suicides. The state received an “F” from this blog for the licensure application questions that appeared on the WMC site in August 2019
The WSMA considered a Resolution calling for more transparency in suicide statistics from WAPHP in October, but strong opposition was garnered by the PHP in favor of continuing the status quo, and as a result not much information has been forthcoming. Clearly it is easier to conceal the potential for abuse when there is little or no transparency, and also to continue it, when there is no meaningful oversight or supervision by anyone, least of all a compliant (if not complicit) medical board.
What IS becoming increasingly clear is that many of the routine actions of employers, MLBs and PHPs are being taken in contravention of the ADA. Published comments by prominent spokespersons for the FSPHP reveal that they are completely ignorant of the scope and protections of the ADA as related to their operations. Ironically, they actually view themselves as protecting doctors from discrimination, when it is indisputable to experts that they MLBs and PHPs are themselves prime agents of discrimination.
Unfortunately, the ADA is not self enforcing. Those who are discriminated against by being forced to pay for unwarranted medical examinations and unnecessary treatment will need to seek relief invoking the ADA via federal courts or the Dept of Justice or EEOC. Under certain circumstances, attorney fees and penalties are available, but injunctive relief is what is needed in most cases immediately. And virtually none of these is even possible without finding counsel that is knowledgeable and educated in ADA law, and not merely self designated “professional licensure defense counsel”. Many such lawyers are former counsel for boards, and they are not knowledgeable or aggressive in efforts to change the status quo by pursuing individual cases. After all, they can earn their fees by simply urging an enmeshed physician to simply “go along to get along”. When docs realize that they have been duped, they are often so far down the rabbit hole as to be unable to see a way out.
1) Why is it that one disgruntled individual in a social setting can leverage a complaint (unrelated to patient care) against a competent physician and undermine a doctor’s entire profession? Because in democratic societies there is “free speech”.
2) Why are two individuals with 10-month community college certificates in charge of determining the fate of a doctor’s career in 45 minutes? Because there is a lack of standards (training, competence testing etc.).
3) Why are physician health programs not using evidence-based medicine? These programs are only as good as the physicians working for the program.
4) Why is there a lack of transparency in physician health programs so that the physician and family and not given a diagnosis and treatment plan with a clear pathway to resolving the unsubstantiated allegations against the doctor? Sometimes there are confidentiality issues. At other times, there may be fear of an error being exposed.
5) Why are physician health programs unwilling to answer questions about physicians who have died by suicide under their care? Usually because of confidentiality issues.
I suggest it all starts with unregulated licensing boards. The intial complaint i am guessing went to the Medical Board who have the unregulated authority to send practitioners to the PHPs. Boards of medicine accept complaints as truthful, rely, on hearsay, deny mitigating circumstances and are permitted the latitude to enforce sanctions to attend a PHP, based on a complaint that had nothing to do with competency to practice.
It is these State Boards that need to be reigned in and made to adhere to a standard of clear and convincing evidence of a risk to the public. Texas Right to Know and American Association of Physicians and Surgeons has been working hard with members of the legislature to address these very issues that lead to denial of due process. They have had some success. The fight continues to create a licensing agency oversight Ombudsman.
I am deeply sorry for the injustice and cruelty your wife and you endured. This must stop. The evidence is replete that these PHP are rogue, for profit scams. Enough lives destroyed
Vince Nethery, thank you for sharing your story. I am making this post on idealmedicalcare.org to offer my answers to questions on the passing of your wife Dr. Shawn Kelley. Based on the information you provide and my own experience as a medical student involved with the Massachusetts “physician health program,” I have prepared the following response:
1) The medical director of the hospital could have leveraged the receipt of the complaint by deciding to apply hospital policies and procedures to a situation which sounds like started in a private setting unrelated to patient care. The question is why though? From my observation, hospitals and doctors are generally befuddled by public health issues having to do with prescription drug crisis, homelessness, hospital acquired infections, and rising incidence of preventable diseases; therefore, a complaint coming from within the hospital could mean opportunity for much desired “medical” work for the director.
2) Ten months of community college to receive a substance abuse training seems excessive. Who put such individuals in charge? It appears to be a group of doctors and administrators across universities, hospitals, and state licensing boards.
3) Some of the issues the Washington State PHP addresses may be subject to federal law according to Controlled Substances Act, for example. This means that researching something as important as medical students’ cannabis use, for example, may not receive research funding. I hear your concern for medicine not using evidence-based methods; however, the reality is that medical school starts with an oath to someone who lived thousands of years ago, Hippocrates. And, psychiatry has in the past hundred years substantially lowered the standards of providing evidence when making diagnosis as compared to most other specialties, in part because meeting with a psychiatrist is the single most important piece of evidence needed to make diagnosis of mental disorder.
4) I have this same question. The Massachusetts physician health program for example claims to be a “Medical Review Committee” according to Massachusetts General Laws chapter on public health (chapter 111, section 1); however, they should go in the chapter for top secret state affairs in my opinion.
5) A lack of response in such a situation could be interpreted in various ways, but let us respect people’s rights on self-incrimination, which the PHP may do (inadvertently or otherwise) if they tried to respond. While I understand your question gets to other suicides the PHP experiences, and even more generally to the crisis of physician suicide, I am still unclear on the question.
If there are ways I can help you get more answers or questions asked, then feel free to write back. I am providing my email in the comment form. When it comes to the question of what led to the suicide of your wife, I could not make even a guess based on the information available. And while I could not imagine what your family has gone through in the past six years as a result of your loss, I do hope my response here offers condolences.
I knew Dr Kelley, a horrendous tragedy. I am another WPHP participant who has found my involvement with them to be career ending.
I would love the opportunity to share my 10 year experience with them, and my continued struggle to get my license back. The money I have spent in this past decade has been enormous. Had an ER visit reecently with suicidal ideation. If I didn’t have the many supportive people in my life I would have been part of that statistic.
Can this be anonymous?
“Another WPHP Victim”
Please reach out to me, I will see if I can help with your situation.
I am a former commissioner of the Washington Medical Board, and Former Chair of the Commission, Retiring from clinical practice in 2016.
I am willing to help anyone as a navigator and physician advocate through the process at the Commission and WPHP. This is a free service and my way of giving back to the medical community.
I previously commented on the high number of suicides related to PHP reports of “non-compliance” to medical boards or request for re-evaluations and how the majority of these actions were precipitated by tests reported positive for alcohol biomarkers with most of these positive tests occurring during the last 6-months of the typical 5-year monitoring contract. As potential triggers for completing suicide this makes perfect sense as reported “non-compliance” always results in disciplinary action and a request for an “assessment” is never just an assessment and always results i treatment whether it is needed or not and in the overwhelming majority of cases it is not. These threats are real and the consequences significant and certain and this is when one would feel most helpless and hopeless with no way out.
The alcohol biomarkers used for PHP monitoring are not FDA-approved as they were introduced through the laboratory-developed test loophole.. The LDT pathway was designed for clinical tests and regulated under the Clinical Laboratory Improvement Act (CLIA). The LDT pathway was not designed for forensic tests but does not prohibit them by any law and this is the loophole that allowed Greg Skipper and NMS labs the ability to develop the EtG as a forensic LDT for non-clinical use. LDTs are regulated b the Clinical Laboratory Improvement Act which by definition only applies to labs used for clinical purposes the forensic LDTs are exempt meaning they have no oversight.
Greg Skipper and NMS labs introduced and promoted EtG as a forensic test that detected drinking if the test was above a cutoff level of 100 ng/m. This was quickly proved untrue resulting i a SAMHSA advisory cautioning against these tests and a Wall Street Journal article exposing its flaws. There is no known cutoff level that indicates drinking The EtS was introduced and promoted as a confirmation test for positive EtG but this was also proved untrue and there is no known cutoff value that indicates drinking.
A confirmatory blood test that” confirmed drinking” was introduced in 2013 with a cutoff level (> 20 ng/ml) drinking.
A year ago, I had a large 30 year practice, a decent retirement IRA and a few toys that I could entertain myself with over the weekends when I wasn’t on call.
I was sent to a PHP in Oregon at the behest of the Oregon Medical Board for inappropriate use and prescribing of tramadol. Yes. You read it right. Tramadol. At the time of my admission, my blood, urine, fingernails and hair were all negative for metabolites of tramadol. I have been on a regimen of UA’s, PEth tests, all negative for substance and alcohol use.
A year later, my practice is bankrupt. My retirement? Gone. My income? Gone. My earning potential for the future? Gone. But thats all material. the psychological and emotional costs? Incalculable.
Every group moderator and leader WITHOUT EXCEPTION, has voiced their opinion that the punishment inflicted by the Oregon Medical Board was not proportionate to the offense.
Hate to say it, but when you have everything taken from you under these conditions, suicide doesn’t seem like that bad an option. Criticize that if you like, but don’t judge until you’ve been in this situation.
I have a question. Could you email me. Thanks!
You can contact me any time via my contact page: https://www.idealmedicalcare.org/contact/
Hi I am currently in PHP?. My advice to anyone needing help is my God yes please get the help!!!! I got help for myself before I almost died from my addiction. My job is my joy as a Respiratory therapist which is being very quickly taken away from me from these awful people that put on there web sites honesty, trust, help, safe etc!!!! My God get help for yourselves unfortunately in disguise not letting anyone know your profession if possible or you will hurt yourself more. I would love to share my story from beginning to end but unfortunately my story begins tomorrow when I tell PHP enough and I’m going to fight back. What they are doing to me is destroying me mentally and physically!!! So my advice is AVOIDING PHP AT ALL COST!!!!! I pray for all of us to find and keep our natural happy spirits that no one can continue to take that from us when our joy in this world is to whole heartily help people. PHP WILL DESTROY YOU!!!!!! Sincerely Brenda
The biggest mistake I made was talking to the WPHP. I wish I could warn all medical professionals to avoid the WPHP. The physician health program will ruin your life.
I hope you will reach out for help. You have options. Promise. I’m here. Contact me: https://www.idealmedicalcare.org/contact/
I think that every physician that goes to a PHP meeting needs to bring an attorney with them every time. That’s your only protection, and is a way to start legal proceedings by havingan educated witness from the outset. If they object, start there by taking it to court under the bright lights of judicial inquiry.
The only mistake Dr. Kelley made was not killing herself at the WPHP offices so that her story would be front page news. It’s a crime what the WPHP did to her and to many other physicians. That organization prides themselves by proclaiming they “advocate” for physicians. Their “advocacy” seriously injures and kills many doctors. Physicians should be warned to avoid them at all costs.
I know of a doc in Florida hanged himself in front of the med board building and not sure that made the news. Let me check. Very public doctor suicide rarely make the news. I actually showed up and forced this one into the news (at the request of suffering/grieving colleagues). Yet this is rare: https://www.idealmedicalcare.org/suicided-doctor-covered-tarp-silence/
The latest WPHP contract has dropped the requirement for WPHP to track suicides and make a quarterly report to the Department of Health. It also explicitly endorses the use of abstinence-only diagnosis and treatment for SUD’s and any other condition in which it wishes to apply this pseudo-science approach.
WPHP has never made a quarterly report on suicides even when this was a contractual requirement. The DOH was asked to report the number of such cases and responded formally that they have no records on the subject.
Do you have a current WPHP suicide tally? The people who had responsibility for collecting these data completely shirked this responsibility.
The USDOJ has just ordered the Pennsylvania state courts to stop using abstinence-only approaches exclusively in its alternatives to discipline cases. Abstinence-only is not in line with current best evidence and is promoted by a cadre at ASAM.
I tried to get the Oregon Med Board to track physician suicides and twice they declined. Obvious place to track the active licensees who lapse due to death. No interest. I do have a list of doctor suicide cases that were involved with PHPs at the time of their deaths. Medical Boards exist to protect the public FROM doctors, not to protect or advocate for doctors. Sad reality. I am reading a book on the history of medical licensing and disciplining in America (note the emphasis on discipline/punishment).
US Justice Dept Puts Indiana Nursing Board on a Monitoring Program
Board and Its Professional Assistance Program (“ISNAP”) Told to Comply With Federal Law Within 7 Days … Or Else
The Indiana State Board of Nursing and its PHP equivalent, the curiously named “ISNAP” program, were informed rather straightforwardly by the US Department of Justice (DOJ) a little more than a month ago that they were in serious violation of the Americans with Disabilities Act (ADA). This determination applied as well to their exclusively contracted nurse professional assistance program (essentially a PHP type assessment, treatment and monitoring program) and all its service contractors in their nurse rehabilitation treatment complex.1
Think twice before joining a PHP. Some states follow the FSPHP guidelines like Georgia. Others make practicing in a State difficult. Most importantly gain help. Before you contact a PHP find our what you are getting into.
Been there. Done that. It’s a huge scam to suck the lives/souls/money out of physicians. I think the non-MDs in these programs find a life’s mission to destroy those who make them feel small.
The PHP has found a perfect pool of victims – doctors terrified of losing their licenses after investing dozens of years in medical education. It blows my mind how they’re literally run like a cartel. I spent a year battling the PHP, was forced into their contract to remain employed, and a few months later lost my residency (in large part because the insane biweekly drug tests made me impossible to include in an operating schedule. Note, I’ve never had a single positive test or diagnosed problem.)
It all brings me back to the Skype call I had with them “reviewing the PHP contract.” When reviewing one of the subsections, the PHP rep read out loud, “and what is your drug of choice?” I almost burst out laughing. It’s a kafkaesque nightmare. Wouldn’t wish it on my worst enemy.
I’d love to speak with you if you are willing. Please contact me here.