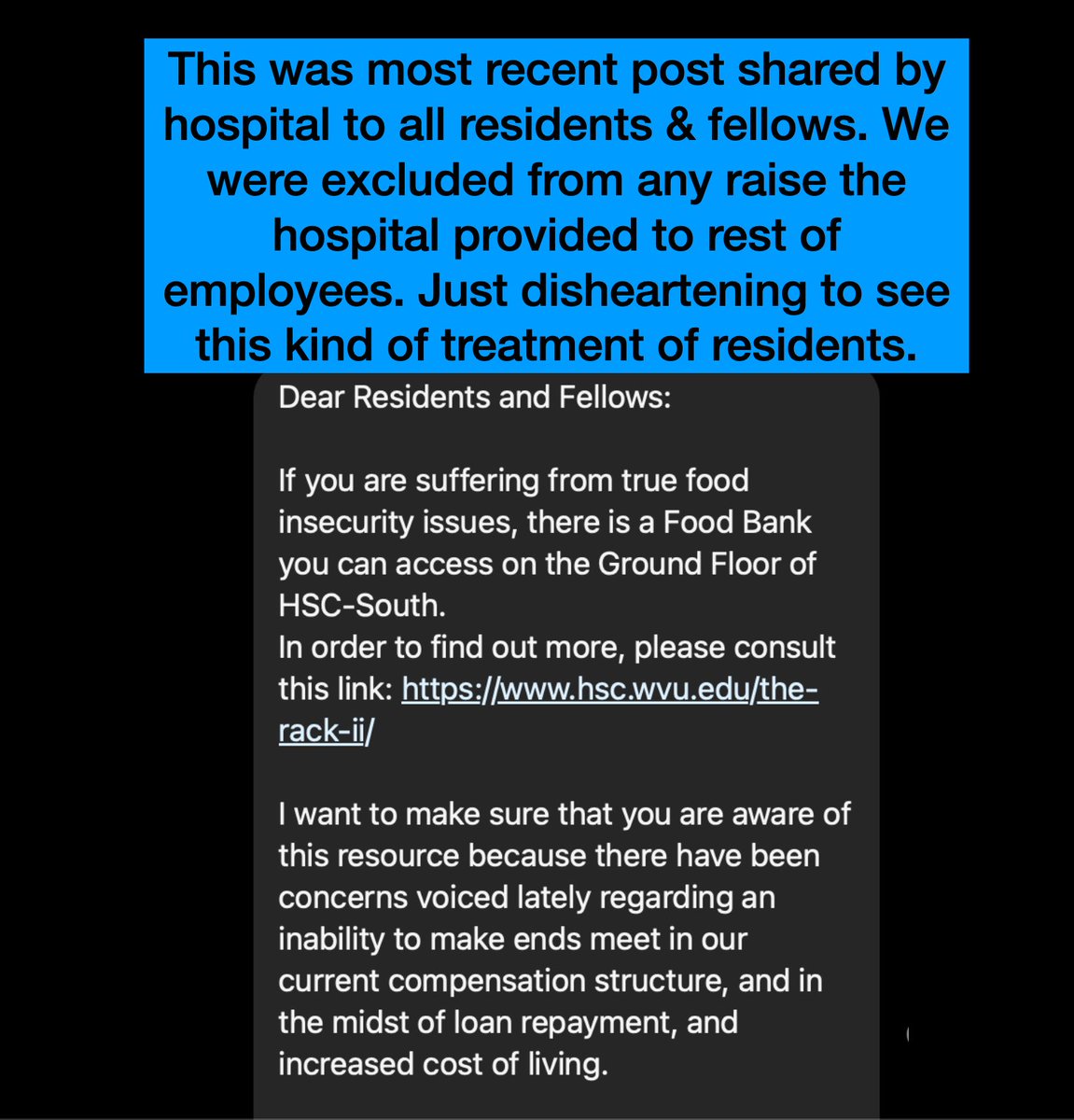
Just got this Instagram message (de-identified, posted with permission). A few comments:
“I calculated my own residency compensation as under 250 pennies per hour.”
“What the actual f***. Food bank??? Increase to a livable wage jeezz that’s embarrassing.”
“Average salary of residents and fellows is $60-80k depending on area and program. When working an 80+ hour work week it usually averages to less than $14 an hour. As a literal physician, my 16 year old brother makes more than I do at an Italian ice shop”
“I calculated for a friend recently that she started at 11 dollars per hour as an intern and is up to 15 per hour this year as a third year resident (min wage in her area is 16/hr so still below a livable wage for her in NYC area)”
“When I was a resident we had a meal card for food this is insane to work this hard and be hungry. They likely don’t even have time to visit a food bank.”
“Even residents in the military is making an actual income bc they are officers. This is insane.”
“The government gives them [hospitals] nearly 140k per resident to pay them 65 k this is bs.”
“I didn’t even finish clerkship because they expected us to work 55 hours per week in clinic while only receiving $10/DAY, and on top of that prepare for exams and ‘get a nanny.’”
“It’s not uncommon to see medical students and residents fainting from hypoglycemia and recovering on gurneys in the hallway.”
“Two times I fainted from hypoglycemia. The second time I hit my head on a stretcher on the way down and I was given juice by a kind nurse and then expected to keep seeing patients like nothing happened.”
“At my old residency, one resident went into diabetic ketoacidosis and required hospitalization for several days because of our irregular access to food and water.”
“Labor laws don’t apply to medical students, residents, or physicians. No bathroom breaks. No time for meals or snacks. Due to irregular access to food on shifts that exceed 24 hours, medical students and physicians, like most victims of starvation, develop pathologic behaviors around food including stealing apple juice and crackers from the nurses’ station or grabbing leftovers from patient trays.”
“I learned to eat fast. If you ever see someone eating fast they either served time in prison or medical residency!”
“Getting a break was sitting on the toilet doing your business while wolfing down anything!”
“The cafeteria closed at 1:00 pm so usually we’d miss breakfast because we’re on the wards at 7:00 am and breakfast is at 7:00. And then we’d often miss lunch because it is really hard to get off at 12:00 pm to go get something to eat,” reports a hospitalist on a multi-day shift. “And then the cafeteria was closed because it’s a small hospital so we’d have no access to food. And then I’d think, ‘Well, I’m gonna go out to get a Whataburger, (which I hate eating) and then I wouldn’t get out.’ When we’d ask, ‘Could we have access to food?’ Administration would respond, ‘Well, you outsiders, you come in and you tell us how you need to eat.’ It was insane.”
“I couldn’t afford to buy food at the hospital on an inpatient medicine rotation. I also was given no place to store anything so I would fill my pockets with dollar store granola bars and pray they kept my stomach from growling. One day I forgot them and got so hungry after a long day that I stole cold leftover rice from a meal for attendings in the physicians’ lounge. I was so afraid I would be caught and have to explain. I lost almost ten pounds off an already small frame during that one-month rotation.”
“Medical trainees lose significant weight due to lack of access to food. A close physician friend went from 130 down to 88 pounds during the first five months of her intern year.”
As a third-year medical student witnessing a surgery, I wasn’t doing anything too important other than holding a retractor with another classmate. Suddenly she collapsed onto the floor. She was out. Her blood sugar was 26.They checked my blood sugar. It was 24. I was still standing.”
* * *
Food deprivation is lack of access to food essential for normal function of the human body. The right to food is protected by Article 25 of the Universal Declaration of Human Rights. Medical professionals know well the impact of food deprivation on the human body. When our physiologic needs for caloric input are unmet, we struggle to function.
Labor laws guarantee that employees get bathroom breaks and regular meals during their shifts. At PetSmart, my dog groomer gets two 15-minute paid breaks and one 30-minute unpaid break during her 8-hour shift. At Starbucks, my barista gets two 10-minute paid breaks and one 30-minute unpaid break per 8-hour shift. Both work 40-hour work weeks. Even my pilot gets breaks and can’t fly more than nine hours straight. Yet new doctors-in-training work 28 (or more) hours per shift without breaks, meals, or sleep and are expected to work 80 (or more) hours per week.
Labor laws don’t apply to medical students, residents, or physicians.
Many doctors work for less than minimum wage.
Now they are being sent to food banks to eat.
Your thoughts?
Some excerpts above from Food Deprivation chapter in Human Rights Violations in Medicine (a survival guide for residents).














I believe every facility should offer free cafeteria food with a meal card to every resident due to the fact they are paid so little. This is the least the facility could do! Also cafeteria could stock breakroom fridge with health snacks!
Nurse break rooms also could be stocked!
Such a common sense solution (the least they can do when you work for them 80 hours/week)
I made $144k a year after taxes as a military resident, I was prior service which increased my salary, but compared to civilian residents, the contrast is insane. We had access to very cheap but nutritious food options. The fact that my civilian colleagues can’t be given living wages is an assault on medicine itself. Why does a PA fresh out of school get paid so much when they are easily seeing less volume and acuity? The whole thing doesn’t make sense. The hospital system that bucks this trend and fairly compensates the residents will reap the rewards. Don’t get me started on now actual physicians salaries have remained stagnant for 20 yrs.
The military versus civilian stats on salary and working conditions are really extremely informative. I’d also like to share a bit from a med student who wrote me: “I was less stressed in Afghanistan” – posted with permission.
Dear Pamela,
Let me start off by telling you that I am a warrior, a protector, and a healer. I am an Army Veteran. I’ve worked as an EMT, completed a bachelors degree and 2 years of medical school, plus I’m raising a family. I’ve achieved amazing things, but I have never been defeated like I’ve been over these past few years.
Honestly, I was less stressed in Afghanistan. Medical school is worse than my deployment experience.
It’s not easy to share this so bear with me. When I finished undergrad, I decided to be a doctor. So off I went. Completed my sciences at a local community college, volunteered at hospitals, and worked as an EMT to beef up my resume for med school applications. I got all my applications in then boom, I was deployed to Afghanistan. I was recruited to deploy with Military Police as a combat medic. During the first few missions I was scared for my life. After that, I became numb to that fear and just focused on making sure I was able to save my guys’ lives if we were attacked. The stress was incredible, but I had their back and they had mine. In an unsafe country and a future filled with uncertainty I felt secure because we supported each other.
Once I was home I started medical school and I was SO excited! I was finally living out my dream. I’ve always been able to make friends with no problem and I’ve always done well in school, so I was good to go. I am not the traditional medical student. I’m 30 with a family and it turns out my life is very different than my peers, so I isolated myself. The course material was incredibly difficult for me. I struggled. I barely passed some exams and always wondered if I would make it to the next course. I worked so hard to do well, but couldn’t hack it. I was just in awe at how much more intelligent everyone else around me was.
This was it, I had put all of my eggs in this basket and my basket was falling apart. I cried almost every single day. My family was there to support me but no one could understand what I was going through. Or so I thought. I never really opened up to other medical students because they seemed so smart and were doing well. It was bad. Here’s the worst part: I thought it would be easier to die than continue living like this. I started to see a therapist and we identified that I was persistently depressed and passively SUICIDAL.
I know I’m a strong, intelligent woman. But medical school broke me down.
* * *
The thing that gets me is that not only are you able to access food and a salary that help truly support you, but the camaraderie among military personnel is lifesaving (versus the competition in civilian medicine).
Nurse not physician but came to empathize after reading this. I remember being in a code in the ER with 8 patients. I’m a 260lb man. I started to cry in the middle of compressions saying that if someone didn’t take over I was going to mess my pants. Meals didn’t exist and going to the bathroom was a luxury. The abuse that comes with working in a hospital setting is universal and sad.
Thank you Luke. ER and OR nurses have very high rates of trauma exposure and likely not getting the support and debriefing necessary to maintain emotional health. Ugh . . . curious what it was about that person that made you cry. or maybe (like my husband) you cry more easily than most. A GOOD THING.I always felt in medical training that if I lost the ability to cry—THAT would be my death knell.
it doesn’t get any better once you are an attending. I did 2 years of 12hr night shift. I told my program director he needed to hire another physician because the work load was unsafe for 1 physician. I even told him I didn’t have time to eat yet alone use the bathroom. He told me to take the call-phone with me to the bathroom and to buy snack bars to eat on the go. What I learned was, unfortunately you cant look to make sure I have my basic needs met. I needed to learn how to say “I can’t right now Im eating, but i’m happy to do “x” after my lunch break” (this is excluding emergencies of course). Doctors are probably the least empathetic people I know. Needless to say I quit the night shift.
“Doctors are probably the least empathetic people I know.”
I think we start with some of the highest empathy among all——then meded and the culture of medicine (and the sheer vicarious trauma exposure) severs our connection with our hearts and souls.
Do you agree?
Well said
Dear Residents,
I feel you and I hear you–I empathize with you.
I have been there and I am there.
Seriously?
A food bank?
I have so many questions…
Why isn’t the pay and support for training physicians improving?
Is it open 24 hours a day?
Are there items there I/my family needs? Or do I waste my time and go down there to find out it’s closed or bare?
Do I have to come on my day off, which is super rare?
My other question–if there is a need for residents needing assistance, obviously no increase in pay AND a food bank why is the hospital not approaching the Food Bank and the volunteer staff to help the residents?
It’s inhumane, in general rude and an absolute slap in the face for those that go decades in school/training to serve others including the underserved and indigent populations without judgement. WHY? Because we took an Oath to do so? Yes. Because we took an Oath to do so and that means something (hold on and read).
As a resident 20 years ago, I made $37,000 a year and had bills twice that. One month I worked so much, I flat out forgot to pay my bills and everything was turned off.
My pay equalled $2.83 per hour (just before the hourly change requirements).
I ate crackers and peanut butter and sipped tomato soup from the Galley on a regular basis. The whole time I just kept thinking: This must be how it goes…this is part of your trial…to see if you can make it through the most intense, tough situations and hold it together. And, so I did.
After everything you have accomplished (which is A LOT…and don’t ever forget that) it’s truly disheartening to be guided to a food bank.
You deserve better.
I will also let you know: it doesn’t end at the food bank.
Before I write the following, please know I’m not certain I’ll practice medicine the way it was in my dreams starting in the second grade. Back then, I knew I was smart enough, objective enough and compassionate enough to be a physician. It’s a weird combination but it’s the combination that creates a great physician.
In 2020, as an established physician, female and a single mother of 3, without notice my medical practice came to a halt.
It was devastating at the time and the following 3 years have been and will remain so indefinitely.
That being said: stand together, don’t be afraid to say you need more support, don’t be afraid to come up with ideas. Don’t be afraid to put yourself before your Oath and walk away.
If needed exit medicine (hopefully gracefully) but DO NOT take the exit on yourself–somewhere in you is that trifecta: smarts, objectivity, compassion and…. a Doctorate Degree.
No one can take that from you.
Kelly – this is such a thoughtful and informative response. Thank you. I could not agree more with your concluding remark. I’d love to speak with you. We can do so much better.
“If needed exit medicine (hopefully gracefully) but DO NOT take the exit on yourself–somewhere in you is that trifecta: smarts, objectivity, compassion and…. a Doctorate Degree. No one can take that from you.”
Thank you Kelly, and to you (to your point of not know if you will practice medicine the way you dreamed in second grade) and all the residents, there is a better way to practice medicine. Please reach out to me to learn about our efforts to improve the lives of physicians at ViTel Health.
This is a travesty. While I did not suffer from food insecurity (my wife worked during residency and fellowship) this was a very real problem – even 30+ years ago.
Please remember that there are multiple levels to this problem – the residency program and their budget, as well as the hospital administration that is likely withholding money from the residency program. Again, we must seem to support administrators at the risk to the rest of the staff.
If anyone has a proposed solution (besides sending residents to the food bank), I’d love to hear it. 💕🙏
I was a senior resident when I had my first child. I did my residency in a city with a higher cost of living (how can you not, you don’t have much say so in the Match). Qualified for WIC and that’s how I fed my kid. Very few people know about this and I am sure my co-residents at the time were unaware. Went to the grocery store at odd hours or further away from the hospital so no one would recognize me. Between WIC and pizza coupons, that’s how my family ate during that last part of residency and prior to starting my first job. It was only later that I found out that other residents did similarly.
If we all compared notes we’d see our suffering is the norm. Sadly.
They can send billions to kill people overseas and fight proxy wars with taxpayers dollars and spend billions on illegal immigrants resettling but nothing for its own working class. Disgusting to say the least.
Publishing anonymous bc telling as it is , means getting “cancelled” these days.
💯 – though we must continue to share our truth. We cannot allow the fear and destruction to permanently dismantle our humanity.
I can understand the issue with food. My intern year I worked in Brooklyn my salary was $26,000 a year. I took home $714 every 2 weeks. I transferred to Univ of Miami for my 2nd year of surgical residency. In my 2nd year of residency at Miami, I was paid $20,500 for that year; my salary increased incrementally each year until my chief resident year, where I made $25,500. In my 2nd year of residency in Miami, even though my overall salary was much lower, I took home $714 every 2 weeks. New York city and state taxes were far more than Florida’s. Despite such low salaries, I paid off part of my undergraduate and some medical school debt (I had signed a Navy HPSP scholarship in my 2nd year of Medical School). In the early 1980’s HEAL loans (medical student loans) came with an 18% interest rate. And with the HEAL loans, you had to begin paying this debt back after your 3rd year of residency. Which meant that if your residency took longer than 3 years, you had to begin paying back at the beginning of your 4th year of residency- while you were still making nothing. I had fellow surgical residents who had to go to the bank to restructure their loans just to survive.
We just took it for granted that slave labor was the norm for residencies with the payoff being an attending’s salary when you finished.
And we did NOT have residency hour restrictions. I estimate that I worked on average about 120 hours a week. We worked 36 hours on, 12 hours off, 36 hours on, 12 hours off… I never stopped to calculate how much I was making per hour. In addition, my younger brother, who did not go to college was pulling down $60,000 a year working for Anheiser-Busch. I had taken a residency at the University of Miami in 1985 because I knew that if they allowed me to finish- at the very least I would be a competent surgeon. Knowing that I would be capable of tackling the vast majority of general surgery problems which would come my way after my residency is what drove me to continue this residency until I completed it. During my residency I had decided to quit a couple of dozen times- but at the end of the week or the end of a particularly challenging rotation. But at the end of the week or the rotation, the stresses lightened considerably- and I continued on. My chief resident year was like being a child in a candy store. I picked the cases I wanted to do, I supervised the residents and interns under me very competently. Life was a whole lot better as a chief resident- because I had suffered through countless trying situations, all the time increasing my knowledge, sometimes exponentially.
Now, I have worked with general surgeons who completed their residencies after 2010. And there are a frightening percentage who are “unfinished”. They cannot convert to an open cholecystectomy without another surgeon being present. Or they are stumped when they are faced with a challenging case- because during their residencies the attending surgeons always stepped in to take over the “tough” cases. And they never learned to think through the challenging cases- they want someone else to pick up the messy situations. Now I am old enough that I may need one of these people to operate upon me when I am in dire straits. Oh, Lord….
My salary “jumped” to $72,000 when I completed my residency- almost a tripling of my wages. I thought I was richer than Croesus with this salary (everything is relative, you know). Today residents are making more than what I did as an attending who finished a 5 year residency in surgery.
Of course, education costs have skyrocketed. Which is why I counseled my children to seriously consider undergraduate debt along with the other pluses and minuses of each university they applied to enter.
The downside of ensuring that costs of education for physicians are underwritten by institutions or the federal government is that you also sign away your future salaries as attending physicians. The day is coming when the head nurse of a hospital will make more than the staff neurosurgeon. Let us not help this happen any sooner than it has to. I was stationed in Spain from 1992-1995. Every single year about 98% of the Spanish physicians in the country went on “strike” each August. Because Spain had “socialized medicine”- the physicians’ salaries were capped around $60,000 a year, no matter your specialty. Plumbers and other tradesmen in Spain made more money than the physicians. We hired a Spanish female physician married to a Navy pilot stationed at Rota as our Occupational Health Physician. She was a fully trained, Spanish board certified ENT surgeon. The Occ Health position paid about what a primary care physician made working for the US Navy. I asked this lady why she took this job. Her answer: “It pays more than I would make as an ENT surgeon working in a Spanish hospital.”
Sacrifice has always been part of the scenario for physicians and their training. Sacrifice of time, of money, and of peace of mind.
I love what you are doing and I thank you for your efforts. These comments are made as part of the background for your conversation, not as detractions. There are many sides to consider with such a multifaceted subject.
Most Sincerely,
Philip Alford, MD FACS
P.S. As both an undergraduate and as a medical student, there were times when my money ran out. My parents were both lower-middle-class (that is generous) people with two other children at home. They had no additional money to give me. I borrowed from friends when the times were really tough. Survived on ramen noodles and cans of tuna fish for months at a time. I completely understand what it is like to try to study while you are hungry- and have never forgotten it. But my goals were worth the sacrifice in my estimation.
Just because its not as bad as when you trained is not a justification for inhumane treatment of residents. We are human beings who are expected to care for other humans and provide compassion in their darkest moments, and yet we are starving and being abused. This cannot stand in America anymore.
When I was a resident, my lunch or dinner was a single Glucerna or Pedisure/Ensure drink. It fit in my pocket (since we didn’t have a place to store them) and I literally had 30 seconds to finish my meal before working again.
Also, a friend ate peanut butter pocket (“Uncrustables”) for lunch for a whole year during fellowship because if you took more than 10 minutes lunch break it was frowned upon by the program.
There is absolutely no reason the hospital can not allow the cafeteria to be open and free to the residents and fellows. I’m private practice the hospitals feed the medical staff all day long. In addition, give these guys a raise as it’s not a good plan if you want some of f them to stay after training.
Agree. Bad decision just as a recruitment and retention tool for a clearly underserved area.
I recently found out that some of my vet students get food stamps. It is ridiculous and sad…
As a resident from 2009-2013 I was paid $36K per year after taxes. This is the money I had to live on. We received a card to access food in the hospital so that is where I ate all of my meals. I live in Sacramento, CA where cost of housing is about $2K for a one bedroom which left only $1K per month for everything else, including utilities, travel, etc..
I suffered from hypoglycemia and would often pass out during a long surgery. When I left my residency in 2013 due to health issues I never had another episode of hypoglycemia. The slavery and inhumane treatment of residents needs to end. There need to be alternate pathways to licensing for doctors who stand up to this treatment and have “Unintended attrition” that leaves them unable to become board certified.
After decades of “learned food insecurity” I’m STILL struggling to figure out how to feed myself properly … In my last fellowship, there were even rumors going around that I had an eating disorder because I was so thin … NO! I was just plain HUNGRY! Desperately so. Yet whenever I tried to eat (at reasonable times), I’d get accused of being “selfish” or “not a team player” … and even warned (politely) that I was at risk of losing my job if I couldn’t man up.
During my many years of training, I may not have had time or permission to eat as much as my body needed, but at least I got paid enough to buy food … So disheartening to hear some residents now aren’t even getting that! Thank you, Pamela for spreading the word! It truly is a serious problem, on so many levels. I think the general public really needs to hear about this … so many are completely unaware that doctors can struggle with food insecurity, too.
We were able to eat in the hospital as far as I remember. I did residency at Parkland in Dallas, and we worked hard but they took care of us. Residency and fellowship I will say I did work really hard but I never felt that they didn’t care about us. It was only when I got into being an attending when the work was endless that I really just got to where I didn’t like work anymore.
If they’re going into primary care, I hate to inform them that their situation won’t change. 40 patients a day, charting at home, taking call, no sleep, no time to eat lunch… it is now a way of life in health care. Although I’m a nurse practitioner, not a resident, the job experience is still the same where these issues are concerned. We are killing ourselves to take care of others. Some are killing themselves literally, the rest of us more slowly
“Regarding medical students + food stamps + food insecurity – I helped secure food stamps for medical students and other prof grad students (pharm, law, etc.) while at medical school (over 2000 plus people). I also ran an informal survey for food insecurity amongst medical students/professional graduate students (because at the time, there was like next to no research on medical students in particular and I needed something to show the politicians I was meeting that this was a real issue and not just a bunch of “privileged” students who didn’t know how to “tough it out”)
The rate of food insecurity, the stories of its impact, and the difficulty of securing food stamps when you’re a professional graduate student (e.g. medical student), as it stands right now in most states, is absurd. Food
accessibility is essential for students being able to take on academic programs, no matter if you’re in kindergarten or medical school. The idea that medical students, drowning in learning and diligently working to take care of patients, are not able to afford taking care of themselves – without applying to take on more debt – is outrageous.
There needs to be changes in how the law acknowledge medical students and how institutions support their students when designing their educational programs.
This issue is particularly urgent because we know it takes huge financial, social, etc capital to end up in medical school – which reflects studies finding that the majority of medical students come from privileged backgrounds. This means that for those from under resourced backgrounds who set their eyes on this challenge and make it all the way to medical school, accessibility of programs like food stamps (should students want to avail themselves to it) becomes all the more important for supporting their physician journeys. People deserve to study medicine while thriving, not stressing about starving.
This is insane. In residency we know intrinsically that we are being abused by the system, but you are so busy just trying to survive long enough to graduate, that you do not spend much time really evaluating how severely deprived you are forced to be. This needs to change. Is there and organization working on behalf of these residents to petition the ACGME to ensure that our future providers are paid a living wage? I propose we start one. Family and Friends Against Resident Exploitation. FFARE.
OSHA
What a sad situation. Where are our medical boards and medical associations? They only care when a patient reports a problem?
In the early ’70s my intern medicine program in San Francisco paid $11,000 the first year. Of course my apartment was $200 / month. Nevertheless, I could only support myself. Those who were married with or without children struggled. The spouse had to work full-time. Who took care of their infant child. Neighbors or nannies had to be paid. There was certainly no money for any luxuries from dinners out to vacations for married Interns. In my two years of Residency we were paid $14,OO0. One of my group of 12 committed suicide and two were hospitaized in the attached psychiatric facility. For reference we were ages 26 to 29. P. Golden, MD
I have experienced lack of food as a qualified OT with over 14 years work experience. Hence eventually gave up. I don’t treat any longer and struggle to go to the doctor. Allopathic medicine is a dreadful regime
As a former Program Admin for a family medicine resident training program, what you’ve shared here is a reprehensible situation. These trainees have enough stress with just covering shifts, continuing a high level of learning, and taking care of patients, and now they have to worry about whether to pay rent or eat? The direction of our medical system and its educational process saddens me.
I appreciate all that you do to support these people and to continue to bring the messages to us.
Looking forward to seeing you at our live session to discuss in more detail in about 30 minutes. TY for caring so deeply.
Yes, good ol’ Abraham Maslow’s Hierarchy of Human Needs pyramid
ensures that basic functions DO have to be met FIRST — food, shelter,
sleep — as the FOUNDATION for all the rest of the good work we can do!
Is it a question of >timeparenting< — her approach has
applications in ALL our relationships — employees, family members,
our partners, — and, OURSELVES.
I would wonder about having more docs absorb these kinds of messages
— so that, when they're training those who come behind us, they can
convey a more positive, supportive, realistic (healthy?) culture.
Best to you in your work, Dr Pam!
Now, back to the Friday To-Do list!