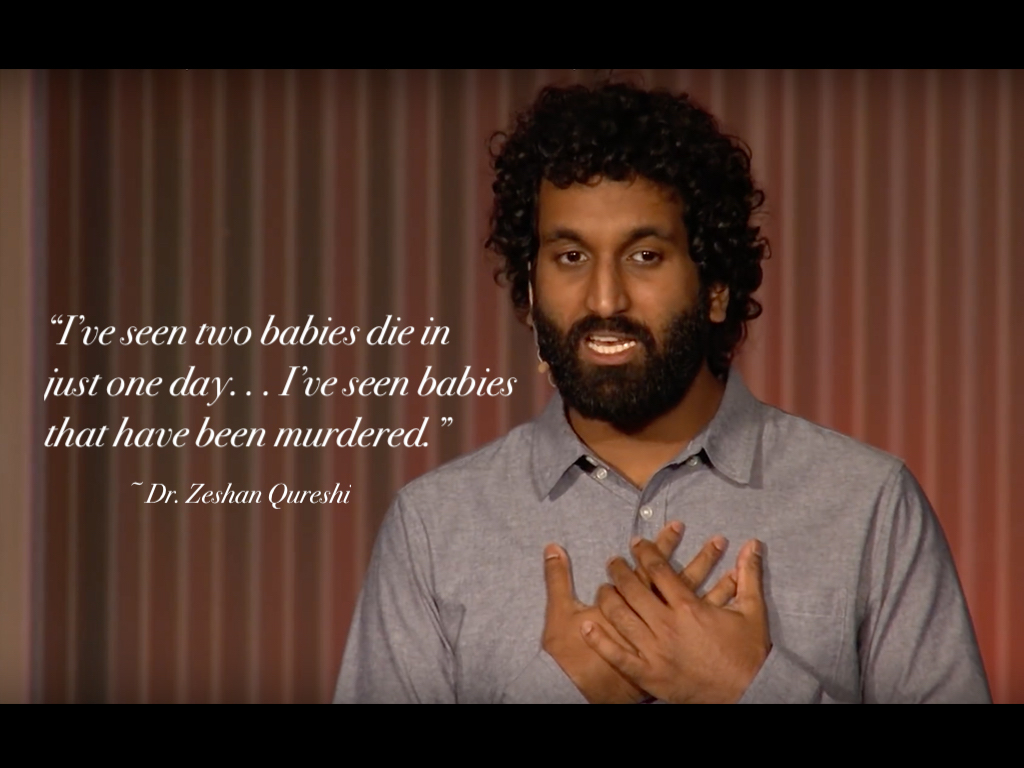
My friend, Dr. Zeshan Qureshi, just delivered this TEDx talk in New Zealand. Dr. Qureshi is a paediatrician in the UK with a lifesaving message for us all:
Our healthcare systems are making doctors mentally ill
I am a children’s doctor and I’m going to talk to you about the sick people I see. Not the patients, but my colleagues by my side. Tragically, I have attended the funeral of children that have died under my care. But equally tragically, I have attended the funerals of my colleagues—of doctors that were perfectly medically fit and well that took their lives by suicide. The rate of suicide amongst doctors is double that of the general population. America alone loses the equivalent of an entire medical school cohort a year to suicide. And that’s just the tip of the iceberg with depression, anxiety, post-traumatic stress disorder, burnout, drug and alcohol dependence all reaching near epidemic proportions.
We need to take urgent action because so much of this burden is entirely preventable. What are the solutions? Well some of them are so straightforward you don’t need to have been in hospital to be able to figure them out. You don’t need to be a doctor. First, we need enough doctors to do the job that’s asked of us.
My colleague—she was working a 72-hour shift. Horrific in of itself; you don’t really do that in most other industries. But on top of that, she was so overworked, so under-supported that in the whole 72 hours she only got six hours of rest. And not even a bed to sleep in, but a hard floor. You wouldn’t even treat a criminal like that.
But in the NHS where I work in the UK, I have never worked in a hospital that’s been fully staffed. We regularly come in early, leave late, skip our breaks, don’t eat, maybe not even drink. It’s absolutely exhausting, and it’s no surprise, given the fact that there are ten thousand doctors less than we want in the NHS. A hundred thousand less staff than we want in the NHS.
Burnout is inevitable and there’s a moral case for us hiring more staff to solve that problem. But if you don’t take that moral argument, there’s a strong economic case as well for the hospitals. I worked a really busy night shift in the Emergency Department and I was so exhausted by the end of it that when I went to sit in my car to drive home, I fell asleep. I wasn’t fit to drive a car. I wouldn’t have been fit to fly a plane or to drive a truck. Yet two hours previously, a little girl arrived in the Emergency Department not breathing and I had to make those decisions as to what we did to save her life.
Now how is that fair on me as a practitioner to be forced to make those decisions in a state of exhaustion? More importantly, that mother, she’s brought her child in at her time of crisis. She deserves and wants the best possible service and we’re not able to give it to them. And for the hospital, I don’t understand why it makes sense for them to make that kind of a risk when it comes to children’s lives.
Burnt out staff leads to increased costs, decreased productivity, decreased patient satisfaction and crucially decreased quality of care. So, it doesn’t make sense. What can we do about it? Well, start from the beginning. Medical school is consistently oversubscribed yet we artificially limit the number of places in medical schools. We need to liberalize that to account for the demand and staff in the future. The hospitals themselves—it’s simple, they need more staff and better working conditions. People working less hours, more flexible hours and then their needs being catered for on a day-to-day basis.
And then what do we do on those days when there’s a mismatch between the amount of work required and staff? Well, hospitals need to pay what it takes to get that emergency cover to help deal with the workload. And there needs to be a much lower threshold to cancel non-urgent work to allow doctors to work in safe conditions.
And what should we do as individual doctors when we’re in that situation, where there’s too much work to do, for our own wellbeing? We should be able to say ‘no’ and say ‘no’ much more readily. It’s difficult when you’ve got sick people around you, but the reality is, you’re sabotaging yourself and you’re harming yourself.
In London, over four years, there was a 160% increase in sick days taken by doctors and that is partly attributable to the fact that we’re pushing ourselves beyond our limit because we feel obliged to. We feel the sense of vocation to do so. But we have to look after ourselves in order to be productive in the long run.
However, this isn’t purely an issue of staffing and of working conditions. Medicine by its very nature involves facing human suffering and death at an intimate level where you feel a sense of responsibility for things when they go wrong. Thankfully, most people here will have never seen a baby die. I’ve seen two babies die in just one day. Now the families that have just gone through that tragedy—they’re not going back to work the next day, the next week, the next month—maybe not ever, and nobody would ask them to. But what about the staff, the staff that are there with the parents screaming, petrified as to what’s happening. It’s the staff that see that baby with that tiny glimpse of possible life doing everything they can to try and bring them back. The staff that go through that horrific process of saying, “I’m sorry we couldn’t save your child.”
After that shift, I had no space to grieve and to breathe. In fact, I went straight on to six further night shifts. For me, it was too much. I broke down. I couldn’t cope. And the burden that we experience is immense. I’ve seen babies that have been murdered. I’ve seen children that have been abused in manners that you wouldn’t want to imagine. There are difficult communication scenarios too. Imagine telling a child that they have cancer. You’d have to be close to a sociopath to be able to process all of those emotions without any degree of harm felt to you.
What are the solutions? Well, I’ve had some people say things to me like: “You just have to turn your emotions off at work.” They presented it as a choice between being human and being a doctor. For me, I am human, and I am a doctor. Both of those need to be preserved in my job.
There are lots and lots of things that can be done in the workplace to try and make it a better environment for dealing with these kinds of situations. One thing that is particularly important to me is the support of my colleagues, of people going through similar things around me on a day-to-day basis.
But in medicine nowadays, how well do we even know our colleagues? Take the cardiac arrest team. This is the team of staff that come together when a patient, or in my case, a child, is really sick. You would think that we trained together, we work together, we relax together, we debrief together. Well, what if I said to you that sometimes I’m meeting people from this team for the first time over that sick child. And then sometimes I don’t even see them again afterwards, with no space to process those lingering emotions and those doubts.
It’s difficult and it’s hard because even though we want to be able to debrief and that’s our gold standard, there often isn’t felt to be time and other clinical priorities take precedence. But even on a day-to-day basis, I spoke to a doctor the other day who had been working in a job for four months and his boss didn’t even know his name, let alone his struggles. And this leads to doctors suffering in isolation.
How do we solve this? Well, we need to prioritize bringing the team together. We need cross-disciplinary training and we need to prioritize debriefing in a meaningful way with the team involved and on the same day, even if it is busy because it’s so important for people being able to process what’s going on. But as I said with staffing, even if we do have the perfect team dynamics and other factors in hospital, the fact remains—we are dealing with a very emotionally intense job. And people will be in situations whereby they can’t process fully their emotions without the help of specialists: their friends and their colleagues and their own processing powers aren’t enough.
Medicine is an incredibly difficult place to do this. We are trained to be healers not sufferers. Imagine for me as a doctor; it’d be very hard for me to tell Dr Harris that I’ve got possible depression, because I went to medical school with him, or to tell Dr Fitzpatrick that I might have anxiety, who might be on an employment panel for me in the future. There’s so much stigma and people present late. How do I know? I have suffered myself. I probably could have got help a bit earlier than I did. That was a mistake. But I’m not the only person that has done that. And when it happens to doctor after doctor after doctor, then it’s not a problem with the individuals—it’s a problem with the system.
I’m very lucky—I had good people that helped me, I made a full recovery and I’m on the stage here speaking to you. But other people aren’t so lucky. They’re still sick or in a worst-case scenario in graveyards. So how do we address this? Things that are effective and that are increasingly being prioritized are sources of support that allow for anonymity and ease of access.
There’s lots of examples. I’ll give you two. One is a social media community called Tea & Empathy. 24 hours a day, seven days a week, you can access this, and thousands of doctors will support you, whatever your problem might be. Completely anonymously if you choose it to be that way. Or the practitioners’ health programme. This is again in the UK a service where you can anonymously and confidentially refer yourself to see specialists one-on-one for problems with mental health and addiction.
And this program was so in need that they had to close their doors for six weeks just to catch up on the backlog of people that needed help and support. However, there is still a huge unmet demand. If there was a drug that doubled the rate of suicide, it would be a scandal. It would be taken off the market immediately and an urgent intervention be put in place.
What do I think is needed? I believe that every doctor regardless of what their assessment of their mental health is should get routine psychological support for dealing with this traumatic world that we are working in. So that they don’t have to come forward while suffering to say we need help. And that truly will be able to bypass stigma because you’d have a safe, anonymous space to talk.
The Hippocratic oath was recently changed—the oath that we take when we graduate medical school—from purely talking about looking after patients to also looking after your health and your own wellbeing. But we have to go further.
We have to think about governments and hospitals being accountable. And if they don’t respond to the moral and the economic arguments, perhaps they should be held accountable through courts for how they treat their employees. One psychiatrist said to me that if the NHS was a coal mine, it would have been shut down years ago.
Perhaps we should treat doctors with that same respect. We are expecting extreme resilience in the context of a catastrophic emotional burden on top of working ridiculous hours from our doctors. We need healthy doctors to have healthy patients.
So, let’s improve the situation at work in terms of staffing and resourcing. But let’s also normalize psychological support and end this absurdity whereby hospitals are making doctors sick.
~ ~ ~
I’m thankful that physicians like Dr. Qureshi are speaking out against the injustice of medical training and practice that harms the very soul and psyche of our healers. Though I’m no fan of “physician burnout”—a victim-blaming term that identifies the doctor as the problem when clearly the healthcare systems sets our physicians up to fail. To end our doctor suicide epidemic, we must stop blaming doctors and eradicate human rights violations in medicine. Ensure doctors are protected by the same laws that protect all other citizens—labor laws that allow rest between shifts and guaranteed confidentiality when seeking mental health care. Doctors who receive routine mental health care are likely the healthiest most well-adjusted physicians. So let’s allow—even encourage—doctors to debrief after traumatic cases, to cry, grieve, and share their feelings—without fear of punishment. Don’t you agree?
Contact Dr. Qureshi here and/or leave your comments below.














I myself have been on a 80 hour shift and by the second day I didn’t hardly know who I was or even know what I was doing I was on automatic pilot. I understand what this man is saying and am thankful that we have Pamela Wible to show us what is really going on in the medical profession, a profession that we depend on for advice on health. Thank you Dr Qureshi and Dr. Wible for all your work. James M. Kenyon
What job were you in that expected you to work 80 hours in a row without sleep?
The high suicidality rate is a result of the fact that mainstream allopathy is disordered and fundamentally based on the exploitation (both financial and s-xual) of others inlcuding trusting children. It is also based on massive lies. Thus it makes sense that when the human soul fully embraces darkness (i.e autopsies and voyeurism on the vulnerable etc) that it should be tempted to suicide.
Working 80 hours a week has nothing to do with suicide. No one forces anyone to work 80 hours. They can go work as cleaners or in food service or other honest work. The allopaths who kill themselves also could not continue living with the hypocrisy of their lives and industry.
Dr. Qureshi’s TEDz talk answers one of my questions: Are the doctor suicide rates, and terrible working conditions, unique to the USA? It seems not, at least in the English speaking world. But how are they elsewhere, for example in continental Europe, and particularly in those nations which regularly lead the world in happiness?
I’d love to know true rates in all these countries.
Yes. I couldn’t agree more. Its imperative that governments stay out of our mental health. That is the key. We are not going to change the ineffective and illogical processes of governments backed by the bias and ignorance of human beings in charge of interpreting our rights. We must prevent governments from intruding upon mental health records.
I cant believe what they did to me. I had nothing to hide. But I was unaware of the shocking level of ignorance. Its unimaginable. You would not believe what they did to me. Its incredible. Its unbelievable. Its reminescent of something one could only imagine occurring in the middle ages or something. Like a witch hunt, junk science and a fear of “dangerous doctors”. The system of med boards combined with the state government is so embarrassing bc of the extreme levels of faulty “group thinking”..Its like group think on steroids…The intelligent voices are overpowered and ignored. The machine takes on a life of it’s own. Its embarrassing that human beings in this day and age could be so stupid and then continue to pretend that there is nothing wrong and no remedy is necessary. They took my life for no good reason. They took my soul and my identity and shred it into pieces. Then they pretend to have done nothing wrong and continue to pursue further harm against me. So…I will write my story and publish what they did and how they did it. It is the reason government should never intervene in the mental health of physicians. Physicians must work together to heal ourselves. How dare they rely upon physician expertise to healthemselves, yet when it comes to physicians own health, suddenly we are no longer to be trusted as experts? Blasphemy!
Medicine is a staid conservative profession of scrambling to avoid or to limit the down flow of detritus. Lying cheating manipulating any situation for personal immediate benefit is a norm. As young fellow prior to medical school, training and ‘practice’, I considered medicine to be noble, yet I was young ignorant and idealistic. No one going into medicine has clue as to stressors and abuses to come tumbling down in fits and volume. When on the Admissions Committee, my most important question was ‘what is your stress buster? how do you handle stress, pressures, incessant unrealistic demands?’ It is a war of attrition and so very draining emotionally. In that respect I was fortunate I was a runner every off-call day to bring me to the present after call ended. And the fault is in the system itself, and that is a lot of physicians perpetuating a flawed system on the edge. This requires a multi-faceted long-term fight for reform; any beginning anywhere is good. Talk is cheap and continues to babble over the past few decades plus. So who can will pick up the mantle and approach undergraduate and medical education programs? Here I can say Pamela Wible, MD and Zeshan Qureshi, MD are good starts who have been able to pull themselves out of the maelstrom of inner hell to address a large audience.
I think it requires quite a bit of resilience to graduate from any medical school. We all come from different backgrounds and had different advantages and disadvantages, but even the most advantaged students cannot graduate from medical school without the demonstration of attributes required for success. I think that those who are compassionate and healthy can only tolerate a certain level of abuse. I think that if we have to ask someone, who has accomplished medical school graduation, how one handles stress… it seems as if to imply that residency requires an abnormal kind of tolerance or adaptation that is beyond what is healthy. If we handle the rigors of medical school, we should be able to handle the rigors of residency. It should not require an abnormal suppression or adaptation to an abusive environment and I agree with you. I also think that those who do not respond negatively to this type of environment become immune and insensitive to patients. This is also not good from a legal perspective bc those who are unable to express empathy or communicate effectively with patients, family and other members of the health care team are more likely to be sued by patients. I think this concept is extremely underestimated. I think that state med boards and governments need to get their dirty hands out of our mental health. They have no idea what they are doing and how they harm the public by ignoring common sense. Its infuriating. Sometimes I wish I was simple and ignorant because then I would not have so much anger about the level of stupidity in our state institutions. I didn’t want to discover all of this. I devoted my life to learning about the human body and I ignored the signs around me. But now I see. I see a world filled with horror, abuse, human trafficking,false imprisonment,and people who go on about their lives thinking there is nothing that can be done. I was on the edge of discovery in my own field. My unique background had primed me for significant contributions to knowledge and discovery and after 20 years of progressive training and exoerience… I could see so many areas for discovery about how the body functions.. But just as I was about to apply my unique insight to reaearch and discovery…I was crushed by the California medical board. They took everything from me for no legitimate reason at all. I was forced to figure out what they did, how they did it and why they did it. I discovered an underground network represented by laws which circumvent due process and corruption which circumvents what little rights physicians are afforded. The whole system functions to benefit lawyers and in no way protects the public. It’s pretty alarming to know what I know. I see and I understand how suicide can become the only option in the mind. My love for my family keeps me here. I try to find others like me because this particular kind of trauma is unique to physicians and it is necessary to be able to connect with people who have experienced the same kind of trauma. Regular PTSD group therapy is not appropriate. The trauma I have is specifically caused by the medical board and the DOJ. This is litigation trauma on top of the ultimate career sabotage, a complete blocking and ending of my career, followed by severe and PURE public defamation of my character, honesty, intelligence and mental health. It’s hard to find someone else who has endured what I have endured. I almost wish I would have done something wrong because then the focus would be on my action and I could admit to wrongdoing and move on. However, I had not. When I say it’s pure defamation, it is truly pure defamation. There is no action or wrongdoing to support the accusations of incompetency. In fact, there is overwhelming evidence to the contrary. So….um….there is a big problem with medical boards and lawyers profiting off of this….and then there is the mental health of physicians industry..another money making scheme profiting off the suffering of physicians…falsifying high success rates by forcing doctors into programs who do not need them….
I totaled my Bimmer after finishing a seventh 12-hour consecutive night shift. I fell asleep and next thing I knew was awoken by the airbag. The accident was on the interstate, so I was driving over 60 mph, on my was home. This was not only a seventh consecutive shift. It was the seventh consecutive shift at a brand new job. I was hired and fast-tracked through credentialing and training to be able to get on the schedule ASAP, only to find my first 7 shifts would end in a horrible crash. Fortunately, no one was seriously injured…. the thing is, I went back to work and did not tell a soul. I felt it was my fault, I was responsible.