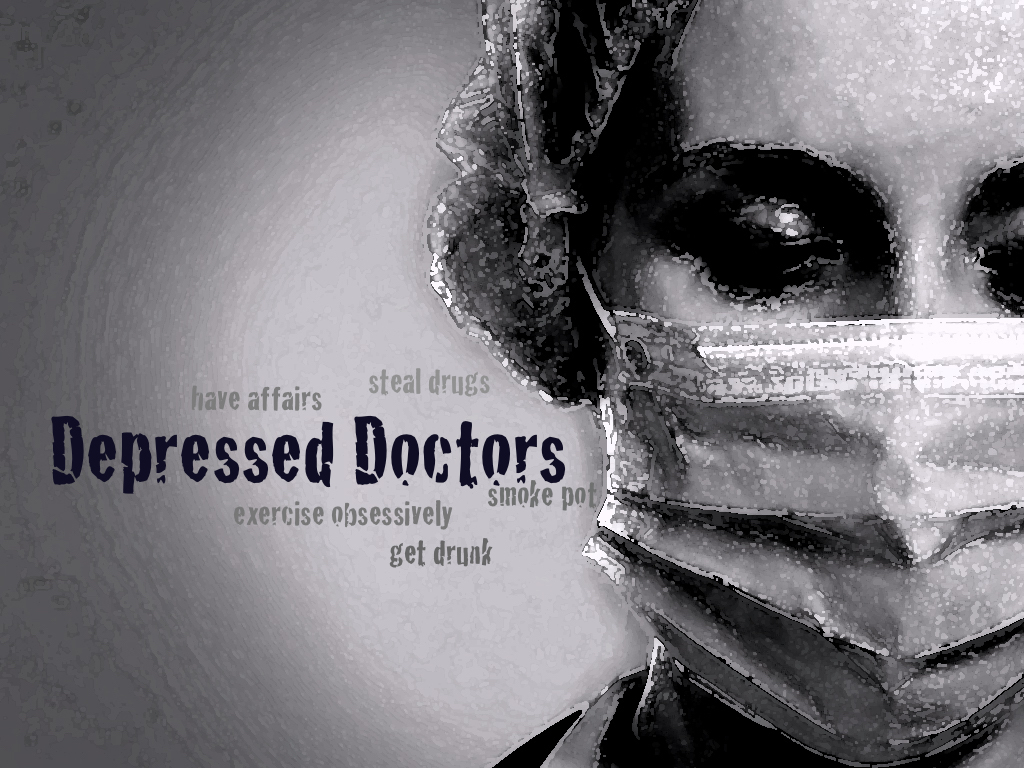
Do depressed doctors go to doctors? Do they even seek help? What do depressed doctors do when they’re not helping you? Doctors have affairs. They drink alcohol and smoke pot. They steal prescription medications. They binge-eat crap, scream, and exercise obsessively. Depressed doctors contemplate suicide. They hide their feelings to prevent being punished by licensing boards or mistreated by “Physician Health Programs.” Fact: depression is an occupational hazard in medicine. Chances are your own doctor may be depressed now.
Recently 220 physicians responded to my survey, “Have you ever been depressed as a physician?” Two hundred (90%) stated yes. Yet when asked what treatment they pursued only 33% chose professional help. Many just ignore their feelings or fall into self-destructive behaviors. In their own words, here’s what doctors disclosed to me (published with permission).
“Currently struggling immensely and realizing it is all due to the pressure of the assembly line I work in! Made worse by being made to feel like shit for standing up for what I believe in. It’s fascinating that wanting to care for patients, know them, love them, be thorough for them is viewed as incompetence! Anyway I digress. I abuse my son’s Adderall to try to be more efficient and survive on little sleep! Abuse 5 hour energy for the same reason! I self prescribe Cymbalta. I rescue too many pets trying to think that caring for them will help me. I drink to escape when I can on the weekends and I am not on call. I have tried an 8-week mindfulness based meditation class. Wow I could go on and on! Have to take my internal med board recert Monday and then make some major changes. Currently on an escalating path of self destruction. More than you wanted to know I am sure!!! Thanks for all you do! Trying to hang on! A few others I just feel like I need to confess to someone… Research how much of certain meds to kill myself, save up old Meds just in case, fantasize about getting a self-limited illness such as appendicitis so I can get some time away from the office to catch up … Sorry once started needed to get these off my chest as no one knows …I hide it so I am confessing to myself! Try to pretend like I am a good mom and a put together doctor! lol.” ~ Caroline
“I sought therapy while in med school….later on, meds and therapy. Honestly, I can’t remember how depressed I was in medical school and residency..let’s see…it’s such a blur!! I worked SO much, and was SO tired, (this was in the 1980s, and I am a woman) We were treated like dirt, male docs were always making sexual remarks, and making comments about us. Had an affair (he was married) with an ER doc when I was a 3rd or 4th year medical student (I guess that’s a form of therapy, yea, right)…. In residency, I worked such long hours….and despite being married (to another MD), I had another affair (again, treating depression??)…changed programs, got a divorce,….. Making me look back, it’s a wonder I made it!! Geez, such poor choices..was it youth or depression?? You are free to use this information…maybe it will help others. When depressed, we find lots of way to get through day to day…and they AIN’T ALL HEALTHY!” ~ Victoria
“I was told by the psychologist at my med school’s campus assistance program, that 75% of the class of 175 people were on anti-depressants. He wasn’t joking. How broken is the system, that doctors have to be pushed into illness in order to be trained to do their job? And then we wonder why so many of us get detached—detached from patients, family, but most importantly, ourselves. I am a psychiatrist. It is only through my personal work on myself that I have been able to stay in my own reality, observing compassion for myself, and then bring that compassion and reality to my patients. That’s what I should have been taught by my mentors in school. That’s what we all should have been taught. Because what is a doctor but the ultimate public servant? We are tasked with caring for others as a profession. How can we possibly achieve that when our own beginning in the work, is characterized by detachment, dissociation, and despair? I’m passionate about medical education. Whatever I can do to help, please do let me know.” ~ Jaya
“During residency took med prescribed by family doc. In practice took meds from sample closet (Celexa, Lexapro), self medicated with food, Binge eating disorder. I see my family doc now and a psychologist (self pay). I use Seasonal Affective Disorder as the reason for my med now and not depression although I am not afraid of medical boards anymore. I also see psychologist self pay so that it is not in my chart.” ~ Laura
“I experienced PTSD, complicated grief and am leaving medicine. I abused alcohol for awhile, sought help (am now alcohol free 2 months!) and have had a negative experience with a ‘healthcare professional’ treatment center AND the Physician Health Program. It is really sad how the other doctors in my group therapy and Caduceus meetings suffer at the hands of the PHP. Their stories break my heart. I am glad to be able to walk away and start fresh!” ~ Max
13 Tips for Confidential Mental Health Care for Physicians
“I’ve tried everything including PHP self-referral (with the noose around my neck). Far and away the most destructive action was PHP referral.” ~ Tony
“About 18 months after graduating from residency and taking what I thought was my dream position as a new faculty member doing hospital medicine, I slipped into a suicidal depression and ended up doing ECT as a last resort. I thought that was the worst things would ever get, but when I found out I my husband was having an affair while I was working my ass off doing 80-hour weeks of call and hospital medicine, I was caught completely off guard and made a horrible, horrible decision to quit trying. I overdosed on a combination of Tylenol, Clonazepam and a bottle of wine. I was taken to the hospital where I work, and someone decided to call my CMO, who got the PHP involved. From there, I lost all my pride, almost lost my license, have had to continuously hang my head in shame every time I apply for a license, privileges, participation with an insurance plan and disclose my ‘dirty little secret.’ Oh, and I paid them over $7000 of hush money. All so they could call me once a month to ensure that I was doing all the things I would have been doing anyway: seeing my psychiatrist, my therapist, my couples therapist, etc. Geez, Pam. That just turned into a PHP rant. Sorry, I’ve just been doing licensure applications for a new state and new job interviews, and it’s bringing a bunch of anger up. We’re moving to California when my youngest graduates from college, and it’s turning my job search into a huge trigger-y mess! I ran into an article the other day about PHP and physician suicide the other day, and you were mentioned, so I’ve actually had you on my mind. I’ve thought long and hard about trying to write a book about my experience with the PHP, but I’m still not sure I have the distance and detachment I need from it to do it. I think it’s important that people understand what a scam this is, but maybe it’s a retirement project?” ~ Carmen
“I have had serious depression since med school. I self medicated and abused alcohol for a lot of years until I figured that out. I have self prescribed antidepressants and also have psychiatrist and therapist. I try to follow the psychiatrists instructions but at times I will crash and they are not available so I try something myself and then tell them what I did at the next visit. I can’t go 3 months not being able to function well waiting for an appointment.” ~ Patrick
“I have eaten, exercised, quit, thrown hay bales, thrown my pager, yelled, done counseling, seen psychiatrists, been hospitalized having detailed suicide plan down to supplies and practice, committed to not dying by suicide, played saxophone, gone to more counseling, meditated, cooked, eaten, drank Diet Coke, drank alcohol despite a strong family history of alcoholism and a general terror of alcohol consumption, drank Coke, and finally trying to learn how to love myself again…which is pretty tough when you have been told you’re worthless by the world including the people you respect most (physicians) for 45 years. Oh, I have self prescribed but only when I didn’t have time to see my provider, which is to say my FP NP, FP MD or Psych MD depending on the year although honestly an FP NP will do pretty much whatever her physician patient requests so I’m not sure that’s any different than self prescribing. I do have some ‘illegal’ Xanax for crisis situations that were prescribed to my daughter. Oh, and I did overdose once on Ativan without suicidal intention but with a ‘I need to be unconscious for a while intention’ but that was prescribed to me… thus the illegal Xanax because physicians pretty much don’t trust me with benzodiazepines now because I might overdose although metoprolol is in my prescribed list, like that makes any sense. It’s pretty hard to die by Benzo overdose.” ~ Ellen
“Isn’t depression part of being a physician? It starts in medical school when you have to learn how to study all over again, because the old ways you studied to get A’s as an undergrad don’t work anymore. You are made to feel small at every turn. It continues through your board exams (constantly feeling you failed, even if you didn’t), and well into your residency, when you quickly discover you don’t know anything and are often reminded of that fact by less-than-sensitive attending physicians. You learn quickly to hide your feelings, because being a doctor, by its very nature, implies tremendous self-sacrifice. It implies putting your own needs on the back burner for many years in pursuit of medical knowledge. This, in itself, is rather depressing, don’t you think? But legitimate clinical depression can creep in too. And often does. During my internship, I found out that at least 75% of my fellow residents were on SSRIs or other antidepressants, just ‘to get through it,’ because it was so horrible. Depression, or a constantly depressed state, is more or less the norm in medical school and throughout one’s residency. It’s truly a wonder that more doctors don’t die by suicide as they go through this lengthy, rigorous, and often heartless process. Well, the height of my depression occurred after medical school and after my residency when I was working primary care. I decided the only way to preserve my own mental health was to get out, which I did. I quit my job. And I quit a subsequent job as well. You have to take control of your own situation as a physician, because in the world of corporate medicine today, they will literally work you to death. There is little or no consideration for the feelings or the health of physicians, many of whom have to work when they are sick themselves—or face criticism or retribution. It is a truly heartless system where the only thing that matters is making money. But the money is not being made by the physicians, at least not the primary care physicians (maybe the cardiologists, orthopedic surgeons, radiologists, and neurosurgeons). The money is being made largely by the business people, the managed care and pharmaceutical industry executives and other third-party players. And if you’re a woman working in medicine today, you have yet another reason to be depressed—sexism in medicine. Women consistently earn less than men in medicine, and also have more trouble advancing professionally compared to men.” ~ Joel
“I was depressed clinically. I saw my family doctor and tried some antidepressants. They were not that helpful. I did not seek specialist care until I had been sick for a long time. Treated myself with ethanol, 2 to 6 ounces per day. Crashed. Hospital thought the best way to deal with this was to fire me.” ~ Ron
“Pamela, Yes I’ve been depressed as a doctor—ever since my postpartum depression as a third year med student. First, I did nothing and withdrew from friends, family, and interests. I’ve had moments of what I’d call my best Facebook self and became a strict bedtime adhering good diet eating runner/gym goer for a spell (and looked damn good in a pair of jeans) until I could see that plan didn’t help me feel like I stole my life back from the gaping mouth of medicine. I self prescribed antidepressants and even bought them through a drug wholesaler to hide my shame of my illness for fear no one would trust the judgment of a depressed doctor. I sought help from primary care docs, psychiatrists, psychologists and several therapists and life/ career coaches and I can never seem to be “ok” with depression. It’s hard to sort out. I’ve never been fired or dismissed from work. I’ve never been out for long periods because of it and I’ve never been hospitalized or suicidal. Like a functional drunk, I’m functionally depressed. I have good days and good weeks and I also have horrible mind numbing days that all run together for months on end and I look back and cannot fathom how I was surviving not to mention caring for others. I’ve been cynical , angry, optimistic, aggressive, passive and passive aggressive. I had periods where I drank everyday and even considered drinking before work but never did. I’ve numbed my mind with pot in Colorado and Seattle. I’ve had affairs and even fucked a guy in my office while on call. True story. So yeah. I’ve spent a life and a career trying to simultaneously handle and avoid this ever present shadow of depression. Which might I add I never experienced prior to med school.” ~ Laurel
“During my fellowship training I was treated for depression/OCD because of the extremely difficult work environment there. I was illegally terminated from said fellowship (per EEOC Decision), and have had periods of homelessness and unemployment and underemployment since then. The past five years have been even more trying than my four years of medical school. My journey through medicine has taken so much from me in every way.” ~ Sara
“[To treat my depression] I quit what I had always hoped would be my ‘forever job,’ where I would work until I retired for my small town critical access hospital. After years of boorish mistreatment, and watching them fire a 20-year veteran of the local medical community, I realized that I had to take control. I quit, and am, unfortunately, in the middle of legal action against the administration, as they couldn’t even let me resign in peace. If I could walk away without further financial insult, I would have washed my hands of it. In addition to the MD they fired, they had 3 MDs (including me) and a PA resign in a three month period. I will admit, though, that I was trying to figure out a ‘way out’ that would have gotten my family my life insurance, until I realized that I was in control and walking away jobless with my family intact was better than my family without me. Reading your blog helped immensely in that aspect.” ~ Michelle
“For years I tried to heal myself while employing the common coping mechanisms of intellectuals (workaholism, intellectualizing, OCD behaviors, obsessive exercising, etc.) in addition to repeating self-destructive patterns in relationships. Then I finally waved the white flag: My healing & recovery has included: Individual professional & church-based counseling, Christ-centered support groups, persistent personal prayer & dedicated Bible study, exploration of generational roots of my issues, and creative writing in the forms of journaling, poetry & prose (including memoir and a future book).” ~ Nadine
“I am thoroughly disgusted and somewhat depressed, as a direct result of my experiences in medicine. Thank God for sobriety and having some tools in the toolbox of life. I have realized recently that the environment of practicing medicine with corporate contamination and yes..bullying, is really the only truly dark spot in my life. I am allowing it to rob joy from a sober, happy, and otherwise pretty healthy life. For that, I am responsible. I am actively in the initial stages of planning my exit to something similar to what you promote. The only snippets of joy found in a typical workday are the times when I say to hell with metrics, throughput time, and the high pressure move ‘em in, move ‘em out mentality, and sit with a patient that truly needs me. These folks are often the ones that are terminal, dying, or the ones that have been shunted through the assembly-line system like cattle with little or no true explanation of what is happening and what their choices are. I have deep gratitude for these folks allowing me to work together with them. I feel blessed, even in the sad instances because I am doing what I was trained to do, what I am good at, and what satisfies the soul. It goes against the grain of corporate medicine on every level. I hate my job with exception of those few moments I can carve out with a few patients.” ~ Rick
“Yes, I have been depressed. To tell u the truth seeking professional help is taboo… ur looked upon as weak so I try my best to deal with it myself. I’m considering quitting.”. ~ Robin
“I’ve had 25 years therapy (psychoanalysis), brief trial self dispensed Bupropion and Fluoxetine (not much benefit but the Wellbutrin helped me fight my way through a deposition). Overeating and wishing it all would end. Never went to a physician for help always afraid of being judged and excluded or reported in some way even though I was able to carry on my duties. Always sought treatment from non-physician providers and always paid out of pocket. Being in psychiatry made it ok to be in psychoanalysis back in the day. Thank you for all you do you are a life saver.” ~ Denise
“I have been actively suicidal over the past 7 years more times than I can count. In a strange way it has become one of the few comforting constant areas / states where I feel I exert some degree of control and autonomy. What I think I experience when it comes to my profession goes beyond ‘Clinical Depression.’ It’s the depletion of one’s humanity. What I see from the mirror staring back as I cross into my 40’s is many times unrecognizable to me.” ~ Mike
 “I tried to do the work-life balancing thing, making sure to do fun stuff on my off days so that I could unwind. Most of the time, since I have limited free time, all I did was to eat out, which led to it being self-destructive. I also talk to close friends at times about how things are going, but, most of the time they can’t really relate or most of the time our free times don’t match. I’m usually free after lunch when I get out after a 28-hour shift, while my friend is in the middle of her workday. I’m usually asleep when she gets off work and so we don’t get to talk much. Eating out too much made me continue to gain weight and I totally have lost self-control. My mind, when tired, wants to eat even though my body is just begging for good quality sleep. I don’t know why, but I feel that I was just wasting time sleeping when I should be doing something else. However, I usually end up binge eating because my mind is too tired to think of other things to do than eating and sleeping. The cycle goes on and on up to this day. I’m really frustrated at myself for this bad habit.” ~ Abigail
“I tried to do the work-life balancing thing, making sure to do fun stuff on my off days so that I could unwind. Most of the time, since I have limited free time, all I did was to eat out, which led to it being self-destructive. I also talk to close friends at times about how things are going, but, most of the time they can’t really relate or most of the time our free times don’t match. I’m usually free after lunch when I get out after a 28-hour shift, while my friend is in the middle of her workday. I’m usually asleep when she gets off work and so we don’t get to talk much. Eating out too much made me continue to gain weight and I totally have lost self-control. My mind, when tired, wants to eat even though my body is just begging for good quality sleep. I don’t know why, but I feel that I was just wasting time sleeping when I should be doing something else. However, I usually end up binge eating because my mind is too tired to think of other things to do than eating and sleeping. The cycle goes on and on up to this day. I’m really frustrated at myself for this bad habit.” ~ Abigail
“After years of bullying, I gained weight, cried, lost relationships, friends, isolated myself—changed jobs—I was depressed and feel like it cost me years of life and joy. Thought about dying. Still have PTSD—despite enjoying the roll of medicine, I am exhausted by the demands and the perceived professional competition, the back stabbing. It’s better now that I’m older. Still Everyday is count down to retirement—a long marathon—paying back thousands of med school bills and knowing I can’t get the time back nor can I quit as I am captive by bills.” ~ Lydia
“Medical school into residency, I ignored [my depression] for awhile, started on small dose SSRI from my family doctor, intermittently thinking about driving my car off the interstate on the way home from work, more psych appointments, more meds, feeling better through med school graduation, intern year had ups and downs, venting via text to high school friend (also with depression) on the shitty days, so far I’ve had fewer depressive times as a second year resident.” ~ Jennifer
“For self-care when I start to feel myself slipping I pick 3-4 of the things on my Rose Anti-depression Plan 1) Go to bed by 11:00 every night. 2) Begin each day with 15 minutes of stretching along to worship music. 3) Exercise 150 minutes per week or 20 minutes per day. 4) Eat 18 servings of vegetables per week. 5) Keep sweets to a minimum. 6) Use the sun lamp 15-30 minutes per day. 7) Keep gratitude journal. 8) Have regular devotional time. 9) Have friends over for meals. 10) Engage in art/music (quilt, drawing, watercolor, guitar, etc.) 11) Finish tasks and minimize distractions/interruptions. 12) Read books. 13) Spend quality time with family. 14) Consider other ways to simplify life. 15) Consider counseling. 16) Consider medication. ~ Rose
After collecting all these stories, I’ve had some revelations about my own responses as a depressed doctor. So I’ll add my story to the mix.
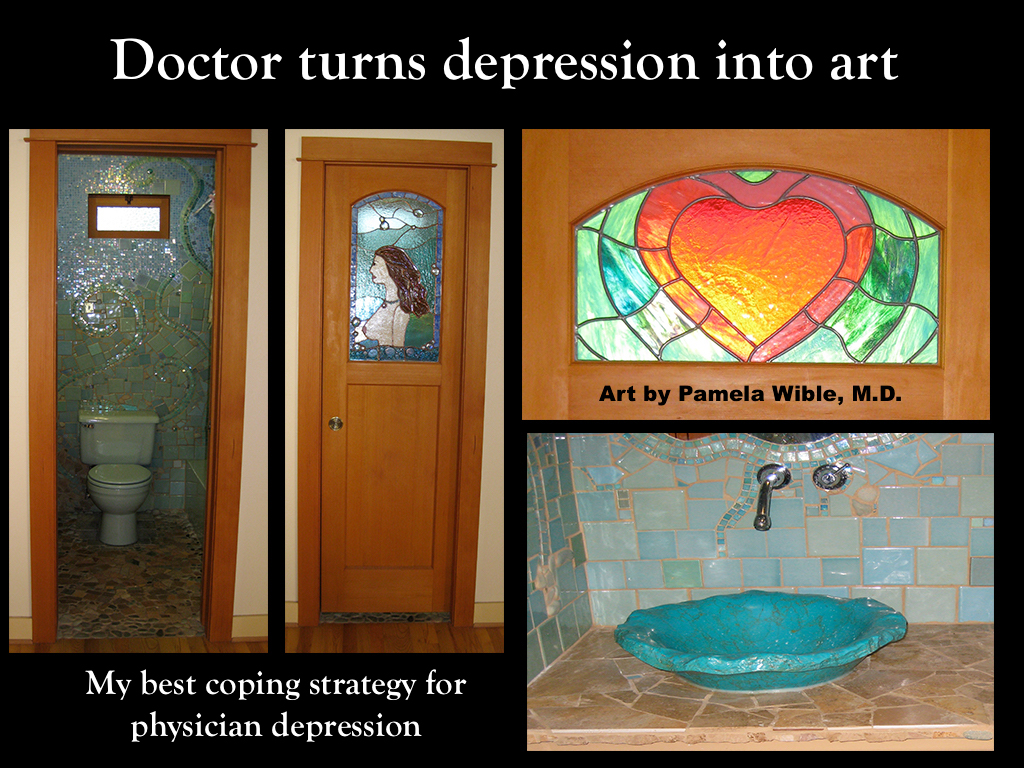
“First year of med school was by far the worst year of my life. I cried constantly. Cried myself to sleep most nights (one morning my eyes were actually sealed shut from crying!). Called my physician parents for help. Not helpful. Mom (a psychiatrist) mailed me antidepressants (Trazadone). Didn’t help. I kept crying. I stopped eating sugar. I made it through med school on NO caffeine! I became a strict vegan (then would sneak to the store at midnight to eat string cheese). Like Caroline, I rescued ‘too many pets trying to think that caring for them will help me.’ Had an apartment full of strays. Quit med school. Then realized I had no money to leave (and my tuition was paid) so my anatomy partner convinced me to stay and ‘to keep taking tests and see what happens.’ I graduated. He died by suicide. Had sex with my best friend in med school’s boyfriend! Years later, he died by suicide. After his funeral, I apologized (for both of us). She understood. Threw myself into my patients’ pain to distract myself (note: I was always at my best with patients) yet ended up suicidal due to complete disgust with assembly-line medicine. I prayed, journaled, meditated, went to random psychics on the side of the road, energy healers, shamans, massage therapists, and all kinds of counselors. Rare binge-eating then attended Overeater’s Anonymous (even though I’m not an overeater). Slept A LOT. My mom gave me Prozac. Didn’t help. I never saw a psychiatrist because I figured the profession that wounded me wouldn’t be able to fix me. I never drank alcohol (yuck!) or treated my depression with illicit drugs. Instead, I did lots of art projects around the house. A mosaic mural covering every square inch of my bathroom that took nine months. Intricate 3D stained glass in doors and windows. Obsessive knitting. Creative writing. Got divorced after my husband had an affair. Had to sell the house with all my art. Quit a ton of assembly-line jobs until I FINALLY had the courage to open my own ideal clinic in 2005. Since then I’m no longer depressed!!!! Go figure . . .” ~ Pamela
Bottom line for me is occupationally-induced depression and suicidal thoughts can not be cured by staying in a crappy job while doing a beautiful bathroom mosaic, rescuing stray animals, having affairs, obsessively knitting, or numbing the pain with Trazadone or Prozac. These are COPING mechanisms for a dehumanizing medical education and terrible working conditions. There is nothing intrinsically wrong with me. My depression resolved when I extricated myself from assembly-line medicine and became the doctor I had always dreamed of. (Incidentally, I’ve spent more in various therapies to recover from the trauma of my medical education than I did on med school tuition!). If you are a depressed physician and need help, contact our physician suicide helpline.
Have you been depressed? What did you do? Leave your (anonymous) comment below.











In college, I just wanted to be an anthropologist. Society didn’t allow such action. Went to medical school instead. Drank & did drugs. Flew through it. Decided I want to do psychiatry. I was told that wasn’t real medicine. Completed first year nsx residency. It was trauma; pure & simple. I saw gross malpractice, experienced sexism & bias bc I am a well dressed punk. Attempted suicide with an MVA. Gave up and did FP bc psych was so long. Entered some jobs I hated. Sued one. The only redeeming factor was that I loved my Medicaid patients. Received a DUI. Totally sober for two years. Went to a course on patient boundaries per the board due to not reporting suicide attempt from 2009 in 2012 application. Yes, you read that correctly. Mind you, in 2014, my friends and family still didn’t know it was a suicide attempt, but the board did. I did some snow; someone narced. Medical Board insinuated I was running a rx ring. After almost killing myself at inpatient rehab, found great tx in SD. Board did not accept it. They had dropped all allegations except snow & one stating I had rxed benzos wo documentation. My previous job did not provide all the documentation to the board. I had documented. I also had a very low positive THC from CBDs of 24. I dreaded the non-therapeutic HPSP groups. I was done. I surrendered about four weeks ago. I spent 2-3 weeks actively suicidal; dreaming of ODing on TCA & then shooting myself. I did nothing for days, but cry. My psychiatrist started me on a new med that essentially masks the pain. I am now stable on desipramine, clonazepam, clonidine, modafinil, CBDs, & THC. Stable meaning I am functional and not holding a .45 debating. Stable meaning I can take my four yr old daughter to go buy eye shadow today. Stable meaning I am alive. It’s still fresh, but I will persevere. My mental health, happiness and compassion are not worth practicing anymore in such malignant environments. I never took meds until my PGY2 year. This suffering is due to medicine. We must fix it & I greatly respect your work.
Wow. Life was normal before med school?
The only reason assembly line medicine is even bareable at all is that I have a plan to escape and start a direct pay clinic instead of continuing on with this dehumanizing, degrading, liability creating, burn out creating “profession” that medicine has turned into. If the suits in business of medicine think that they can enslave doctors like this they are WRONG!!!! There will be a revolution!!!!!! Either a silent revolution where doctors are quitting or choosing other professions or an active one with direct pay clinics popping up all over or both. Both btw are in full swing already and spreading!
Yep. Docs are leaving assembly-line medicine en masse to create ideal relationship-driven practices all over the country. Great time to be alive! FUN to watch people waking up! Free-range physicians much better than factory-farmed. CONGRATS on your emancipation!!!
What a great article! I knew there had to be other doctors with this problem, especially since we live in an age, and in a society, where anxiety and depression are so widespread, but I had no idea it affected physicians to the extent that it does! I still have nightmares about medical school and residency but I can say one thing with certainty: you (doctor) are screwing yourself if you are still working as an employee. I have been an employee (the law calls you a servant-employee and believe me servant is an apt description and slave an even better one), I have been an independent contractor (not much better), and I have been self-employed. I will take self-employment over anything else every time. There is no one to tell me what I can wear, how fast I have to move, or how many times I have say “yes, master” when they tell me what to think, say, or do. If I had to make a choice between remaining self-employed or continuing to practice medicine, as much as I love medicine, I would rather be a self-employed ANYTHING than an employee-physician. And as for “the boards”…..SCREW THE BOARDS! Why take them? Why waste the money? If every doctor would tell them what they can DO with their boards there would be a lot less depression among physicians!
Agree with you 100%%!!!!!! You took the words literally right out of my mouth!
I play the lottery when I get really depressed with assembly line medicine, I also binge eat junk food, or call in sick frequently when I feel bad.
Oh yes! I have heard of that before. I believe residents play lottery to escape medicine & pay off their loans. Ugh.
Thank you, thank you, Pamela! Education for all of medicine. This is just encouragement to keep on! Your work is sorely appreciated…by so, so many!
-Robert
Oh thanks Robert!!!! I still want to interview you!! When can we talk my friend?
Thank you, Pamela. Anytime.
Ok! I’m calling you on that.
I had my daughter half way through medical school. Then I got divorced three months later (7 year marriage) He became abusive of me after I got pregnant because he thought i should quit medical school once i had my daughter. At 16 I had been placed in a foster home because my father had got me pregnant. I had forced that into the back of my mind and having my daughter and my husbands abusiveness brought it all back. Plus I could not move back to New York to live with my parents so I had to finish medical school in Texas as the sole support of my daughter. Plus I developed a big case or PTSD and depression. All the sleep deprivation made controlling the memories impossible. I finished medical school and went into psychiatry. But it was a disaster. The attending in my first pscyh rotation deliberately went after me and made my life a living hell. It only got worse as the year went on and I was on every third night call and taking care of my daughter who would stay up all night when she got to see me. She was two when I started residency. I had a great babysitter who watched her while I worked even while on call. I lived by her, three houses down in a poor and dangerous side of Dallas. I was the only white person for miles. I was 100 pounds and five foot three at the time. I ended up dropping out of residency in April of the following year. Mostly because all the psychiatrists felt I should stay home with my daughter. And they actively punished me for doing my residency as a single female. This was in 1989. It shocked me how they treated me. They actually expected me to give up my daughter to an adoption agency. Then I got very depressed and was hospitalized. A year later I was well enough to work and switched to a family practice residency. They were nice to me. But it was too much to work full time and be a parent full time. And I got sick again in 10 months. You have to sleep sometime and not sleeping at all was too much for me. I tried the residency one more time and lasted 10 months the second time. SO I did 30 months total of residency. So I went out and practiced on my own in nursing homes. This worked well because I love the disenfranchised. I was very busy and was medical director of a larger hospice and 3 large nursing homes. Then I brought my sister down to help me in my office in 2008. She brought my father with her. Which was Ok by me. He was a burned out drunk and had very bad health. He spent all of 2008 in and out of the hospital and long term hospital ICU”s in December of 2008 we brought him home to my house on hospice care. This was easier then spending the night in the ICU with him. Which I found exhausting. Plus I was on call 24/7 for my 150 hospice and 800 nursing home patients. When he moved into my home he developed sundowning and I would have to sit up with him at night so he would not get up and try to walk. So I really was not getting any sleep at all. I brought him down to my house from New York because He lived far from everyone. He was dirt poor in New York. And living in filth. And I needed him to know I had forgiven him for what he had done. He died 8 weeks later. I was exhausted and busy with my practice. Then in September of 2009 I noticed that the books were not matching up. I corrected them and thought nothing of it. I thought I had just made a mistake. Then I noticed in December of 2009 that the books were really a mess and even though I had seen more patients then ever I was actually getting less money. So I started to look into them more closely in the New Year. It was in February that I finally found out for sure what was happening. Even though I had paid my sister a good salary and paid for her to go to college to finish her degree and paid for all her medical bills she had embezzled from me. To the tune of 100,000 dollars. I fired her then in became very depressed and suicidal. I tried a lot of different medications and then ECT then in November of 2010 I resigned from all my medical directorship jobs. In February of 2011 I turned over all my patients to another physician and quit practicing medicine. I was severely depressed and tried multiple medications ECT twice and rTMS. I self reported the depression and was duly punished for it by the medical licence board. I heard about a novel treatment for treatment resistant depression and enrolled in the study. A deep brain stimulator was implanted in my median forebrain bundle in October 2014. The depression finally lifted in 2016 and I am depression free now. I returned back to work part time in late 2016 and am now working full time since May 2017. I work full time for the hospice I worked for in 2006-2008. I am so glad to be back at work. But I do not think most doctors are very good about depression. Even one of the study doctors, a woman, diagnosed me with a personality disorder when I did not get better right away. They have put in the articles they have written about the DBS study that I have a dependent personality disorder. It is interesting because as a medical director and a successful one you can not have a dependent personality disorder and be so successful in the role of medical director. Interestingly both women, I and another in the study were diagnosed with personality disorders with depression and both men were diagnosed with just depression. I was made to feel a along that I was the only doctor who is depressed and there had to be something seriously wrong with me. And the Texas State Medical board monitoring system had me feeling very bad about myself. Since I wasn’t working I got them to reduce the 1,200 a year fee to 300 dollars a year. But they forced me to go into therapy the whole time I was being monitored by them even though I did not need it. So I paid 30 dollars a copay for the therapy and I had nothing to say to my therapist. Plus they wanted q 3 month monitoring letter filled out by both my therapist and my psychiatrist. That cost me 25 dollars a letter. SO an additional 200 dollars a year. I found it insulting and the form is geared to those who have a alcohol or drug problem something I have never had. I felt like I was being treated like a criminal. It was awful. At least my contact at the Medical Board PHP program was nice to me. So it has been very helpful to see that other people have been through this. Now I do not feel like I am weird and have to be ashamed. Thank you
I realise this is a human medicos blog, yet the same traumatic depression syndromes apply to we who are veterinarians.
Dear Pamela, I came across your article here, as it was forwarded to the Australian Veterinian Network FB page. Personally speaking, I also have two of my immediate family members as junior medical officers here is Australia.
Do veterinarians face the same issues? Yes. Maybe to a greater extent. Our suicide rate in Australia is 38/100000 pple. 4x the national average. (Vets have access to pentobarbitone in Australia). The rate of ‘burnout’ is twice the general population. These are distressing statistics.
Personally I have suffered as a veterinarian – depression, suicidal thoughts (and actions – to the point of intravenous cannulation, driving maniacally), self medication, alcoholism, a marriage on the rocks, (infidelity), plus other symptoms. What did I do? Took a long vacation overseas. Realised that life is short. Live each day as well as I can. Sorting out a dead marriage (by moving on). Adopting a new world view.
Do you have connections with veterinarians?
I’ve had depressed veterinarians attend our retreats (open to all in health care & human services). I have heard their stories which in many ways seem worse than what we face in human medicine. Less pay for daily tragedies of animals. Many doctors have thought of first becoming veterinarians (like myself) but could not imagine euthanizing so many animals. So I believe we are all kindred spirits injured by a system that trains us to become callous and cold-hearted. The details vary but the human debris field is similar. We are losing far too many loving, competent, brilliant healers in all fields. Not sure we are accurately collecting the real suicide data in any of these professions.
Too much to say. Am extremely slow typist. If you want to call me to hear what I have seen and been through, email me and I will give you my phone number. I have had colleagues and residents commit suicide. I have struggled with severe depression and at times have felt suicidal. I have continued working several times when I had life threatening medical problems. We were conditioned to do that. Thank you for your bravery in speaking out about depression, suicide, and abuse of physicians by others and also by themselves.
I’ll email you now. Love to hear more (even confidentially). I’m so glad you are still with us. Time for us to unite and stop the cycle that wounds us and prevents us for reaching out to get help. xo Pamela
Thanks,Pamela. John
Dear Dr. Pamela Wible,
After 43 years in Family Medicine, I found myself frustrated and not enjoying my practice. With the advent of the unclear EMR requirements of the ACA, I burned out and retired my licenses. I was still taking my Wellbutrin and Depakote prescribed for my by my psychiatrist’s after 3 episodes of manic depression induced suicide attempts.
Fortunately with the help of sweethearts and friends, I survived without brain damage or physical defects. God was on my side. Thanks God and my Intensive Care Medical Team and Helicopters!
Now, I am faced with the title of Impaired Physician, not Controlled and Stable Manic-Depressive illness.
Actually, I was allowed to practice family medicine after my third suicide attempt. I volunteered and successfully completed a required 3 year rehabilitation as a result o my suicide attempt. The Maryland Medical Society(Med-Chi) protected me and saved me and my medical license.
Since I complied, I was granted a unrestricted Maryland Medical License in 2003 When I burned out, I was so upset, stressed and unhappy practicing medicine. I caved in and then I quit–Gave up all my Licenses in Maryland and Florida along with my Maryland Controlled Substance and DEA licenses.
I was numb and did not realize the consequences of my actions at the time of my decisions. I thought I could relicense in the future without any problems.
To my surprise, I was labeled IMPAIRED by my present voluntary physician monitoring program- Health Practitioner Monitoring Program (HPMP) in Richmond Virginia.
I received my Restricted License after a Special Credential Committee meeting with the Virginia Board of Medicine in May of 2016.
However, the Health Physician/Practitioner Monitoring Program (HPMP) still labeled me and judged me as impaired.
The HPMP required approval of any medical position I accepted including Voluntary Clinic work for patient BP monitoring at my St. Mark’s Lutheran Church Also, the HPMP required on site supervisor monitoring of my medical acumen and mental performance, monthly at any medical job site.
I have been unsuccessful in finding a family practice position because of these stringent requirements by the HPMP. I have been treated medically for my disease, Manic Depression since my last Suicide Attempt in 2002.
I have been compliant and stable mentally and physically since my last suicide attempt. I have been evaluated by my Primary Care Physician and Psychiatrist and found to be mentally and physically safe to practice medicine with no contraindications.
My dilemma–The Boards of Medicine in the United States and their Mandated Monitoring and Rehabilitation Programs do not distinguish physicians who are ill from those who are impaired.
The Distinction of illness and impairment is central to treatment according to the Federation of State Physician Health Programs, the American Society of Medicine and the American Psychiatric Association.
Conflating Illness with Impairment results in far too many physicians being subject to investigations and treatment that restricts them finding any medical work.
The Federation further defines Impairment as “the inability of a physician to practice medicine with reasonable skill and safety.” Physician illness and impairment exist on a continuum, with illness typically predating impairment, often by many years.
This is a Critically important distinction, illness is the existence of a disease. Impairment is a functional classification and implies the Inability of the physician affected by the disease to perform specific activities.
So, I have an illness Manic Depression and I have been treated and I am compliant with my medications. Why has the Virginian HPMP judged me as impaired. Are Diabetics or Cervical Spinal Injured Physicians impaired because they have controlled diabetes or functioned with limited movements because of paralysis?
I have doctor friends who are diabetic and/or paralyzed from the neck down that are functioning without impairments in Surgical and Medical teaching programs hospitals and private practices.
Is this judgement by the HPMP fair for physicians like me, John J. Shigo.
I feel strongly that I have been judged unfairly because of my depression and mania in the past.
At present, I am now unable to find a locums tenens position or part time job in family medicine.
This decision by the HPMP is totally unfair and judgemental without justification or merit.
The mandatory physician treatment programs need to recognize the difference between illness and impairment as defined by the American Psychiatric Association. The HPMP must therefore revise their contracts and not judge all physicians with a disease or illness as Impaired!
My dilemma of being treated as impaired began when I signed my Participation Contract in June of 2016 with the HPMP. I voluntarily told the Virginia Board of Medicine that I would participate in the HPMP Program.
Also, I was totally honest and truthful to the Virginia Board of Medicine at my Special Credentialing Committee Meeting. I am a rotarian of 34 years and have pledged to always tell the Truth.
My Dilemma—- Returning to work as a Family Physician.
Dr. John J. Shigo
July 11th, 2017
I have not taken care of myself…and I should know better as a family medicine doctor with a chronic disease – secondary progressive MS. I became a doctor because of how poorly I was treated when I was diagnosed and it was the worst decision I ever made. My disease has gotten so much worse with years of not sleeping, anxiety, depression…I was on three different antidepressants, one stimulant, and a sleeping pill until I just smoking pot. *shrugs*
I have contemplated suicide several times. Step 1 inadequacy even when I’m scoring in the high 80% correct. Made to feel worthless, useless or expendable. This isn’t the medicine I signed up for.
I get it. Been there. Medical training is kind of like joining a cult. You lose connection with yourself and others. Doesn’t have to be this way. Would you be willing to share what you had intended to sign up for? What were you hoping to do with your life in medicine? What was your original dream?
I didn’t anticipate how much of my energy would’ve been exerted to refining this craft. I uprooted my entire life and lost myself along the way. The glitz and the glamour of medicine suddenly lost its vanity while studying for step 1. In undergrad I really wanted to be a diagnostician (IM), but between bureaucratic red tape, and discouraging sentiments from current IM attendings, I really don’t know what I want anymore. Ultimately I just wanted to help people, but I wasn’t expecting to feel so broken inside. Medicine has made me feel inadequate, not worthy, and overall numb. I read every single one of those letters and had some relatable moment to each and every one. My wife and I are both medical students, and if it wasn’t for her, I would’ve definitely quit medicine or worse. If I could’ve done this all over again, I would’ve became a police officer. Ya, that’s a dangerous job, but although I may die physically as a police officer, I feel I’m already dead emotionally in medicine.
“I would’ve became a police officer. Ya, that’s a dangerous job, but although I may die physically as a police officer, I feel I’m already dead emotionally in medicine.” That really captures it all. I’ll email you. Here if you ever need support. Life DOES get better after med school!! Especially if you surround yourself with the right mentors. <3
Amen to all of the above. The problem is pride. Most doctors are unable to admit they are broken. Most of us were broken before we started and the training just makes it worse.solution??
pay doctors a living wage and lot more time off so they can see that life exists outside the treadmill. Get rid of onerous malpractice so we don’t have to worry about litigious families bullying us into treatments or tests we would normally not order. Medicine has lost all of its nobility and is not a vocation. It’s a stressful job that you train a third of your life for, then think about how the heck you can retire for the next third! I’ve been through drugs, alcohol, anti depressants etc. best thing was walking away from the job at 58 years old before I had the big one.
Get DEPRESSED? Heck NO, I’m way into Healthy Denial and lots of IRONMAN Triathlons….Give me another 140.6 miles please. I don’t have time for this “depression” nonsense! And I really don’t care if others do not understand me.
Thank you for this article. When I was in med school, I applied for a competitive specialty. I had already given so much- the first in my entire extended family to even go to college, 2 years of med school applications, the threat of eviction and homelessness without any financial support all while studying for the USMLE- I deserved the specialty I wanted. I didn’t match. I had to scramble into an abusive surgery program in a place where I had no friends or family. I became so depressed, but the way I dealt with it was to turn myself into feelingless robot and spend the brief time when I was awake and not at work consuming alcohol and fucking any person who was willing (mostly Internet randos). Almost every morning walking to work in the dark, I would contemplate stepping in front of the city buses as they passed. Whether it should kill me or provide a brief reprieve from the misery of my soul crushing, isolating hell were both equally appealing and better than the shame of quitting and living in financial ruin. The thought that terrorized me about the bus idea was that I might wake up on the trauma service at work under the care of those whom I had grown to despise. Fortunately, I was able to match into another specialty, which has been much more fulfilling. At times I feel down, but I no longer hate my peers, my bosses, my patients, or myself.
I would guess you recognize some of those treatments used by your peers in the article. Looks like many of us have suicidal daydreams, use sex/ETOH/obsessive exercise/food as a distraction/self-medication. It’s unreal how we have been left to fend for ourselves with little/no support in a health care system with rampant human rights violations. It’s shocking (even to me) the depth of despair and the magnitude of the abuses against doctors.
When reading this, I felt like any of the stories could have been mine. I am particularly distressed by the role that my state’s physician health program has played in this for me. In a nutshell, I have been depressed on and off since medical school. I was first hospitalized for suicidal thoughts in residency and have been multiple times since. Luckily, substance use/abuse has not been an issue for me. I’ve tried everything from medication of all types, therapy (generic, cognitive, and DBT), group therapy, acute inpatient, residential inpatient, intensive outpatient, lots of ECT, ketamine infusions, mindfulness – you name it. I finally decided to resign practicing after years of agonizing, eventually going to part-time, and still not finding peace. A physician treating me in a residential program just before I resigned wrote in my FMLA extension paperwork that because of my depression, I had been impaired. Specifically, he said “She complained of depressed mood with associated anhedonia, anorexia, sleep disturbance, impaired concentration, feeling overwhelmed at work with subsequent suicidal ideation. Symptoms have caused significant functional impairment requiring an inpatient hospitalization.” In comes the state physician health program. I voluntarily reported my history to them and was required to sign an agreement lasting 5 years. If I hadn’t signed or if I fail to comply, they will likely report me to the state medical board. The highlights of the agreement are as follows: not practicing medicine, not prescribing, complete neuropsychiatric evaluation at the outset which costed $2000, ongoing quarterly reports from a “work-site monitor” (requiring me to explain the situation to my supervisor), my psychiatrist, and my psychologist, and a yearly $1200 “participation fee”. All because I sought and accepted treatment for depression. I feel as though I am a criminal, not to mention incompetent and crazy, not to be trusted to be the physician I spent so many hours and heartache – but also enjoyment and challenge – training and jumping successfully through all of the hoops to be. When I made the decision to tell my PCP twenty years ago that I was thinking about killing myself and accepted a prescription for Prozac from her, I didn’t know that it would ultimately mean the end of my career as a physician. Again, this because I sought and accepted treatment for depression. Medical students, residents, fellows, and practicing physicians should know that if they seek and accept treatment for depression or probably any other serious mental illness, they are risking losing the ability to practice medicine, as well as raising the possibility that the state medical board will reveal to all of their colleagues and the public that they have done so. Is it any wonder that people in this profession do not seek treatment?
This punitive environment in which physicians find themselves in is beyond INFURIATING! All that you write I’ve read before from other docs so this is not an anomaly. Depressed doctors who seek help CAN be penalized and publicly shamed. I receive a PRINT quarterly newsletter from the Oregon Medical Board listing all the physicians who are “in trouble” and who have various license restrictions. I’m sure many simple sought mental health treatment.
It will all sound familiar- affairs, sleeping whenever I wasn’t working, taking antidepressants (still on those). Moved to a concierge practice 2 years ago that I thought would be the answer- longer visits with patients, smaller panels- and I do have more time with my patients but the expectations are crazy- stay late, come in on the weekends, see patients at lunch, take work home every night- not what I was hoping for. We counsel our patients on healthy lifestyles ( I am a family doctor) but are unable to live them ourselves.
Draw a line in the sand. You MUST care for yourself first. Now that you are in your own practice you should have strict boundaries that allow you do this. Happy to talk to you. Please read this: How to say no for people pleasers
It hurts my heart to heart so many of my colleagues( and yes even though I have never met you , you are my brothers and sisters ). It hurts because nine jobs later I realized I know what it is to be depressed. Ive ignored it , withheld it from family and friends and just allowed it to eat away at me and become an unhappy person. I will bust my ass for a patient though. They dont deserve anything but the best of me despite what Im going through. This is not good for the soul of an MD though, and in the end you are really not doing them any good. I cry on the way to work . I cry at the end of the day.
A few months ago I called you Dr. Wible and that you answered the phone and actually talked to me may have saved me. I heard you but fear made me not listen.
Still wanting to do something for people who really needed it . I tried working at a a community health center. After a week I realized that abuse of the patients in the system , starts with abuse of the providers. I’m now done with medicine as it is. I cant tell you how many times I’ve been told that maybe I need medication to deal with the stress at my job. How about we make an effort to actually take care of a patient. I’ve been through every stage of grief their is for my medical career, for the times I missed with my family , for the husband I don’t have , for the children I don’t have , for the medical friends I don’t keep in contact with because they seems so happy in the profession and I just cant understand that sense of calm. I’m no longer afraid. I’m just tired of trying to do the right thing in a system that doesn’t seem to care.
Thank you Dr. Wible , I hear you
Calling you now Natalia . . . (just left you a voicemail)
I’ve had the normal ups and downs of mood, but never became depressed. Maybe the reason is I have never felt enough inclined to pursue glory or money, and so never allowed myself to be overworked. I started out in academic medicine, and even had a couple of R01 grants, but couldn’t sustain the grant chasing effort to be really successful at that. In private practice, I never worked more than 4 days per week and never saw so many patients that I burned out. In my best years, I never made much over $200,000. So what? That’s plenty of money. I’m still working about 1 day per week with occasional locums at the age of 73. I think the secret is that you have to have a life outside of medicine, have creative hobbies like art, photography, music (playing it, not just listening), etc. Physical exercise like hiking, biking, etc. helps as well. Once you burn out, I’m not sure you can ever get your interest in medicine back. If you think you are burning out, it is time to cut back or change jobs. There is such a huge demand today, that should not be hard to do.
I read your post on doximity, but could not comment there because, well i’m sure you know why.
I am a depressed doctor. I have been depressed most of my life, but aside from some secondhand Prozac from my mom’s FP in college, have never been treated. I have planned suicide so many times it seems normal. I don’t kill myself for the same reason I keep going to work: family duty and obligation.
My days off find me unbathed, bingeing on junkfood, sleeping up to 16 hours a day, and dreading each minute that ticks away until I have to go back to work, function competently, and pretend that i’m not dead inside.
My marriage has fallen apart because my ex is tired of me like this.
I hope only for one thing: a death that’s not my fault–maybe the tumor is growing and spreading as I write this–to end the miserable life that I don’t have the courage to end myself. In the meantime, I’m less than eight hours from another five days of hell, wrapped in a smile a caring, meticulous demeanor.
I know now that i’m not alone. Thank you for your writing.
Will you call me? 541-345-2437. I’ll email you now. I have some things that will help you.
Pamela!!! Thank you for this article, thank you for your work, and thank you for caring! Thanks to you, to the OBDoctorMom who wrote about her reasons for retiring from medicine at the age of 37, and especially to all the brave docs who have written comments sharing their deep suffering, I have received so much healing! The deep emotional and mental wounds that I have carried with me since med school in 1990 and all of their collateral damage (the mess I made) in my life were the reasons I walked away from clinical medicine 12 years ago and never looked back. Since then, I have been walking slowly down a path of self-forgiveness instead of self-loathing. I have begun little by little to feel some real compassion and understanding for myself after years of asking, “What’s wrong with you, you loser???” Most importantly, I have learned that I am not alone. I would like to assist you in any way I can to help our comrades who suffer so much. Like AA, wherein alcoholics help other alcoholics, I think that some of us wounded warriors of medicine can offer a great deal of support and acceptance to our colleagues. If there is any way in which I can be of service, please let me know. Again, thank you. I cried a lot yesterday reading this article and the stories, but for once, it was a good cry.
Wow! Such a broken system! We can definitely do better. Our “health” cannot come at the expense of the sanity and life of our healthcare professionals.
Amen Sister!!
Pam, thanks for identifying this problem. I am so encouraged by reading what others have written. My medical school training was very emotionally damaging, but of course we are supposed to survive the gauntlet to make the grade and become physicians. I was able to survive and retire by working for a large government agency and avoided having to deal with assembly line medicine. In spite of this I have suffered significant depression, had suicidal thoughts and have avoided disclosing my problems to anyone. I have always tried to act in a professional and confident manner. My profession has always inspired self-doubt, second guessing and terror that I would make a mistake and cause harm to my patients. The people who administrate the medical care in this country for the most part seem to be primarily focused on metrics. Our transition into EHR has added stress and made us into computer data entry technicians, which is fine, but that was not what I went into medicine to do.
My only comment is that my marriage has failed as a result of > being married too young, > not having a supportive spouse (in 30 years of vet practice, > I went 7 years without holidays numerous times, WTF!, > I grew up in a very fundamentalistic church of which I have no part of any more (I’m a humanistic atheist), > I’m an ‘ordinary’ but honest vet, > I’ve now entered into an extramarital relationship with someone likeminded, I’ve 3 adult of which ‘see’ that I’m happier outside of my previous marriage. (I’ll forever carry the title, ‘adulterer’, ‘deserter’, ‘infidelity’ etc). I’m not perfect – who is? I struggle in a small town veterinary situation and wish to start a new life. Is that bad? I’ve a divorce to settle….. I’ll not be the first one, to have gone through that, but am struggling not to turn to substance abuse.
Life sucks.
I worked in the Medical field for the past 40 plus years with some very internationally famous MD’s in Texas. The first Institution I worked with was absolutely toxic and the well publicized MD made everyone’s life a living hell, and took great delight in ruining careers by firing Residents in their last years of surgical training or others he felt were inferior. He was like the psychotic officer in the movie “Shindlers list” who would casually pick up a rifle on his balcony and shoot a prisoner walking through the compound for no reason other than he could. He was intoxicated with unchecked power. He was an insufferable prick, hated by all including those that survived only by boot licking. The problem became pervasive as those that survived looked upon their survival as an accomplishment and embraced the same behavior and carried it into the world to multiply like a virus. Those Residents that survived moved into Medical Centers around the country and gradually it became accepted practice that the making of an MD included the abusive insanity that everyone on this site writes about.
It is compounded by the shattering of an ideal that many embraced for years as young students. Believing that they would be contributing to the well being of citizens. The word “Health” became part of their vocabulary while their unconscious was continuously assaulted with “disease”…a contradiction that in my humble opinion contributes to the depression many experience. We have a disease treatment system in this country, yet we continue to describe it as “health care.”
The problems that many of the MD’s experience are shared by many non MD’s also. Allied health workers book long hours, takes call and deal with family members on a regular basis. In a Critical Care environment it is rare that one gets to see the final outcome of a patient that gets moved out of ICU unless it is to the morgue. Witnessing the collective grief of family members gathered bedside while life support is terminated on a regular basis results in an odd sort of detachment from life in order to continue functioning. Witnessing gross negligence that results in a patients death and yet dismissed so casually by those responsible as the cost of doing business cauterizes the soul. When death can be dealt with in such a casual manner it detracts from the joy and meaning of life.
I watched a women in her 50’s bleed out all over the floor in ICU from a torn Aorta post operatively. Minutes later I was in the cafeteria eating dinner and watching the news on TV…oblivious to the incident, or so I thought. Other incidents equally and even more horrific were witnessed over an over throughout the years and I thought I was fine. Then strangely, I started to have dreams, vivid dreams of cases that I’d been involved in years earlier, in some instances, more than a decade previous, replayed in vivid detail via a dream. I found myself recalling more and more cases that I had participated in over the years intruding into consciousness at the most random of times, and found myself becoming sad and even awakening at times from sleep in tears without being able to recall if I’d been dreaming or not. It was if I had been in a trance for decades and was regaining consciousness.
There are so many things so very, very wrong with our Medical System. Those in charge..the “Suits” have a mission that runs contrary to many of the well intended Professionals working within a System that does not serve the needs of the Patient or the Care giver…and yet we continue to repeat the definition of insanity..repeating the same behavior over and over with the same negative results. Is it any wonder we find ourselves feeling out of control of our lives, struggling with depression, thoughts of suicide, shattered relationships and self abuse when we immerse ourselves daily in system that broadcasts insanity? Is it healthy for ANYONE? Dealing with the system as it exists for any length of time will inevitably assure a psychological sepsis.
Maybe if the system crashes and burns we can start from scratch, a rebirth and opportunity to create a system that doesn’t demand that in order to save a life, …we must destroy our own.
The first step to culture change is speaking the truth. Health care and medical education has become an assault on our humanity for so many unsuspecting victims—the medical students who enter this system just wanted to help people. Psychological sepsis. Good one. Do No Harm film coming soon to expose the “Hippocratic Hoax.”
Hi Pam:
I started crying reading this because it’s so painful to know how many people are suffering the way that I have. I am on the mend but it’s still pretty fresh… Physicians care for people but who cares for physicians? It feels like no one, sometimes. We all know how that whole “Physician, heal thyself” goes…
I’ve been wanting to tell my story as well to let it be known that we’re not perfect, just human like everyone else. And we hurt like everyone else. And more often than not, the institutions in place to “protect the public from troubled physicians” just treat us like criminals. There’s just no compassion at all – it’s just business, like most everything else.
You’re welcome to contact me if you like. More people, not just other doctors, need to know about this! When I first started reading your article, I was thinking “The mainstream media needs to know about this”. But now that I think about this, not sure that would help unless you reached out to Sanjay Gupta on CNN. He seems compassionate…
Anyway, thanks so much for what you’re doing!
Christine, yep! I’ve been getting the message out since 2012 and media seems to be just catching on. The film will create a mass movement around medical professional mental health. Make sure you view the trailer. Will share when Do No Harm debuts in 2018.
Christine, also download the FREE audiobook here. You’ll love this!! https://www.idealmedicalcare.org/blog/physician-suicide-letters-answered-free-audiobook/
Thank you for your work. It’s good to know that “I’m not the only one” and to see that you have found a way out of the morass by helping others still stuck in it. I’m trained as IM, geri and palli and am currently being ground down by the Dept of Defense (active duty physician). I dread every Sunday night and every Monday morning. I dream of the month when I can get out two years from now, but have no idea how or what to do fix my situation so that I can do what I love. In fact, I don’t even know what love any more because my days off are spent with mindless internet surfing, reading and avoidance of my career as a physician. I’m afraid to talk to my husband about my reluctance to continue medicine because walking away from it would hamper our ability to retire. I have a lot to offer, but am not sure how to make up the gap in pay if I got out of the military before my 20 years was in and didn’t go straight to the VA to continue the gov’t service. I’m sure you have no answers for me, but I’ll continue to watch you with hopes of learning how to shape my own destiny. Once again, Thank you for all you are doing.
Oh I do have answers for you 🙂 I’ll email you now.
Interesting read. I am going to have to find your book. I am glad my kids are going into engineering, rather than following me into medicine. The stress and time requirements are unhealthy. I don’t even remember my 20’s. All I did was study and work. I would have a hard time encouraging anyone to choose medicine. Thanks for shedding a light on this.
I’ve smoked more pot than Bob Marley.
Beats suicide.
I’ve been an indentured servant to medicine for 20-something years, still owe on loans. No way to quit, but I’ve wanted to for slightly less than 20 something years.
I think you have a common coping strategy. Have you ever thought of liberating yourself (not from your physical body via suicide but from your employment prison)? Call me. 541-345-2437. Love to help you remove the chains Ben.
Thanks for writing about this important topic. Many of us suffer in silence, misery and fear. We are afraid the supportive kind faces we see at work will turn against us if we reveal our struggles. We look like top achievers, high RVU earners and great Press-Ganeys but when you try to let people know your health issues or family problems are driving you to the brink, many try to pop a pacifier in your mouth to shut you up. Therefore, I try to look as put together as possible with the protective umbrella of my “stats” to buy me time until I can escape to another career. Doctors are wonderful people but terrible listeners. The comments healthcare providers toss about regarding those with mental illness will make any physician think long and hard about the risk of disclosure. Therefore, I say nothing.
As with most things in life, it seems people prefer to not know about the difficulties of their fellow man. Few docs seem sorrowful that we have less time to hold the hand of our dying patients or to make sure we’ve thought about a viable well constructed patient-centered discharge plan. So long as the perfunctory boxes are checked everyone is happy…except the caring but weary doc and the vulnerable patient. Not being able to render a care plan that’s actually achievable by the patient just so we can say the encounter is complete is oppressive. I actually love my patients so this current system of building a new building but let’s not feed our elderly ED patients frustrates me continually.
I think we have lost our way as a society. We think better health comes through box checking and procedure lists. While these are crucial for safe predictable care they do nothing to help the medically complex elderly patient in the ED who is disenfranchised and lacks a real medical home. How does the current system deal with the 80 year old with eight serious chronic medical issues in a 15 minute appt?
I’m actually a young doctor who wonders how we are suppose to find the intersection of not working 25% over hours (unpaid), not dictating from home, not getting sued, but continuing to attain high press ganeys and high rvus while still providing thorough personable intelligent medicine, not checkbox medicine. Chronic health problems plus a strange sense of being an alien in your own profession are killers. I wish we were all better and kinder to one another so we could trust our colleagues to be a source of strength to us during trying times. Until that day comes, most of us will never let anyone know anything.
Dr. Wible,
Thank you for your honesty and brilliance. Recently I read that 83% of doctors thought about quitting medicine due to policy, it is 2017. This classic excerpt from “Atlas Shrugged” conveys the sentiments of many some six decades later, written by Ayn Rand in 1956:
The context of this excerpt comes from the protagonist Dagny Taggart’s inquiry to a physician as to why the doctor quit practicing medicine :
Dr. Hendricks says:
“I quit when medicine was placed under State control, some years ago. Do you know what it takes to perform a brain operation? Do you know the kind of skill it demands, and the years of passionate, merciless, excruciating devotion that go to acquire that skill? That was what I would not place at the disposal of men whose sole qualification to rule me was their capacity to spout the fraudulent generalities that got them elected to the privilege of enforcing their wishes at the point of a gun. I would not let them dictate the purpose for which my years of study had been spent, or the conditions of my work, or my choice of patients, or the amount of my reward. I observed that in all the discussions that preceded the enslavement of medicine, men discussed everything—except the desires of doctors. Men considered only the ‘welfare’ of the patients, with no thought for those who were to provide it. That a doctor should have any right, desire or choice in the matter, was regarded as irrelevant selfishness; his is not to choose, they said only ‘to serve.’ That a man who’s willing to work under compulsion is too dangerous a brute to entrust with a job in the stockyards—never occurred to those who proposed to help the sick by making life impossible for the healthy. I have often wondered at the smugness with which people assert their right to enslave me, to control my work, to force my will, to violate my conscience, to stifle my mind—yet what is it that they expect to depend on when they lie on an operating table under my hands? Their moral code has taught them to believe that it is safe to rely on the virtue of their victims. Well, that is the virtue I have withdrawn. Let them discover, in their operating rooms and hospital wards, that it is not safe to place their lives in the hands of a man whose life they have throttled. It is not safe, if he is the sort of man who resents it—-and still less safe, if he is the sort who doesn’t.”
Being well aware of the destruction of lives. What the public sometimes fails to understand as intimated in the above-passage, albeit a 50 some year old fictional work, the value of the intellect or mind if you will, of what level of science, math, physics, pharmacology, etc. required of those who are medical doctors, is mastered in less than 2% of the population. I see doctors retiring in their 40’s…It has been a little over four years since the passing of Christopher Norman Tulin, a wonderful man who practiced interventional cardiology in Colorado Springs for nearly 26 years. He scored in the 99 percentile of every test he took for medical school, and his boards. He trained at the Texas Heart Institute, and worked 18 hour days. He was Section Chief at both hospitals. Slowly and painfully, the rise of electronic health records, squeezes on reimbursements, and loss of decision making power…destroyed a brilliant man…the tragedy is unconscionable.
Been reading for 3 hrs now, never been here before, but im very glad to.
I guess my case is little bit different, im mexican and had my training here too, but after reading you guys, felt so related that it touched me real deep. (Excuse my english, is not very good but ill make an effort to share my story, i need to.
Got into medschool at 19, i was between music(i play several instruments since kid), electronic engineering and medicine. Music was out of question by parents, medschool was in other state so i took the oportunity to experience “living on my own”. I was sober at that time because i had some trouble smoking pot in my teenage years. Didnt drink either. As i went thru school, several times felt very alone, stressed and tired, thought in quitting most of the first 2 yrs, but then i didnt want to dissapoint family, so i finished training. Here in mexico we have to do 1 year social service at a public health clinic which is mandatory so your license can be released. This is where all started: that year i lived at this small public clinic in which i was mainly responsible for, i was so scared to deal with reality in this unknown place that most of the time i spent was studying because i didt want to harm none, i was 24 hrs a day active, 6 days a week, 1 day rest, people was kind and nice, so was i at the moment. There i experienced to lose a patient for the first time, a male around his 70s with a M.i, i was alone with 3 or 4 patients waiting outside while i was performing a code by myself which wasnt effective, here i had this first episode where i felt so alone, so sad, for me and for this people which deposit their trust in their healthcare system but at the same time questioning how fucked this was.. i actually made a song in my guitar for this that day. Some other guy menaced me with a gun on crystal meth because he was jealous that his wife went to the clinic, as soon as i went to the clinic, closed everything and got into my room, put key and didnt open the door until the morning, people buzzed the bell for attention but i didt open all night. I was scared. I started to sleep a lot, most of the time wasnt working i was asleep. Felt tired most of the time, and as the year progressed i was quickly getting tired of practicing, joy faded away slowly. As my social service advanced to its end, i just wanted to finish. I once saw 73 patients in a 18 hr shift.. assembly line medicine for good. I wouldnt smile anymore, i would sometimes feel angry because of so many ill people, i did my best there, lots of poverty, insecurity, drugs, narc etc. But as i finished i remember thinking, “im done with this shithole”, so i moved back to my town wheb my license got released. Had a couple of jobs and raised some money, went to spain and somehow i got a great job at the e.r. for 2 years, over there i experienced the best and the worst, i wanted to marry my gf so i worked real hard to save money, 2 x 24 shifts a week plus 1x 12 and 1 x 6hrs, i lived alone and started to excercise,play drums in a band, started drinking and smoking pot again. Suddenly i couldnt get some sleep without pot, shifts where endless, and then one day i snaped at a nurse because she was laughing in the shock room while cpr, and felt like crap with myself. As i drove back to my house, i felt so sad inside everytime i finished a shift, this really weird feeling of loneliness, melancholy, uselessness dont know how to describe. Money was good but i wasnt, got seriously sick in which i had a rectal bleeding out of nowhere, lost a lot of weight, smoked a lot of pot and hashish, and was always cranky, started having issues with my gf. Contract finished and they wouldnt hire me back, so i was unemployed for 4 months, my gf and i managed to survive with savings until next job, we were recently married and that year was the worst.we argued a lot, she was constantly sad too. Started new job at another e.r. in which i felt even more anxious, people was nice and all but i just couldnt manage shifts so long, i couldnt focus, started to feel really anxious with difficult patients, specially the “red” ones (triage), ive felt i knew shit about medicine, and that i might kill someone for not knowing what to do, this went on until one day, i told my wife we should go back to our country, she got so happy to hear me say that that i worked for a month and resigned.. here in mexico got worst, i was even more angry because work here is underpayed, and a lot more work, didnt sleep well, lots of pot and alcohol, i started to use psychedelics tryng to “understand” why i felt so angry, empty..what happened was that i had an affair with a friend when my partner was on a trip. She caught me because of msgs in facebook and confronted me, i got divorced. As everything turned around, i lost all interest in working, i still practice and really love to be helpfull to others, i give my best to patients, but right now, i see this jobs we can reach and its just plain slavery, i dont work for any gvmnt hospital or institution, just private clinics, but the follow same schemes, same staff etc. Its a joke to be a m.d. here in mexico. Right now in this moment i feel so tired with myself and guilty of my decisions, that i think im about to meltdown soon. Ive been using coke, modafinil, caffeine, pot, ritalin, mdma, lsd.. you name it. I dont do opioids, or benzos. Ive had suicidal thoughts but never went with them just feeling so tired and sad that you wish you where dead. Ive never been treated by the way. Hope some feedback, i really want to just leave all this shit behind.
Hi!
I am male married to female medical doctor.
Usually it is opposite – male is medical doctor and female is not.
Just my observation!
We are together 37 years.
We raised a two boys and both of them decided to follow my wife steps – one is already MD and younger one is studding to be a MD.
It was a long journey to come to this point in our life and to achieve relatively success in their and mine ( I am a part of that) carrier and life.
I will stop about introducing you with my family and will step to a problem which is “killing” me and bringing me to “unknown land” called: “Physician Burnout”!
All of them: my wife, MD resident son and younger one who is studding medicine are part of that unknown territory. I want to be optimistic about boys and their youth and energy that they still poses.
But I am not shore that I can say such thing for my wife. In her case I am very pessimistic.
I am loosing her…MD profession is taking my wife from me!
MD profession is taking my wife from our kids.
MD profession took my wife from our friends.
MD profession took her soul.
…and more and more from her patients – I am guessing looking what is happening with us as a family.
We used to be very strong and united like “musketeers”.
Indirectly I can see that she is abused by members of her administration and by a new “computer” regulation. I would like to say that there is no human approach to this profession anymore.
Medical Doctor wellness become a most sporadic element in “business” called a Health Care!
My wife became a typist and she is very bad in that.
You know all that charts has to be finish on time and there is no money for typist to be paid so that job is dedicated in hands of physicians. Well, everybody thinks that they are very “intelligent” for everything – which is a very wrong perceptions.
She is NOT good typist and she is telling that to everyone.
She hates computers and all different “programs” for charts at every new place where she works.
But I can tell you that my wife is a GOOD doctor and as a GOOD doctor she was reworded so many times.
Rewords are not coming anymore!
It is a past tense in her life.
Not just for her!
And because of all of that said my mind is going further and further to that “unknown land” called Physician Burnout.
Recently I found a very sad and tragic story about very successful MD ( R. C.) who committed suicide.
So, I found all symptoms what she was showing to members of her family and her colleagues in my wife.
My wife is becoming “VERY ISOLATED” like doctor who finished her life so tragically.
For R.C isolation started to be way of life at the close end of her existence.
I just can say I am completely lost not knowing what to do!
I am very week not knowing with whom to share this problem!
I think just MD’s can understand what I am talking about.
Just MD’s in USA!
Please, help me to HELP my wife and to bring her back to her “beautiful profession”.
Please, help me to take her for “unknown land”- PHYSICIAN BURNOUT!
Help!
She does not have “burnout” – she is being abused in an unsustainable and toxic medical workplace. Please contact me here:
Physician burnout is the latest trend among doctors. There are books, workshops, even special breathing exercises for physician burnout. Suddenly every other doctor I meet has burnout. And half of all med students have burnout before they graduate! WTF.
We enter medicine as inspired, intelligent, compassionate humanitarians. Soon we’re cynical and exhausted. How did all these amazing people get so screwed up so fast? ATTENTION medical students and doctors: It’s NOT your fault.
Burnout is physical and mental collapse caused by overwork.
So why are we blaming the victims?
The fact is medical students and physicians are collapsing because they are suffering from acute on chronic abuse. At some medical schools, 100% of students report abuse.
More here on the burnout lie.
I’ve been through some things as well. I am a general doctor from Central America, and things are pretty much the same here. I really loved this article and it is a serious issue. I wish there was something I could do to help! All I can do is pray for all of us doctors as a community, I hope we can all overcome this.
Depression is real and far more common than what we think. The data are given by WHO is harrowing; there is one suicide attempt in every three seconds and one death in every 40 seconds globally. This is just the tip of the iceberg because the statistics are based only on the reported cases. The number of actual cases may go as high as 20 times the number of reported ones. With depression being the most misunderstood areas of medical science, getting help or even asking for mental health care is taboo.
wow i didn’t know this was so huge, but these people emotionally crippled at work also have crippling debts…the otherv side of the white coat story’
hurt people hurt people, especially if they are on adrenergic stimulants and being bullied
i started temazepam to sleep after 36hr caffeined emergency shifts, got deeply depressed..exhausted, sad, stressed, malnourished etc and was put on a SSRI roller coaster ride from 1993-2001 where i ended up in a effexor induced suicidal psychosis
What is the free Suicide hotline number?
541-345-2437
I’m a board certified OB/GYN, fellowship trained in Reproductive Endocrinology & Infertility, but currently working the medical equivalent of “odd jobs” (home health evaluations , etc) for almost no money. I can’t even pay my mortgage and have been relying on the generosity of my husband’s family to get by for a year now. I’ve struggled with depression since internship (probably before that, but that’s when I sought help). I have had so many work catastrophes that it would take hours to explain them all. I’m applying for hospital privileges so that I can be proctored to resume infertility medicine after a 3 year hiatus, but I’ve already been turned down by one hospital and I’m terrified that I’ll be turned down again. I’m on multiple meds for depression, anxiety and idiopathic hypersomnia, but I can barely afford the $73 every two months to get refills and the $100 or so per month for meds. I literally can’t afford to let anyone know that I’m struggling because I can’t afford another office visit and a hospitalization would ruin any future chances of hospital privileges. (I was hospitalized in 2010 and 2011 when I was in the military. Thankfully the application I just completed only asked about hospitalizations in the past 5 years.) My 13 year old son also struggles with depression and anxiety, which breaks my heart. I hate that I can’t support my family properly. I just want to go to work each day and be able to have a financial cushion, be able to buy the kids presents for birthdays and holidays without financial panic. And yeah, I’m pissed that my “Chanukah gift” this year was the tire I had to buy last week when I got a flat. I want a little treat, or a word of appreciation, or just someone to say “good work”. I feel like an utter failure.
Email me here your address & phone number (and cut & paste the above). I have some ideas for you: https://www.idealmedicalcare.org/contact/
Physicians have no civil rights. We are simply subjects of the Totalitarian Administrative State, the harbinger of which are licensing boards. No one elects them. No one can legally get rid of them. And they do not have to answer, beyond mere lip service, to the public or the lawmakers. Anyone telling their children to work and study hard to become a physician are merely deluding themselves that the American Dream is alive and well under these circumstances.
I’m a second-year medical student, a year removed from turning 40 and married. No kids yet. This whole process has been exhausting, and even moreso this year with the topics we covered and now, prep for boards. I slowly made the switch from my first career to a pursuit of medicine roughly 10 years ago. A couple of times I wanted to quit the process…even dropped out of my pre-med classes one semester…only to return again. Was I doing it because I wanted to really go this path or just not be seen as a quitter? I don’t know. Fast forward to now, sitting at $265,000 in loan debt between my undergrad years, pre-med/grad years, and first two years of medical school, I feel stuck. No job will pay back those loans before I turn 70, if at all. The irony of me wanting to pursue medicine is I’m not a big fan of medications having seem the polypharm that is rampant. I’m more into preventing and/or fixing, not management and juggling a bunch of meds. If anything, surgery seemed right for me and ortho surgery is the only field I wanted to pursue since before being admitted to med school(I have a background that would support this desire). Seeing that highly competitive scores are a must to even be considered for ortho, I feel my stress has compounded during this board prep period, to the point I’ve become apathetic to class and board studies over the past few days. Along with that, I don’t feel joy in my life. I don’t feel happy or fun. I’ve also carried this thanatophobia for some time since my first grandparent passed 15 years ago…not that I’m afraid of dying if I walk into a street or I’m going to have a heart attack…but just the general fear that I’ve lived almost half my life now and feel I’m not anywhere at the level of happiness I’d hope to be.And, all I see is that one day I’m going to die and there’s nothing I can do about it. That part, takes the joy out of it all as well. I mean 20 years since high-school graduation has gone soooo fast. I’m afraid of the next 20 years going even faster and being in a darker point in life with regret, bitterness, loneliness, and so on.
Please contact me here and let’s talk. I’ve got some great ideas for ya.
Hi RL, I’m in a similar boat. I’m in the application process for medical school as a second career. If accepted this cycle, I’ll be 36 when I start. I completely empathize with this feeling of fear and anxiety around living half my life and not seeing ANY light at the end of the tunnel. I don’t know if medicine will fix my hatred of my current career. I don’t know if I’ll ever be able to make a contribution, to find happiness, to feel satisfied. I just see nothing but running the rat race until I get dementia, die, or both.
I really like your blog. Most likely, depression is caused by a combination of genetic, biological, environmental, and psychological factors. This is really a thing to think about that do depressed doctors go to doctors? Thanks for sharing your views.
I leave work and I go home, I don’t normally talk to anyone. I don’t want to – no-one will relate. Not even my family. Once a very social person, I’m now a hermit. Sometimes I get the energy to run along the promenade, and sit afterwards, staring at the sea. Sometimes it makes me feel better, but other times it makes me realize the pointlessness of everything. The waves just keep crashing. Non-stop. Forever and ever. When I’m gone, those waves will keep crashing. I’ve lost so many friends through this process. I often dream of having an MI or getting TB, that way I could get some time off. Anything to just get away for a bit
I’m so sorry you feel this way. I get it though. Have you sought help?
I left the medical profession just over three years ago. In hindsight, I’d been depressed long before I became a medical student, perhaps as a result of genetics (my mother and grandmother have also both been depression sufferers, perhaps because of childhood near-death experiences, or perhaps as a result of trauma resulting from domestic violence and psychological abuse from my alcoholic father towards my mother and myself. Likely a combination of all those factors.
However, in spite of all of this, the year before I was enrolled in med school, I was a confident, albeit somewhat emotionally repressed young man. I think people who go into medicine are usually very good at hiding how much they’re struggling even from ourselves.
Anyway, it wasn’t until my third year that the pressure started to take its toll on my health and performance and I noticed my grades slipping. I started doing intense workouts at the gym, eating whole foods, cycling as my main means of transport, practicing mindfulness meditation. Not all of my coping mechanisms were healthy, mind you. I also started drinking alcohol more often, and developed a taste for hard spirits.
I didn’t actually seek help for my depressive symptoms until my final year, by which point, I’d already almost failed some of my practicals due to symptoms of anxiety interfering with my ability to study and perform effectively. In hindsight, I should have addressed it sooner, going on an SSRI did a very good job at keeping the anxiety under control and improving my exam performance and I probably wouldn’t have graduated without them. Nevertheless, the gnawing psychological pain was telling me something wasn’t right. I was going into a profession that takes its toll on everyone, and the level of passion I had for the profession was too low to make it worthwhile.
Tragically, within two years of graduating, I lost two of my colleagues, out of a cohort of about 40 doctors at my hospital who graduated in 2014, to suicide. I came close to becoming a third, however, a therapist working with the occupational health service at that hospital reached out to us at exactly the right time, when I was seriously planning my own death.
After a severe breakdown in my mental health, I lost the ability to function intellectually at the level I was able to before. I decided that the medical profession was not right for me. Thankfully, not being from the USA, I didn’t have a huge student debt to pay off, just a low interest government loan – more of a graduate tax that only kicks in when you’re earning above a certain threshold.
I often feel weak because I had to give up the profession and career I worked 8 years of my life towards when so many other people had the strength and determination to stick it through. But reading some of what you’ve written makes me realise that I’m not alone. Two of my brightest and most studious colleagues at medical school also dropped out for similar reasons – the system is churning up some of the most intelligent and caring people, and spitting them out when they don’t keep up.
I still frequently struggle with dark thoughts from time to time, but I’m off psychiatric medication and I’m in a much better place than I was before. I hope to re-train as a counsellor or psychotherapist so as to help people in similar situations, and so that all my years of studying the human condition can still be put to some use.
I’m an NP but feel like so many of these experiences mirror my own. I’ve had depression since high school but anxiety started in nursing school, and has tagged along with me through my NP program and then my DNP program. My first NP job I worked 60-80 hours a week, was overcome with family stress dealing with in-laws and a husband (college sweetheart) who became completely unsupportive both emotionally and financially. I had an affair, got a divorce after 11 years together, I dropped out of my DNP program, and moved across the country to live with the man I had the affair with…who decided before I got there that I wasn’t what he wanted, after all. I became sexually promiscuous, spent my free time Googling the least painful ways to commit suicide, attended counseling which was somewhat helpful, added Wellbutrin to the Lexapro I’d already been taking for years. I met my now-husband, got offered what I thought was too good of a job to turn down in Michigan, tried to start a family, re-enrolled in my doctorate program. Got there and the job was a bait-and-switch. Paper charting, understaffed, no e-prescribing, but still expected to see the same amount of patient volume as clinics who did have those resources… I tried to stick it out for 2 years and just walked away last month when it became clear the suits and I would never, ever see eye-to-eye. Unfortunately, I needed to hire an attorney but that was the only way out. My husband has been dealing with unemployment for over 2 years as a result of his chronic medical conditions. He has committed bank fraud multiple times throughout our marriage in VERY misguided attempts to help make ends meet (a police officer actually showed up to my office during clinic) and I’ve caught him talking to other women online twice in the last year. We’ve struggled with male infertility for 3 years and I keep wondering what I’ve sacrificed my whole life for – I have nothing to show for it. I can’t afford a house since my student loan payments are so high. I might as well have not gone to college and had the kids I put off having so I could go to graduate school instead. At least I would be in my own house, and I wouldn’t have several hundred thousand dollars in student loan debt.
I am about to start my new job in two weeks and I’m paralyzed with anxiety. I can’t even go to the grocery store or the bank without having an anxiety attack and needing Xanax. I sleep 14-16 hours a day. I’ve struggled with both binge-eating and anorexia. I don’t want another divorce, I’m only 33. I function at my best when I’m connecting with my patients but I’m too scared to admit I can’t handle more than 30-35 hours a week of this line of work, or I mentally collapse and self-destruct. I look at accomplished providers around me who work 60+ hours a week and I feel weak and lazy in comparison, exactly the millennial stereotype I’ve tried so hard not to be. Instead of being excited about the new job opportunity, I’m fantasizing about suicide and almost drove my car into a river during a snow storm my last night in Michigan last month. I feel like I can’t even talk about this with a mental health professional or they’ll report me to the board. I’m not a danger to my patients, I’m a danger to myself. If they take my license and my livelihood, I’ll lose the only remaining reason I have any self-esteem.
I’m so sorry others are struggling also, but selfishly I’m thankful to know I’m not alone.
I am happy to talk to you. Contact me here
(I’ve been running a free suicide helpline for med students & doctors since 2012)
I was recently suspended from Medicare. Long story. The urgent care dropped me so fast without pay and now I can’t find work anywhere. I always had depression. On so many different meds through the years. I took adderall to get through the shifts because I was so miserable.
But now I’m home with three daughters, can’t pay student loans or mortgage. I cry myself to sleep and have no motivation whatsoever to pick myself up. I’m one month out from my last day of work and I feel like I am a useless failure. My whole identity was being a doctor and now I’m trying to collect unemployment. If they let me… getting a hard time there too. I’m divorced and my successful ex ( a psychiatrist) wants to hear nothing about it. Tells me I should just sell the house and live with my parents and he will take the kids. I feel alone, ashamed, sick all the time. I even started smoking which makes me hate myself more. I just need to keep it together for my daughters. But it feels like the world is against me…Especially when you are a doctor that screwed up. It’s an unforgiving world. I just don’t know if I will ever feel ok again. My mild depression in the past was manageable but this has just floored me and I can’t get up.
I’ll call you now. I have some great options for you. If you want to reach out to me I’m available 24/7 while awake here: https://www.idealmedicalcare.org/contact/
I’m not a physician (yet), but I work closely in the world. I’m a mental health clinician in a psychiatric hospital, who is in the application process for medical school. Mental health is just as bad, if not worse. At least physicians make living wages. I have a masters degree and I make 50k. Yet I hold people’s lives in my hands every day. I feel so much shame when I need to take a day off work, or if I feel burnout and need time to myself. I had a supervisor ask me once why I felt burnt out, and I told her I was experiencing financial hardship. She looked at me, perplexed, and asked why I didn’t just pick up more hours. I told her I didn’t feel fit to care for patients when burnt out. She asked what dosage of medications I was on. So inappropriate. Not only are we underpaid and overworked, we’re considered lowest of the low on the medical totem pole. Mental health is not appreciated, and as a masters level clinician I get talked down by psychiatrists all day long and treated like I don’t know my stuff. And just like many of the stories above, especially as someone working in mental health, there is NOWHERE to turn for help. I would love to admit myself to inpatient for a few days or acute residential treatment for a few weeks. But that would be 100% career suicide. No one wants to see a therapist who has been suicidal and been admitted to the loony bin. I’ve quit so many jobs without notice because I couldn’t stand it anymore, and I’ve burned so many bridges. As fucked as it sounds, I want to go to med school to wipe the slate clean and start over. My career in mental health is already so damaged. But if my suicidal ideation was to ever show up on my record, do you think medical schools would admit me? Of course not. I need to hide all of this until I’m through and out.
The need to support doctors and address the mental health toll on the health workforce has never been greater. Vox spoke to more than two dozen colleagues, family members, and friends of physicians who died by or attempted suicide, as well as physicians who attempted or contemplated suicide. They said the pandemic has laid bare an inhumane health system that sacrifices the mental health of the medical workers who keep it going. They also spoke of a mental health crisis in medicine that long predates the arrival of the coronavirus — one that could worsen in the pandemic’s aftermath. One warning sign of the disproportionate stresses on health workers over the past year and a half emerged in April 2020, when a New York City emergency room physician, Lorna Breen, died by suicide. Her family still doesn’t know who alerted the press, but Breen’s story was made public without their consent. “Once it was out there we decided to lean into the conversation, to tell the world what happened, because we believe Lorna’s death could have been avoided,” her brother-in-law, Corey Feist, told Vox. “The more we told the story, the more we heard from others throughout the country, and the world, who had similar experiences.”